Short Implants: a Viable Treatment Option in the “Anatomically Challenged” Patient
Michael Toffler, DDS
Patients with fully or partially edentulous alveolar ridges comprised of markedly reduced bone volume must accept the higher risk of complication, extended treatment duration, and heavier financial burden associated with their implant-supported rehabilitation.1 The clinical challenge is exacerbated by post-extraction ridge resorption and increased pneumatization of the maxillary sinus often creating proximity to both the inferior alveolar nerve and antral floor. This reduced residual bone volume frequently prohibits the placement of implants 10 mm in length or longer without invoking ridge augmentation,2,3 sinus floor elevation,4-6 alveolar osseosdistraction,7 or nerve transpositioning8 procedures. As a less invasive alternative, the placement of short implants (9 mm or less) often minimizes or obviates the need for more extensive surgery, reducing treatment duration, morbidity, and associated costs. In this article, five cases are presented that clearly demonstrate the clinical and practical benefits of using short implants in the atrophic alveolus.
In the deficient posterior maxilla, a variety of sinus floor elevation techniques have been successfully implemented using different graft materials in a delayed or simultaneous approach to implant placement.4-6,9-14 The lateral window osteo-tomy is the most commonly used and reported technique for sinus augmentation,5,6,9-11 but it does have some disadvantages including increased cost, increased morbidity, risk of serious infection, and delayed healing times.15 As a less invasive alternative, osteotome techniques1,6,12-14,16 can obtain a localized elevation of the sinus floor through a 3-mm to 6-mm diameter crestal osteotomy, minimizing the degree of flap elevation and thus eliminating the need for preparation of a larger bony window in the lateral aspect of the alveolus. An osteotome-mediated approach offers the advantages of a more conservative surgical entry, more localized augmentation of the sinus, a lesser degree of postoperative morbidity, and an ability to load the implants in a shorter time period.17 When there is adequate subantral bone for primary stabilization of implants, osteotome-mediated sinus floor elevation (OMSFE) procedures procure 2 mm to 7 mm of localized sinus floor elevation, usually permitting the simultaneous placement of implants 10 mm in length.18-21 Studies by Toffler18 and Rosen et al19 found a significantly reduced survival rate of 73.3% and 85.7%, respectively, when the residual subantral bone height (RSBH) was 4 mm or less. Based on these studies, it would seem that in the more severely resorbed posterior maxilla (< 5 mm RSBH), minimally invasive OMSFE with simultaneous implant placement is not the treatment of choice and a staged approach using a lateral window technique9-11 or crestal core approach6,13,14,16 would be preferred. However, the recently reported success with short implants with a variety of roughened surfaces22-28 may transcend these boundaries, requiring less RSBH as well as minimal sinus floor elevation to achieve successful long-term results. Similarly, the inherent risk of nerve lateralization8 and the extreme challenge of vertical ridge augmentation2,3,7,29 may be avoided by using short implants in the atrophic posterior mandible.
The following case reports clearly demonstrate the clinical and practical benefits of using short implants in the deficient alveolus where the residual bone volume is significantly diminished, resulting in proximity to the nasal floor, sinus floor, or inferior alveolar nerve (IAN).
Clinical Reports
Case 1
An 88-year-old man who was taking warfarin, doxazosin, digoxin, hydrochlorothiazide, and metoprolol to control atrial fibrillation and high blood pressure presented with a failing maxillary right posterior prosthesis (Figure 1) and missing posterior teeth in the left maxilla (Figure 2). He desperately wanted to avoid wearing a removable prosthesis and was anxious to expedite implant treatment, avoiding more invasive staged procedures as these would prolong treatment, impose a greater risk for complication, and would likely require modification of his warfarin intake. The morning of the first surgical appointment, the patient’s international normalized ratio (for anticoagulant monitoring) was 2.2, low enough for the author to proceed with the intended treatment. At site Nos. 13 and 14, 4 mm to 6 mm of subantral bone was present. OMSFE allowed for the placement of 8-mm long, single-stage implants at site Nos. 13 and 14 and a 10-mm long single-stage implant at site No. 12 (Figure 3). Four weeks later, in the upper right quadrant, tooth Nos. 2 and 4 were extracted. A 10-mm implant was placed immediately at site No. 4 in combination with OMSFE, along with a 12-mm implant at site No. 5. Using OMSFE, a 6-mm long, wide-diameter implant was placed in 3 mm of RSBH at site No. 3 (Figure 4). After 3.5 and 4.5 months of healing, splinted implant-supported restorations were cemented in place in the upper right and upper left quadrants, respectively (Figure 5 and Figure 6). This minimally invasive approach reduced surgical trauma and expedited treatment in this “anatomically challenged,” elderly patient.
