Counterfeiting Epidemic
Product substitution and counterfeit materials hold serious consequences for the patient as well as dental professionals.
One of the most troubling trends in dentistry today is the free substitution of products by both foreign and domestic laboratories. Although, in the case of pirated name-brand products, China seems to be the most common offender—the global menace of counterfeit goods is increasing. The free flow of goods across the world, lack of regulation, and socio-economic conditions are the major factors impacting the sale of counterfeit goods. Coach® handbags, Rolex® watches, and Gucci® eyeglasses are sold at much higher quantities than the actual number of items produced by these manufacturers each year. The counterfeits look remarkably like the authentic products but move through an illegal distribution channel to the consumer. Not only does such counterfeiting activity cheapen these brands, it hurts the actual sales of their products and impacts the bottom line of these companies.
However troublesome the sale of counterfeit watches, handbags, and eyewear is, these products pose no health risk to the consumer. The effect could be much more serious when counterfeiting spreads to healthcare products. Currently, cases of counterfeited healthcare goods, such as medications and medical devices, are assuming critical proportions. The Organization for Economic Co-operation and Development (OECD) and the World Health Organization (WHO) estimate that approximately 6% to 8% of the total global medical devices market comprises counterfeit goods. This percentage does not consider unaudited and unaccounted markets where the problem might be more serious.
Dangerous Dental Products?
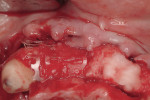
The dental industry is not immune from counterfeit products or from fraudulent material substitutions. The author recently spoke to a dentist who said he tried a BruxZir restoration and was not impressed with the material. This was not just surprising, but startling, because in every case the author has been involved in this product, the opposite reaction from clients has been true.
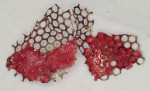
By investigating further, the author found that some laboratories are claiming to have a material “just like BruxZir” and then substituting conventional isostatically pressed and bound framework zirconia, which is not the same material formulation or manufacturing method used to produce BruxZir. The author has also been asked to make adjustments to an IPS e.max® crown fabricated by another laboratory, only to have it ruined in the oven on a regular firing cycle. The failure indicated the crown was fabricated using an ordinary pressed-ceramic material and not IPS e.max lithium disilicate. This could have been a case of material substitution or the purchase of a counterfeit material. Captek™ restorations have been counterfeited for years by substituting very high-noble alloys or gold plating for the real product. Neither produces the bacteriostatic effects that differentiate Captek from cast-metal substructures.
Not only is material substitution fraudulent, altering a doctor’s prescription is also illegal. A serious consequence of counterfeit materials and material substitution is that any resulting product failure cannot be accurately reported and traced because there is no proof that the failed product was in fact the material requested or from where the material originated. Manufacturers are realizing that mislabeled restorations or consumables and product substitution are a serious epidemic. companies such as 3M ESPE have instituted material authentication programs in an attempt to halt the use of counterfeit Lava™ products or the substitution of non-Lava zirconia for framework construction. Steps like these from the manufacturing community as well as the FDA will help crack down on such illegal activities and will continue to increase going forward.
Read more on how the gray market can directly aff ect you by logging onto: www.dentalaegis.com/go/idt11