A New Direction for Model-Based Guided Implant Placement—Part 2
This second of a two-part series describes the use of CBCT cross-sectional imaging to acquire buccolingual information needed for accurate implant placement.
In this second of a two-part discussion of the 3D Click Guide® (Idondivi, Inc., www.3dclickguide.com) for model-based guided implant placement, the author describes the use of cone beamcomputer tomography (CBCT) cross-sectional imaging as an alternative to bone sounding to acquire the buccolingual information needed for accurate implant placement.
Computed Tomography and Implants
In spiral.computed tomography (CT), an X-ray beam encircles the patient, who is slowly moved through it to capture a series of slices. With CBCT, a single cone that rotates around the patient is projected, and the data are captured on an opposing screen and.computed into a 3-dimensional (3-D) data set. Due to their differences, there are distinct positives and negatives to each of these technologies. Compared to spiral CT, CBCT needs less ionizing radiation, is less affected by metal artifacts, has a smaller footprint, and costs much less to purchase and operate; however, CBCT-generated images are less defined, are prone to beam hardening, cannot be used for Hounsfield density measurements, and are volumetrically not as precise as those from spiral CT.1-8 Yet the enthusiastic adoption of CBCT in the dental profession suggests that clinicians accept its negatives and embrace its positives. Very few dentists have had formal education in the application of this new technology, and consequently tend to rely heavily on manufacturer-supplied information. With that came an enthusiastic proclamation of necessity and words like “standard of care.” It took an article in the New York Times9 to remind the profession of the disadvantages as well as the advantages. Since then, it seems that there is a more balanced view. New technology needs time to prove that it indeed does improve the outcome of the delivered care enough to warrant the additional cost in money, time, and radiation.
Of course, developments in other fields might have an effect on the desirability of employing CBCT. For example, if there is 15 mm to the mandibular canal and the clinician wants to place a 13-mm implant, then it is highly likely that cross-sectional imaging does give the needed peace of mind. While in the past, 13 mm was the standard implant length, most implant.companies today report that a majority of the implants they sell now are 10 mm to 11.5 mm in length. An ever-increasing body of literature is making the point that even 8.5-mm implants work as well as the large ones.10-18 Some reports even describe implants as short as 4 mm functioning successfully.19 The reader can appreciate the clinician who, with that 15 mm to the mandibular canal, now wishes to place a short implant but may find that the safety margin toward the canal is so generous that cross-sectional imaging with CBCT does not add appreciable peace of mind as it did in the example of the 13-mm implant. Only the passage of time will show whether or not it improves the outcome. Clearly, technology will adapt to the needs of the profession, the profession will adapt to advances in technology, and third-party insurers will carefully consider whether such technology makes good use of their insurance dollars.
CBCT and Model-Based Guided Surgery
The purpose of this article is to describe the utilization of cross-sectional CBCT imaging specifically with the new 3D Click Guide, an economical, in-office, fully restrictive surgical guide. As was explained in Part 1 of this series, the 3D Click Guide is indicated for cases requiring one to two implants—ie, partially edentulous situations where the guide is supported by the remaining dentition; the clinical situation can be bounded by teeth or free ended.
When planning the placement of a dental implant, it is imperative to think about it as an object in space, as it requires consideration of the x, y, and z planes—the mesiodistal, buccolingual, and apico-coronal. The mesiodistal relationship of the coronal parts of the teeth is readily available from a dental cast. The mesiodistal information hidden from the eye can be derived from a conventional periapical radiograph. The apico-coronal information can also be derived from a periapical radiograph, but will need some help to be reliable enough to be used for measurements. The position of the top of the implant, the implant shoulder, is determined by the buccal margin of the gingiva. As current thinking put the shoulder 2 mm to 3 mm below this margin, no X-rays are needed here.
Determining the correct length of the implant depends on the philosophy of the treating dentist. Periapical images can easily be elongated or shortened. An instrument of known length, such as an indicator pin, can be placed in the intentionally short initial osteotomy when the radiograph is exposed (Figure 1). Because the deformation is uniform, a precise indication of length can be deduced. Again, if the plan is to use a short implant, less information is needed, and therefore there is less to image.
