Becoming a Bench Top Clinician
Looking beyond the technical for better esthetic results.
By Joshua Polansky, BA, MDC
It is no secret that the single central is among the most difficult dental restorations to create. Even with today’s improved materials, the single central incisor still poses problems for many dental technicians. Mimicking nature requires a mastery of form, color, material, and macro/micro nuances that will not create a visual dissonance in the final restoration. The technician who masters these elements in an ideal restorative situation supplied with proper information (quality photographs, accurate impressions, and bite registration) can rest on stable ground when fabricating the single match.
Rarely do we see “ideal” situations to restore. So the question becomes: How do technicians restore a single central in a less than ideal situation? The answer is that we need to broaden our knowledge to the clinical side of dentistry, going beyond the technical. With this knowledge we can help our clients achieve better clinical outcomes by becoming “bench-top clinicians.”
Case Study
The patient presented to the author’s clinic dissatisfied with a restoration recently placed by another clinic over an implant on tooth No. 9. He explained that he was greatly disappointed in the esthetic result and was concerned because the existing restoration did not match the shape and form of his natural teeth. He also reported that he was due to be married within 6 months, and he wanted his smile in his wedding album to reflect how happy he was on that day, rather than the unattractive smile he currently possessed. It was obvious that the patient’s smile could be improved with additional treatment (Figure 1).
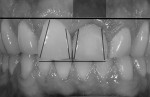
Intraoral photographs revealed details to help the dental team create a greatly enhanced restoration. The patient never mentioned a problem with the color of the restoration; his primary concerns centered on contour, form, and the disharmony created by the less than perfect restoration. Taking this into account, the color intraoral photographs were converted to black and white, which would allow the dental team to assess the patient’s concerns (Figure 2). The black-and-white image showed that the restoration did not have the same form as the patient’s natural dentition. Graying under the tissue from the metal abutment, an obvious tissue-level discrepancy, was also noted.
Technicians are inclined to look only at the model when restoring a case. However, to really achieve winning restorations, the patient’s entire oral environment—including the tissue, lip line, and smile—needs to be studied. It was evident when examining this patient’s lip line at full smile that the tissue-level discrepancy had to be addressed in order to reach an ideal outcome (Figure 3). Using photography to communicate the team’s concerns aided in educating the patient. After being shown the intraoral images, the patient agreed with the dental team that in order to fully restore his situation, not only did the form of the restoration need to be reworked, but the form of the surrounding tissue also needed to be corrected. Once enlightened, the patient was ready to proceed with the necessary treatment (Figure 4).
After the patient accepted the plan, the first step was to identify the type of implant placed. To obtain the necessary parts, the surgeon who placed the implant was called. The clinician removed the old restoration and observed the form of the surrounding tissue. It was very clear that the tissue-level discrepancy needed to be modified for an optimal case outcome (Figure 5). To save time and extra expense, the clinician was very careful when removing the old restoration so that the existing implant abutment could be salvaged (Figure 6). If necessary, a temporary abutment was available for placement.
With the old abutment and a soft-tissue impression of the existing situation, the technician could now go to the bench and, using a scalpel, contour the tissue on the model to ideal contours (Figure 7). The technician used the old abutment to recontour the sulcus area to a new ideal situation. This was done by priming the old abutment using GC Metal Primer 11 (GC America, www.gcamerica.com) and adhering composite (GC Gradia) to the abutment to create the optimal sulcus contour (Figure 8). Once the tissue and sulcus modifications were completed on the model, the technician could now fabricate an esthetic temporary as well as build the tissue simulation (Figure 9). An esthetic temporary was fabricated using Anaxdent New Outline acrylic (www.anaxdent.com) with a highly polished custom temporary abutment (Figure 10).
The bench-top work completed by the technician could now be transferred to the patient’s mouth. The clinician placed the new temporary abutment in the mouth and marked the tissue contours for cut-back (Figure 11). The tissue was contoured using a DEKA CO2 soft-tissue laser (DEKA Laser Technologies, Inc., www.dekalasers.com). Once contoured, it became clear that the highly polished composite margin was ideally placed (Figure 12). The clinician used temporary cement to secure the provisional restoration in place and begin the tissue-healing phase of the treatment (Figure 13). The patient returned a week later for a clinical monitoring of tissue progress. For the dental team, it was important to observe not only that the tissue was healing nicely, but also that the form and color of the temporary matched the patient’s expectations of the final case outcome (Figure 14). The team wanted to be sure it was headed in the right direction in terms of form, value, and tissue height (Figure 15) because this information would directly translate to the final restoration.