Case 2
A 52-year-old woman had recently lost teeth Nos. 28 and 30 to periodontal and endodontic infection. Significant bone resorption had taken place and the dental scan revealed only 8 mm of bone superior to the IAN at site Nos. 29 and 30 (Figure 7). The patient was advised that an implant-supported prosthesis would not be possible without staged vertical and horizontal ridge augmentation. She was also informed of the risk of a long-span fixed prosthesis supported by a compromised second molar abutment. As a less invasive alternative, avoiding advanced augmentation procedures, short implants 3.5 mm to 4 mm in diameter and 7 mm to 9 mm in length were placed at site Nos. 28 through 30 (Figure 8) and restored with a screw-retained prosthesis 4.5 months later (Figure 9 and Figure 10).
Case 3
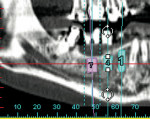
A 48-year-old woman had lost tooth No. 18 to extensive caries 5 months prior to presentation. She retained the opposing maxillary second molar. The patient had previously been advised that there was inadequate bone volume superior to the IAN to predictably replace missing tooth No. 18 with an implant-supported restoration (Figure 11). A dental scan revealed 8 mm of bone height superior to the IAN (Figure 12). A 4.5-mm x 7-mm implant was placed and restored 3.5 months later with a cemented restoration (Figure 13). Careful analysis of the existing anatomy and good remaining bone quality combined with an expertly contoured restoration provided this patient with predictable second molar replacement under adverse preoperative conditions.
Case 4
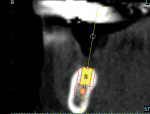
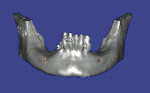
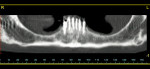
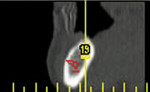
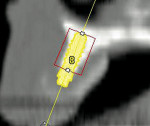
A 57-year-old woman presented with complaints of instability of her mandibular removable partial denture (RPD) and pain associated with her remaining mandibular teeth, Nos. 22 through 27. The patient had lost her posterior teeth 25 years earlier and, as a result, the posterior alveolus was severely atrophic (Figure 14 and Figure 15). At a consultation appointment with another surgeon several months earlier, it was suggested that iliac grafts were necessary to reconstruct her posterior mandible or, as an alternative, she should consider the extraction of her remaining teeth and insertion of implants at site Nos. 22 and 27 to support an overdenture. As the patient’s primary concern was improving the stability of her RPD and reducing the stress on her remaining teeth, the author considered posterior placement of short implants to aid in denture stabilization. Thorough analysis of the cross-sectional views of the dental scan revealed barely adequate bone volume at site Nos. 19, 21, and 28 (Figure 16; Figure 17; Figure 18). Implants measuring 3.5 mm x 7 mm were placed at site Nos. 21 and 28, and a 4.5-mm x 7-mm implant was placed at site No. 19. The implants were uncovered 3 months later and three attachments were placed to aid in partial denture retention (Figure 19; Figure 20; Figure 21). This less invasive treatment alternative not only reduced treatment time, morbidity, and cost, but also stabilized the mandibular prosthesis. The patient achieved improved function and reduced stress and discomfort associated with the anterior teeth.
Case 5
A 54-year-old woman presented with missing teeth Nos. 5 through 12, complaining of instability of her maxillary RPD. She had lost the anterior teeth in a motor vehicle accident 15 years earlier, and the remaining ridge was severely atrophic. An advanced degree of bone loss was also noted around tooth Nos. 2, 3, and 15 (Figure 22). She sought a second opinion after being advised that she required iliac grafts in the anterior maxilla, extraction of teeth Nos. 2 and 3, and sinus augmentation to stabilize the RPD or allow for placement of a fixed implant-supported prosthesis. The dental scan revealed a small “island” of bone at site Nos. 8 and 9 (Figure 23) where 3.3-mm x 8-mm implants were placed with a minor nasal floor lift (Figure 24 and Figure 25). Six months after placement, abutments were attached to the implants (Figure 26), stabilizing the prosthesis (Figure 27 and Figure 28) and reducing stress on the remaining teeth. This minimally invasive approach, using strategically placed short implants, adequately addressed the patient’s chief complaint and avoided hospitalization and a prolonged staged treatment.