Next to discuss is the buccolingual plane. In part 1, bone sounding was explained as the technique of choice for 95% of the one- and two-implant cases treated by the author. The remaining 5% could not be treated based on bone sounding and periapical information alone, because there was not enough information to safely perform an osteotomy. In cases with advanced bone resorption, there is either not a sufficient amount of the bony crest available to impress—even with the previously described technique of overextended VPS impression, or the mandibular canal and the mental foramen are not visible on periapical X-rays even after taking a few from different angles. Taking a CBCT is the logical decision. The surgeon planning a simultaneous sinus lift who feels the need to acquire the information can take a CBCT. However, in consideration of the time, cost, and radiation involved, CBCT should be taken only when clearly necessary.20,21
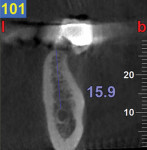
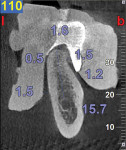
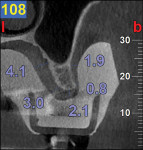
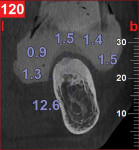
A CBCT study shows hard tissues and the shadow of soft tissues as long as they are surrounded by hard tissue. The pulpal tissue of the teeth is not visible, but the outline of the pulp chamber is visible. The mandibular nerve is not visible, but the cortical bone surrounding it does appear on the CBCT, making it possible to deduce where the mandibular nerve is expected to be. The proposed visualization technique allows very strong contrast to create a negative, much like the just-discussed image of the mandibular nerve. The concept is rather simple; VPS impression material can be radiopaque, but not all materials are radiopaque to the same extent, and some are not radiopaque at all (Figure 2). The patient wears a VPS impression during the CBCT exposure (Figure 3 and Figure 4). This can be the actual impression, or a dedicated impression made from a diagnostic cast (Figure 5). This simple technique shows a very distinct space, which is visible between the VPS material and the bone (Figure 6 and Figure 7). For the purpose of the 3D Click Guide fabrication, this space would otherwise be measured with the bone-sounding technique, as discussed in Part 1 of this series. Because the surface of the VPS impression visible in the CBCT image is exactly similar to the surface of the cast, the two can be exactly superimposed. Within the CBCT software, simple measurements can be made. Those measurements are made at the same locations as those used when bone sounding. Those measurements are then transferred to the cast. Additional information—eg, location of the mandibular canal—can be extrapolated and drawn as needed (Figure 8 and Figure 9).
Clinical Case
An 80-year-old woman, who presented with a missing lower molar, requested an implant-supported replacement. Advanced periodontal bone loss at site No. 19 resulted in considerable resorption of the alveolar ridge after healing. Although simple bone sounding is the preferred data-gathering technique for the author, in this case, there was insufficient information available to safely perform an osteotomy. The decision was made to gather additional information with a CBCT study.
An intentionally overextended VPS impression was made by placing a stiff VPS putty material (ExaMix™, GC America, www.gcamerica.com) in a stock impression tray. The soft putty was covered with a plastic wrap (Saran Wrap, SC Johnson, www.saranbrands.com), and the impression was seated. Finger pressure was used to push the stiff putty against the soft tissue, thus.compressing the soft tissue tightly against the bone. Upon setting, the impression was removed, and a small volume of freshly mixed putty was added to the area surrounding the edentulous site; it was covered with the plastic wrap, and the impression was reseated. Again, finger pressure was used to now overextend the impression even more. Once set, the impression was removed, the plastic wrap discarded, and the putty impression was loaded with injection-type VPS impression material (ExaMix). The tray was then reseated. A CBCT volume was taken while the injection VPS impression material was setting (Figure 10) to ensure that the impression was perfectly seated while also saving time. The impression was cast in a dedicated VPS casting material (Blu-Mousse®/Mach-2®/Mach-SLO™, Parkell, Inc., www.parkell.com). Since the casting material is similar to the impression material, a separating medium was first applied (Release Anti-Adhesive and Dry Lubricant, Cetylite Industries, www.cetylite.com). Alternatively, one could cast the impression with dental stone. A base former with a built-in indexing system was used (Accu-trac® tray-system, Coltène, Inc., www.coltene.com) to allow reassembly of the cut cast. A dual-layer vacuformed carrier was created by simultaneously heating and forming a 1-mm soft-guard material and 0.75-mm bondable material together (Essix® A+ and model duplication material, DENTSPLY Raintree Essix, www.essix.com). Alternative carriers can be thermoplastics (Tak Hydroplastic, www.taksystems.com) or even a stiff VPS bite-registration material.
