Immediate Implant Placement and Provisionalization Following Partial Extraction Therapy
Virtual planning and 3D printing enable the design and fabrication of an esthetic provisional restoration prior to surgery
Rick Ferguson, DMD | Gregori M. Kurtzman, DDS
Immediate implant placement after extraction is often preferred due to the shortened treatment time, reduction of surgical procedures, and accelerated restoration of esthetics. However, various challenges can complicate treatment involving implants placed immediately after extraction, including those associated with planning and the delivery of immediate provisional restorations. These challenges are largely related to the design and fabrication time for surgical guides and provisional restorations, but recent technological advancements have helped to mitigate these issues.
Combining virtual planning that utilizes cone-beam computed tomography (CBCT) with the in-office design and printing of surgical guides can permit treatment to be rendered on the same day that a patient commits to it. In-office planning and 3D printing can enable the chairside design and fabrication of a screw-retained provisional crown in a 1-hour period following implant placement. After an intraoral scanner is used to acquire a digital impression of a titanium base or scan body seated on the implant, a provisional restoration can be designed and printed.
In the following case, virtual planning was utilized to produce a surgical guide and provisional restoration to facilitate single-visit immediate implant placement following partial extraction therapy (PET). PET was implemented to help preserve the patient's thin facial/buccal plate, which decreases the incidence of dehiscence during healing after implant placement.1,2 3D printing was implemented to enable rapid fabrication of the implant-supported provisional crown for same-day delivery.
Case Report
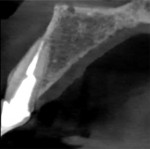
An 84-year-old male patient presented to the practice for an emergency appointment. He stated that a crown on one of his upper front teeth had come off and needed to be recemented. The patient's records indicated that the tooth (No. 7) had been endodontically treated and restored with a fiber post, core buildup, and crown more than 5 years prior to his current presentation. During the clinical examination, it was noted that the tooth had fractured supragingivally, leaving the core and a portion of the fiber post in the detached crown (Figure 1). A periapical radiograph was taken to assess the remaining root structure (Figure 2). Structurally, the tooth was deemed non-restorable, and treatment options were discussed with the patient, including replacement with an implant-supported crown.
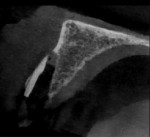
Three months prior to this emergency visit for the maxillary right lateral incisor, the patient had been treated in the practice with an implant in the posterior left maxilla and a CBCT scan was acquired. Examination of a cross section of this CBCT scan at the tooth No. 7 position revealed a thin facial plate of bone with dehiscence (Figure 3). As a result, traditional extraction of the lateral incisor and implant placement would require flap exposure of the facial aspect of the ridge and osseous grafting to ensure that the entire implant would be encased in bone following healing. This approach would also negate the possibility of immediately loading the implant and require the patient to wear a removable provisional to replace the missing tooth during healing.
An alternative approach would be to utilize partial extraction therapy (PET), in which the facial aspect of the root would be sectioned and left in the socket to act as a shield to prevent dehiscence once the implant was placed. If an acceptable insertion torque value was achieved using this approach, an immediate provisional restoration could be placed and worn during the implant's healing and osseointegration period. This procedure was discussed with the patient, and he accepted the treatment as recommended. To allow a surgical guide to be fabricated, the patient was scheduled for PET and implant placement the next day.
Virtual Treatment Planning
The patient's recently acquired CBCT scan was imported into the practice's dental treatment planning software (Blue Sky Plan® [v4.9.4], BlueSkyBio) and a virtual model of the maxillary arch was created. Because the crown that later fractured was present in the scan, modifications could be made to the coronal aspect to esthetically blend the new crown design with the adjacent teeth and better mirror the left lateral incisor. The virtual aspects of the old crown were then removed from the model, leaving the newly designed virtual crown. When the virtual model of the maxillary arch was articulated with a virtual model of the mandibular arch, the software indicated heavy occlusal contact on the distolingual aspect of the new crown. Therefore, the occlusion was adjusted on the virtual design so that the immediate provisional would have no occlusal contact when placed (Figure 4).
Utilizing the CBCT scan data, it was determined that an implant with a diameter of 3.3 mm would fit within the facial-lingual dimensions of the ridge and leave adequate space between the implant and adjacent teeth bilaterally. An implant length of 16 mm was selected to utilize all of the available bone height present, which would maximize the initial stability and permit immediate provisionalization. In the planning software, a virtual 3.3 mm × 16 mm implant was placed in the virtual model, positioning the long axis so that the screw access channel would be located on the lingual aspect of both the planned provisional restoration and the final restoration that would be created after the implant was completely osseointegrated (Figure 5).