Discussion
Ideally, implant treatment must be cost-effective, short in duration, simple in procedure, and highly predictable.22 The ability to achieve long-term success with all implants is intrinsically related to the amount of surface area of the implant contacted to bone.30 The quality of the bone–implant interface encompasses multiple factors, including bone quality and the length, diameter, surface properties, shape, and design of the implant.31 The addition of a roughened surface texture to machined threads is known to enhance overall clinical performance, especially in areas of reduced bone density such as that found in the posterior maxilla.32 It is believed that the surface irregularities ensure a firm contact with the blood clot allowing primitive cells to migrate to the interface, differentiate to osteoblasts, and form bone directly on the surface.33 Modifications of the implant surface features, such as etching, blasting, and increasing porosity, improve the retention between the implant and the bone by enlarging the contact surface area, thus increasing the biomechanical interlocking between implant and bone.32,34 These enhanced osseoconductive surfaces increase the bone-to-implant contact, effectively reducing the length of the implant previously necessary to successfully function under occlusal load generated in the posterior alveolus. The improved bone-to-implant contact in the minimal residual bone along with preservation of the remaining bone in the crestal cortical passage allows the successful long-term function of a short implant with a significantly increased crown-to-implant ratio.
The clinical application of short implants in the deficient alveolus serves to minimize or eliminate the need for vertical ridge augmentation, nerve transposition, and extensive sinus floor elevation. These advantages reduce procedural morbidity and treatment duration, as evidenced by the case reports presented where short implants were placed without ridge augmentation and only minimal sinus or nasal floor intrusion. Short implants are an especially valuable treatment alternative in a growing geriatric patient population that is not only notoriously undertreated, but also reluctant to undergo prolonged and invasive implant rehabilitation. The strategic placement of short implants in the anatomically and often medically compromised elderly patient effectively enhances oral function, comfort, and quality of life, in a more conservative, timely, and patient-friendly manner. When the patient’s medical, emotional, or financial status precludes prolonged, more invasive, and costly site development procedures, the clinician should consider short implants as a viable treatment option.
Conclusion
If dentists ultimately desire to successfully treat implant patients through the most conservative means possible while minimizing treatment duration, costs, and trauma, then the use of short implants in combination with minimally invasive augmentation procedures where necessary would make great strides toward the achievement of this lofty goal. This approach has been eagerly accepted and successfully applied in the author’s clinical practice, broadening the referral base and increasing implant availability for even the most reluctant dentists and patients.
Acknowledgments
The author would like to thank surgical assistants Tracey Lindsay, Gricel Crespo, Opal Lumbsden, and Andrea Arroyo for their constant support, encouragement, and patience.
References
1. Toffler M. Treating the atrophic posterior maxilla by combining short implants with minimally invasive osteotome procedures. Pract Proced Aesthet Dent. 2006;18(5):301-308.
2. Jacotti M. Simplified onlay grafting with a 3-dimensional block technique: A technical note. Int J Oral Maxillofac Implants. 2006;21(4):635-639.
3. Simion M, Trisi P, Piatelli A. Vertical ridge augmentation using a membrane technique associated with osseointegrated implants. Int J Periodontics Restorative Dent. 1994;14(6):496-511.
4. Raghoebar GM, Timmenga NM, Reintsema H, et al. Maxillary bone grafting for insertion of endosseous implants: results after 12-124 months. Clin Oral Implants Res. 2001;12(3):279-286.
5. Wallace SS, Froum SJ. Effect of maxillary sinus augmentation on the survival of endosseous implants. A systematic review. Ann Periodontol. 2003;8(1): 328-343.
6. Toffler M. Staged sinus augmentation using a crestal core elevation procedure to minimize membrane perforation. Pract Proced Aesthet Dent. 2002;14(9):767-774.
7. Jensen OT, Laster Z. Preventing complications arising in distraction osteogenesis. J Oral Maxillofac Surg. 2002;60(10):1217-1218.
8. Ferrigno N, Laureti M, Finali S. Inferior alveolar nerve transposition in conjunction with implant placement. Int J Oral Maxillofac Implants. 2005;20(4):610-620.
9. ten Bruggenkate CM, van der Bergh JP. Maxillary sinus floor elevation: a valuable pre-prosthetic procedure. Periodontol 2000. 1998;17:176-182.
10. Smiler DG. The sinus lift graft: basic technique and variations. Pract Periodont Aesthet Dent. 1997;9(8):885-893.
11. Garg AK, Quiñones CR. Augmentation of the maxillary sinus: a surgical technique. Pract Periodont Aesthet Dent. 1997;9(2): 211-219.