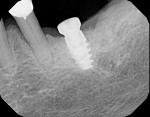
The cast was sectioned 4 mm distal of tooth No. 20. The data from the corresponding cross-sectional cut were transferred to the cast. The ideal buccolingual axis was drawn onto the cast, based on a screw access hole in the central fossa of the future crown. A small hole was drilled at the desired location of the shoulder of the implant. The pin of the Bucco Lingual Positioner (BLP) was placed in the hole, and the central groove of the BLP was lined up with the drawn implant axis. A drop of fast-setting cyano-acrylate glue was applied to lock the BLP in place (Figure 11). The opposing part of the cast was adjusted and the cast was reassembled into the Accu-trac tray. At this point, the buccolingual axis and the top of the implant were irreversibly set, and the mesiodistal could be determined without the risk of making inadvertent changes in the buccolingual plane. The correction slot in the crossbar of the wing assembly fits snugly over the top of the BLP, allowing mesiodistal rotation and mesiodistal translation (Figure 12). Once the correct mesiodistal position was selected, the wings were irreversibly connected to the vacuformed carrier by means of ortho-acrylic (Orthoresin, DENTSPLY International, www.dentsply.com); then the cross-sectional bar was removed, allowing placement of a rotation block. The surgical guide was placed in the mouth and a periapical radiograph was exposed (Figure 13). Note that if the buccal and lingual wings overlap and appear to be one, the radiograph has been taken exactly perpendicular to the ridge, allowing a decision to be made because the image is of acceptable diagnostic quality. In this case, the trajectory was as desired, and the 0º rotation block was selected, as there was no need for rotation adjustments by means of the 3º or 7º rotation blocks (Figure 14). The surgical guide was sterilized in a cold sterilizing solution and the surgery was performed per the manufacturer’s drilling protocol. A 8.5-mm x 4.3-mm implant (NobelActive™ 4.3 x 10 mm, Nobel Biocare, www.nobelbiocare.com) was placed as planned (Figure 15).
Conclusion
Three-dimensional implant placement is driven by an international peer-established knowledge base of criteria. The clinical execution in a freehand or limited guided manner is still highly dependent on individual operator skill. Fully restrictive surgical guides allow operators with less experience to place implants expertly, and they enable experienced clinicians to do so more expediently. Computer-generated surgical guides are less economical for smaller cases; hence the development of an economical dedicated analog surgical guide for one- and two-implant cases. 3D Click Guide is an in-office, model-based surgical concept using data from bone sounding measurements or, if desired, CBCT.
Disclosure
Dr. Stumpel is the owner of Idondivi, Inc.
References
1. Koong B. Cone beam imaging: is this the ultimate imaging modality? Clin Oral Implants Res. 2010;21(11):1201-1208.
2. Draenert FG, Coppenrath E, Herzog P, et al. Beam hardening artifacts occur in dental implant scans with the NewTom cone beam CT but not with the dental 4-row multidetector CT. Dentomaxillofac Radiol. 2007;36(4):198-203.
3. Sanders MA, Hoyjberg C, Chu CB, et al. Common orthodontic appliances cause artifacts that degrade the diagnostic quality of CBCT images. J Calif Dent Assoc. 2007;35(12):850-857.