Design and Fabrication of the Surgical Guide
The coronal aspect of the virtual tooth No. 7 crown was removed, and a socket was placed over the implant on the model. The surgical guide was then designed in the software to facilitate the creation of the osteotomy as well as the insertion of the implant (Figure 6). As part of the design, cutouts were placed over the occlusal and incisal portions of the remaining dentition, which would allow the practitioner to visually verify that the guide was fully seated on the remaining dentition prior to the initiation of guided implant surgery. The surgical guide was then printed on a dental 3D printer (Pro 55, SprintRay) using an appropriate biocompatible printing resin (Surgical Guide 3, SprintRay). Following printing, the supports were removed by hand, and the metal guide sleeve was luted into place using additional resin. This yielded a completed customized surgical guide that would enable precise preparation of the osteotomy and placement of the implant (Figure 7).
Design and Fabrication of the Provisional Restoration
One of the many benefits of virtually planned guided surgery is the ability to design and print the provisional restoration prior to the surgical appointment. For this case, a virtual titanium base was added over the planned implant on the virtual model, followed by the previously designed maxillary right lateral incisor crown. The virtual model and implant were then removed, which resulted in a design of the screw-retained provisional restoration on the titanium base. After the virtual titanium base was subtracted from the software, the resulting virtually designed screw-retained provisional crown was ready for printing (Figure 8). The provisional crown was 3D printed using a ceramic-filled hybrid resin material (SprintRay Crown [A1], SprintRay) (Figure 9). After the supports were removed, the crown was polished and then luted to the titanium base (CONELOG®, BioHorizons) with a dual-cure resin cement (Maxcem Elite™, Kerr Corporation). To complete the screw-retained provisional restoration, the margin between the titanium base and the resin crown was polished to remove any excess luting material (Figure 10).
PET and Implant Placement
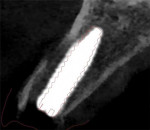
On the day of surgery, the patient presented, and the treatment plan was reviewed. The patient's questions were answered, and informed consent for PET and implant placement was acquired. Preoperatively, 2,000 mg of amoxicillin and 400 mg of ibuprofen were administered to the patient, and he was instructed to swish with chlorhexidine for 1 minute. After a topical anesthetic (20% benzocaine) was applied to the buccal vestibule at the right lateral incisor site with a cotton swab, local anesthesia was administered via infiltration using 1 cartridge of prilocaine (4% Citanest® Plain, Dentsply Sirona) and 2 cartridges of articaine HCL 4% and epinephrine 1:100,000 (Septocaine®, Septodont). Once profound anesthesia was achieved, a surgical carbide bur (P.E.T. Partial Extraction Therapy Bur Kit, Salvin Dental) was used in a highspeed handpiece to make a cut across the center of the maxillary right lateral incisor from the mesial aspect to the distal aspect, sectioning it into facial and lingual halves (Figure 11). Next, an elevator was utilized in the lingual periodontal ligament space to luxate the lingual portion of the root and remove it atraumatically. The facial portion of the root was then shaved from the prior cut at the center until only a 1-mm thick root segment remained that extended approximately 9 mm apically to the crestal bone (Figure 12). A periapical radiograph and a small field of view CBCT image were acquired to verify the integrity of the socket, its facial wall, and the remaining root segment (Figure 13 through Figure 15).
Once the integrity of the socket was verified, the previously fabricated 3D printed surgical guide was inserted, and complete seating was verified via the occlusal cutout on the first premolar and the incisal cutouts on the canine and central incisors (Figure 16). Osteotomy burs and guide sleeves (Guided Surgery Kit, BioHorizons) were then used to develop the site to accommodate a 3.3 mm × 16 mm implant (CONELOG®, BioHorizons) (Figure 17). Following completion of the osteotomy, the site was debrided with 5 mL of a 0.5 mg metronidazole solution. The implant was then placed through the surgical guide to ensure that the planned depth was achieved, which would ensure that the 3D printed immediate provisional restoration would be positioned where planned (Figure 18). After the implant was placed, its initial stability was evaluated using resonance frequency analysis (Osstell® ISQ, Osstell). It was found to have an implant stability quotient of 75; therefore, immediate provisionalization was indicated.
