Making the Right Selection
A strong foundation in restorative options is key in choosing the appropriate fabrication method and materials.
By Peter Pizzi, MDT, CDT, FNGS
Achieving successful outcomes in esthetic cases sometimes requires dental technicians to go slightly against the grain when choosing which restorative materials and fabrication methods they should use. They must carefully weigh the myriad material options in their toolbox, always basing their decisions on the quality of the end result for the patient—not which manufacturer made the product or the fastest way to get the job done. Having a strong foundation and extensive knowledge of the restorative materials is paramount. Otherwise, as the old saying goes, “If your only tool is a hammer, you tend to see every problem as a nail.”
A technician’s comfort level with a particular material or technique can influence the choices he makes. For example, in an anterior, esthetic-driven case (Figure 1), the technician would typically pick the material and technique he is most comfortable using. Although this case seems fairly straightforward, in reality, the material and technique options are endless. As with any case, all aspects should be evaluated before a standard material selection is made.
If porcelain-fused-to-metal is part of the technician’s comfort zone, then this case becomes a single PFM on tooth No. 8 and ceramic veneers on teeth Nos. 7, 9, and 10. However, the reflective index of metal compared to the natural light transmission of dentin and enamel challenges him to make metal-based and all-ceramic materials work together. So is that the best restorative option? There are occasions when a case requires the use of different substructure and overlay materials. Most technicians have likely fabricated cases like this, with results that range from high quality to poor (Figure 2).
An Educated Decision
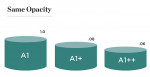
If a press-to-metal technique and press-to-metal materials are chosen, all four restorations could be fabricated using the same material and technique, eliminating the need to match different materials. However, the press-to-metal technique creates its own unique set of challenges. Press thickness plays a critical role in restoration-to-restoration density and how that density affects light transmission. There are also limitations in the pressability of each material (Figure 3). For tooth No. 8, the full-coverage crown would be much thicker than each of the veneers, changing the value base of each unit. In a perfect world, each restoration would be fabricated using materials with similar thicknesses, allowing each of the preparations to finish in the same spacial plane. Unfortunately, this is not always possible. Most often the tooth preparation, tooth position, and even decay or coloration of the underlying dentin or enamel dictates restoration thickness. A final factor impacting material selection depends on whether the practitioner chooses an adhesive technique (cementing) or a cohesive technique (bonding).
The challenge in this case became how to control ceramic depth with opacity and translucence through material selection. This is not to say that different materials can never be used next to each other—sometimes that is just not an option. But with a large toolbox of materials, a technician should be able to make an educated decision about what will work best in each situation, based on a few key factors:
• Functionality of the case; ie, the occlusal aspects
• Esthetic demands of the case; ie, color and light transmission
• Fabrication technique
Of these, the fabrication technique is the biggest challenge. If a technician is not comfortable using a particular material and technique, it will be more difficult to achieve the expected outcome. On the other hand, the case could also have a less than optimal outcome if the material chosen is not the right fit for the case—even if the fabrication method is.
When the author diagnostically evaluated this case, his first consideration was from a functional standpoint. Because this was primarily a veneer case, he had no control over the lingual aspects and only had to include tooth No. 8 in the anterior coupling. As a result, he was fairly free to choose almost any material to fabricate the case.
The next factor was the stump shade of each tooth and its effect on the final color. Would it be necessary to mask any aspects of the tooth or could the stump color be utilized in the final restoration? All stumps were in the A2 shade range, and the author was looking to achieve a final A1 finish.
The last consideration involved how much space there was for the veneering material. Ideally, the author wanted to press a dentin structure for tooth No. 8 using a highly opacified material. By using a cutback technique, he could slightly mask the dentin and yet create a core similar in value to the adjacent veneers (Figure 4 and Figure 5). That would allow him to layer over all four restorations using the same veneering material (Authentic®, Jensen Dental, www.jensendental.com). Once the core was pressed, the case then really became a four-unit veneer case. The next obstacle in the selection process was the CTE compatibility of the veneering material and the refractory die material. The author could choose to use the foil technique, but he likes working on a refractory tissue cast. Because he was using a press veneering ceramic, he ran a test of the ceramic on a mock refractory die before pressing the core (Figure 6).
Four-Unit Build-up
These are the steps the author used to layer the core and fabricate the veneers so he could achieve an optimal esthetic outcome. The refractory dies were seated in the cast, and the pressed core was placed in position on tooth No. 8 (Figure 7 and Figure 8). Dentin, enamels, and translucents were built to frame tooth shape and create the canvas upon which the other ceramic materials would be layered (Figure 9 and Figure 10). Mamelon and effect materials were used with a glaze medium for control over the canvas to help mask the transition between the opacity of the stump or ceramic core and the canvas translucency (Figure 11 and Figure 12). The materials were broken up with a brush tip to make light transmission more random (Figure 13).
White enamel (Authentic Pearl, Jensen Dental) was used as a band and feathered in over the mamelon effects to increase value and control the transition between the stump and canvas (Figure 14). Enamels and translucents were applied from 0.3 mm to 0.5 mm (cervical to incisal) to cover and filter the underlying effects (Figure 15). After a firing cycle, contacts were adjusted and the restorations were fit to the cast. The contour was evaluated with a wax pencil on the heights of contour (Figure 16). After the final restorations were glazed, polished, and de-vested, they were fit to the original dies (Figure 17 and Figure 18). The accuracy of the die cast plays a large role in the final fit of the restorations on the solid cast. When done right, it should be an easy transition (Figure 19). Under different lighting conditions, the light transmission of each material can be evaluated to ensure that they appear very similar (Figure 20 through Figure 22).
In this esthetic-driven market, the dental technician’s comfortability with different materials is key to achieving successful results and retaining clients. The challenge of learning about different systems and ceramics is difficult, but it empowers the technician so he can best serve the patient and can create a better esthetic outcome.
About the Author
Peter Pizzi, MDT, CDT, FNGS
Owner and Manager
Pizzi Dental Studio Inc
Staten Island, New York