Creating the Final Restoration
Confident that the patient’s expectations had been met, the clinician took the final impression at the next appointment. The current sulcus diameter that was achieved with the new temporary was used to transfer the patient’s new situation. This was accomplished by placing the transfer coping back on to the model and filling the sulcus with Pattern-resin (GC America, www.gcamerica.com) (Figure 16 and Figure 17). This technique allowed for an exact pick-up of the patient’s new condition. All of these details were extremely important for creating the design for a patient-specific custom ceramic abutment. A zirconia ceramic custom abutment would not only help the dental team achieve a good biologic environment, but it would also help the contour of the final restoration as well. The final outcome of the case was based completely on the temporary abutment and the temporary restoration (Figure 18). The model was shipped to Atlantis (www.astratechdental.com) for the CAM-milled ceramic abutment. The abutment design was based on the contour of the temporary to guarantee the proper dimensions needed for layering ceramics (Figure 19). The abutment design presented to the dental team by Atlantis was meticulously inspected prior to the milling process to ensure that there was adequate space for layering ceramics based on the design of the temporary and to check the functional aspects of the case as well (Figure 20).
When the milled ceramic abutment was returned, the team checked it against the design specifications (Figure 21). It was critical that the abutment not only possessed the desired room for occlusion and ceramics, but that the sulcus was developed as planned (Figure 22, Figure 23, Figure 24). With all these details checked, the technician could now begin the final layering stage. Although much care and energy had gone into tooth form and tissue development, it was critical that in order to go to the final stages of layering, an accurate shade image be taken to achieve a successful outcome. To determine the final shade, a value shade was obtained and custom shade tabs were used to visualize the final restoration (Figure 25 and Figure 26).
When fabricating a single central, the devil is truly in the details. If we look at the principles outlined in Ludwig Rinn’s book, The Polychromatic Build Up Technique (Quintessence Publishing, www.quintessence.com), it is clear that each ceramic layer is critical to the final outcome.1 Often the core, opaque, or bonder layer is overlooked by technicians in the ceramic build-up phase. However, this layer is extremely important because it allows natural light to scatter and reflect, helping to give the restoration a more vital appearance. For this case, light reflective liners were applied to the frame modifiers (GC America Zirconia light reflective liner kit). To achieve a nice foundation, GC Initial ZR base layer L-2 was used for the cervical portion of the coping as well as for highlights on the interproximals and where the mamelon structures would appear. The remainder of the coping was coated with GC Initial L-BL (Figure 27).
With the base layer placed, polychromatic ceramic layering was begun always following the principles of nature (Figure 28 and Figure 29). Although the proposed restoration was a basic A1 shade, a deep understanding of a segmental ceramic layering technique should be understood. The layers of deep dentins, modifiers, enamels, translucence, and opalescent ceramics are catalysts for the diffusion, transmission, and scattering of light that will allow for a life-like restoration. Figure 30 shows the segmental layering for the proposed restoration. Note the multiple layers of dentins, effects, and opals used to achieve the final result. Once the ceramic layering was complete, the crown was tried in for final analysis (Figure 31). For this analysis, the team looked at the overall natural harmony of the restoration, shade, shape, and value (Figure 32). At this stage of final treatment, we also observed the results of our efforts to achieve optimal tissue reaction (Figure 33 and Figure 34).
The crown was temporarily cemented in place so that the patient could wear it for a week or two to ensure no other adjustments or corrections were needed before final cementation. At the final appointment, the patient had one request for an adjustment. He said that from different angles the mesial aspect was a hair short and he wanted it to be more even (Figure 35). This is the reason that we always temporarily cement before the final cementation, to be sure that the patient is happy with our efforts before going to a final. Using low-fusing add-on powder from the GC Initial Zirconia kit, the technician added a small addition to the mesial aspect of the restoration to even the mesial–incisal edge (Figure 36). While we always want to improve our patients’ overall smile, we also have to consider the appearance of the restoration with other facial expressions, such as lips at rest (Figure 37). Once all the details of this case came together, the satisfied patient felt confident with his new smile (Figure 38). Even though this case was only a single central incisor, a great deal of thought and consideration was necessary to achieve successful treatment and a life-like final outcome (Figure 39, Figure 40, Figure 41).
References
1. Rinn, Ludwig. The Polychromatic Layering Technique: A Practice Manual for Ceramics and Acrylic Resins. Quintessence Pub. Co., 1990.
About the Author
Joshua Polansky, BA, MDC
Owner
Niche Dental Studio
Cherry Hill, New Jersey