Grafting and Immediate Provisionalization
Because the virtual implant positioning was designed to allow for a thicker facial ridge following grafting and site healing, a gap was present between the facial aspect of the implant and the sectioned root attached to the facial aspect of the socket wall (Figure 19). A cover screw was placed to prevent any graft material from being caught in the implant-abutment connection, and then the facial gap was filled with a combination of mineralized cortical and cancellous chips (MinerOss® Blend, BioHorizons) that was hydrated with blood from the site (Figure 20). A postoperative CBCT scan was acquired to verify that the facial portion of the ridge over the implant did not have a dehiscence and that the plate was intact. Overlaying the planned virtual implant position over a cross section of the postoperative CBCT scan demonstrated that the guided position of the placed implant closely matched the virtually planned position, confirming the accuracy of guided implant placement protocols based on CBCT virtual planning (Figure 21).
Following radiographic evaluation of the implant position, the cover screw was removed, and the 3D printed screw-retained provisional restoration was inserted (Figure 22). The fixation screw was hand tightened so as not to turn the implant. To verify complete seating of the titanium base in the implant, a periapical radiograph was acquired (Figure 23). Sterilized PTFE tape was then placed into the access hole over the fixation screw, and the access was sealed with composite (Venus® Pearl, Kulzer) and light cured. Once the provisional restoration was placed, the occlusion was checked to confirm that there were no contacts in any position and adjusted as needed. The esthetics of the 3D printed provisional restoration allowed it to blend well with the adjacent dentition (Figure 24).
The patient was given postoperative instructions that included being told to avoid biting on the provisional crown because that could affect implant integration and lead to failure. Oral hygiene instructions were also given, and the patient was scheduled for a postoperative follow-up appointment 1 week later to check the progress of healing and verify the lack of occlusal contact on the provisional crown.
At the 1-week postsurgical follow-up, the patient reported that he had felt no discomfort following resolution of the local anesthesia, and he confirmed that he was following the postoperative instructions and avoiding chewing in the right anterior area of his mouth (Figure 25). The patient was then followed periodically for a planned 4-month osseointegration period before the final restoration was delivered.
Conclusion
Due to the patient's thin buccal plate, accurate implant placement was vital to the success of the treatment in this case. The use of CBCT for virtual planning and a 3D printed surgical guide for implant placement helped facilitate the required level of accuracy.3,4 Virtual planning permits an implant to be placed in the most ideal position based on the available anatomy. A surgical guide based on that virtual planning can then be 3D printed in the office, even on the day of surgery if necessary. In addition, the use of virtual planning allows for an immediate provisional restoration to be designed and 3D printed prior to the surgery so that chair time for the patient can be minimized and the efficiency of the treatment can be improved. 3D printing enables the fabrication of highly precise long-term provisional restorations from durable and esthetic materials.5
About the Authors
Rick Ferguson, DMD
Diplomate, American Board of Oral Implantology/ Implant Dentistry
Director, Implant Educators Academy
Private Practice
Davie, Florida
Gregori M. Kurtzman, DDS
Master, Academy of General Dentistry
Diplomate, International Congress of Oral Implantologists
Private Practice
Silver Spring, Maryland
References
1. Atieh MA, Alsabeeha NH, Payne AG, et al. Interventions for replacing missing teeth: alveolar ridge preservation techniques for dental implant site development. Cochrane Database Syst Rev. 2021;4(4):CD010176.
2. Bynum JH. Managing ridge resorption after tooth extraction using partial extraction therapy. Compend Contin Educ Dent. 2018;39(2):102-108.
3. Cho JY, Kim SB, Ryu J. The accuracy of a partially guided system using an in-office 3D-printed surgical guide for implant placement. Int J Comput Dent. 2021;24(1):19-27.
4. Bencharit S, Staffen A, Yeung M, et al. In vivo tooth-supported implant surgical guides fabricated with desktop stereolithographic printers: fully guided surgery is more accurate than partially guided surgery. J Oral Maxillofac Surg. 2018;76(7):1431-1439.
5. Xie C, Fang T, Wang Y, Yu H. A digital workflow for the fabrication of an immediate implant-supported interim restoration [published online ahead of print March 9, 2022]. J Prosthet Dent. 2022. doi: 10.1016/j.prosdent.2021.12.018.