4. Liang X, Lambrichts I, Sun Y, et al. A.comparative evaluation of cone beam.computed tomography (CBCT) and multi-slice CT (MSCT). Part II: On 3D model accuracy. Eur J Radiol. 2010;75(2):270-274.
5. Yu L, Vrieze TJ, Bruesewitz MR, et al. Dose and image quality evaluation of a dedicated cone-beam CT system for high-contrast neurologic applications. AJR Am J Roentgenol. 2010;194(2):W193-201.
6. Watanabe H, Honda E, Tetsumura A, Kurabayashi T. A.comparative study for spatial resolution and subjective image characteristics of a multi-slice CT and a cone-beam CT for dental use. Eur J Radiol. 2011;77(3):397-402.
7. Nackaerts O, Maes F, Yan H, et al. Analysis of intensity variability in multislice and cone beam.computed tomography. Clin Oral Implants Res. 2011;22(8):873-879.
8. Hua Y, Nackaerts O, Duyck J, et al. Bone quality assessment based on cone beam.computed tomography imaging. Clin Oral Implants Res. 2009;20(8):767-771.
9. Bogdanich W, Craven McGinty J. Radiation worries for children in dentists’ chairs. New York Times. November 22, 2010.
10. Renouard F, Nisand D. Short implants in the severely resorbed maxilla: a 2-year retrospective clinical study. Clin Implant Dent Relat Res. 2005;7(Suppl 1):S104-S110.
11. Kotsovilis S, Fourmousis I, Karoussis IK, Bamia C. A systematic review and meta-analysis on the effect of implant length on the survival of rough-surface dental implants. J Periodontol. 2009;80(11):1700-1718.
12. Anitua E, Orive G. Short implants in maxillae and mandibles: a retrospective study with 1 to 8 years of follow-up. J Periodontol. 2010;81(6):819-826.
13. Grant BT, Pancko FX, Kraut RA. Ou.comes of placing short dental implants in the posterior mandible: a retrospective study of 124 cases. J Oral Maxillofac Surg. 2009;67(4):713-717.
14. Griffin TJ, Cheung WS. The use of short, wide implants in posterior areas with reduced bone height: a retrospective investigation. J Prosthet Dent. 2004;92(2):139-144.
15. Maló P, de Araújo Nobre M, Rangert B. Short implants placed one-stage in maxillae and mandibles: a retrospective clinical study with 1 to 9 years of follow-up. Clin Implant Dent Relat Res. 2007;9(1):15-21.
16. Misch CE, Steignga J, Barboza E, et al. Short dental implants in posterior partial edentulism: a multicenter retrospective 6-year case series study. J Periodontol. 2006;77(8):1340-1347.
17. Arlin ML. Short dental implants as a treatment option: results from an observational study in a single private practice. Int J Oral Maxillofac Implants. 2006;21(5):769-776.
18. Nedir R, Bischof M, Briaux JM, et al. A 7-year life table analysis from a prospective study on ITI implants with special emphasis on the use of short implants. Results from a private practice. Clin Oral Implants Res. 2004;15(2):150-157.
19. Slotte C, Grønningsaeter A, Halmøy AM, et al. Four-millimeter implants supporting fixed partial dental prostheses in the severely resorbed posterior mandible: two-year results. Clin Implant Dent Relat Res. 2011 May 20. doi: 10.1111/j.1708-8208.2011.00346.x. [Epub ahead of print]
20. Walter C, Weiger R, Dietrich T, et al. Does three-dimensional imaging offer a financial benefit for treating maxillary molars with furcation involvement? A pilot clinical case series. Clin Oral Implants Res. 2012;23(3):351-358.
21. Roberts JA, Drage NA, Davies J, Thomas DW. Effective dose from cone beam CT examinations in dentistry. Br J Radiol. 2009;82(973):35-40.
About the Authors
Lambert J. Stumpel, III, DDS
Private Practice
San Francisco, California