12. Summers RB. The osteotome technique: part 3—less invasive methods for elevating the sinus floor. Compend Contin Educ Dent. 1994;15(6):698-710.
13. Toffler M. Site development in the posterior maxilla using osteocompression and apical alveolar displacement. Compend Cont Educ Dent. 2001;22(9):775-790.
14. Fugazzotto PA. Immediate implant placement following a modified trephine/osteotome approach: success rates of 116 implants to 4 years in function. Int J Oral Maxillofac Implants. 2002;17(1):113-120.
15. Regev E, Smith RA, Perrot DH, et al. Maxillary sinus complications related to endosseous implants. Int J Oral Maxillofac Implants. 1995;10(4):451-461.
16. Toffler M. Minimally invasive sinus floor elevation procedures for simultaneous and staged implant placement. N Y State Dent J. 2004;70(8):38-44.
17. Fugazzotto P. Augmentation of the posterior maxilla: A proposed hierarchy of treatment selection [published erratum appears in: J Periodontol. 2004;75(5):780]. J Periodontol. 2003;74(11):1682-1691.
18. Toffler M. Osteotome-mediated sinus floor elevation: a clinical report. Int J Oral Maxillofac Implants. 2004;19(2):266-273.
19. Rosen PS, Summers R, Mellado JR, et al. The bone-added osteotome sinus floor elevation technique: multicenter retrospective report of consecutively treated patients. Int J Oral Maxillofac Implants. 1999;14(6):853-858.
20. Nkenke E, Schlegel A, Schultze-Mosgau S, et al. The endoscopically controlled osteotome sinus floor elevation. A preliminary prospective study. Int J Oral Maxillofac Implants. 2002;17(4):557-566.
21. Cavicchia F, Bravi F, Petrelli G. Localized augmentation of the maxillary sinus floor through a coronal approach for the placement of implants. Int J Periodontics Restorative Dent. 2001;21(5):475-485.
22. ten Bruggenkate CM, Asikainen P, Foitzik C, et al. Short (6-mm) nonsubmerged dental implants: results of a multicenter clinical trial of 1 to 7 years. Int J Oral Maxillofac Implants. 1998;13(6):791-798.
23. Griffin TJ, Cheung WS. The use of short, wide implants in posterior areas with reduced bone height: a retrospective investigation. J Prosthet Dent. 2004;92(2): 139-144.
24. Renouard F, Nisand D. Short implants in the severely resorbed maxilla: A 2-year retrospective clinical study. Clin Implant Dent Relat Res. 2005;7(Supp 1): S104-S110.
25. Arlin ML. Short dental implants as a treatment option: results from an observational study in a single private practice. Int J Oral Maxillofac Implants. 2006;21(5):769-776.
26. Nedir R, Bischof M, Briaux J-M, et al. A 7-year life table analysis from a prospective study on ITI implants with special emphasis on the use of short implants. Results from a private practice. Clin Oral Implants Res. 2004;15(2):150-157.
27. Domingues das Neves F, Fones D, Bernardes SR, et al. Short implants—an analysis of longitudinal studies. Int J Oral Maxillofac Implants. 2006;21(1): 86-93.
28. Renouard F, Nisand D. Impact of implant length and diameter on survival rates. Clin Oral Implants Res. 2006;17(Suppl 2):35-51.
29. Stellingsma K, Bouma J, Stegenga B, et al. Satisfaction and psychosocial aspects of patients with an extremely resorbed mandible treated with implant-retained overdentures. A prospective, comparative study. Clin Oral Implants Res. 2003;14(2):166-172.
30. Cochran DL, Nummikoski PV, Higginbottom FL, et al. Evaluation of an endosseous titanium implant with a sandblasted and acid-etched surface in the canine mandible: radiographic results. Clin Oral Implant Res. 1996;7(3):240-252.
31. Tawil G. Peri-implant bone loss caused by occlusal overload: repair of peri-implant defect following correction of the traumatic occlusion. A case report. Int J Oral Maxillofac Implants. 2008;23(1):153-157.
32. Cochran DL. A comparison of endosseous dental implant surfaces. J Periodontol. 1999;70(12):1523-1539.
33. Davies JE. Understanding peri-implant endosseous healing. J Dent Educ. 2003;67(8):932-949.
34. Pillar RM. Overview of surface variability of metallic endosseous implants. Textured and porous surface-structured designs. Implant Dent. 1998;7(4): 305-314.
About the Author
Michael Toffler, DDS
Diplomate
American Board of Periodontology
Private Practice
New York, New York