Managing Dentin Hypersensitivity
Howard E. Strassler, DMD; and Francis Serio, DMD, MS,MBA
Dentin hypersensitivity, also known as tooth sensitivity, root sensitivity, or just sensitivity, is a common patient complaint. Patients describe this phenomena as sharp, short-lasting tooth pain irrespective of the stimulus.1 Holland et al described dentin hypersensitivity as “characterized by short, sharp pain arising from exposed dentin in response to stimuli typically thermal, evaporative, tactile, osmotic, or chemical and that cannot be ascribed to any other form of dental defect of pathology.”2 Clinicians see dentin hypersensitivity as an exaggerated response to routine stimuli to the teeth. Patients respond to dentin hypersensitivity when drying a tooth with an air spray or scratching a tooth with the tip of an explorer. Some patients complain of pain when brushing their teeth or flossing. Although it causes no direct harm to the tooth, dentin, or pulp, it has all the criteria to be considered a true pain syndrome.3
It is important to distinguish sensitivity pain—which is of short duration—from pain of longer duration, not treatable with desensitizing agents, which may be the result of pulpal inflammation.4 Frequently, dentin hypersensitivity is triggered by tooth exposure to cold foods, sweets, beverages, or plaque accumulation on exposed root surfaces. Dentin hypersensitivity has been referred to as one of the most painful and least successfully treated chronic dental conditions of the teeth.5
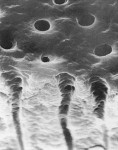
Once a diagnosis has been made and depending on the etiology of the condition (Figure 1; Figure 2A and Figure 2B; Figure 3; Figure 4; Figure 5; Figure 6), treatment recommendations can be made that could include in-office professionally applied treatments, at-home professionally dispensed treatments, or recommendations for over-the-counter (OTC) treatments.6 No matter what treatment recommendations are made and provided, it is important for the clinician to follow up with the patient to evaluate the therapeutic results of treatment recommendations.
Treatment of Dentin Hypersensitivity
With the correct diagnosis, a treatment plan can be developed and implemented7 (Table 1). Drisko summarized preventive recommendations for dentin hypersensitivity.8 Suggestions for patients include avoiding the following:
- gingival recession resulting from poor plaque removal;
- using large amounts of dentifrice or reapplying it during brushing;
- using medium- or hard-bristle toothbrushes;
- brushing teeth immediately after eating acidic foods;
- overbrushing with excessive pressure or for an extended period of time;
- excessive flossing or improper use of other interproximal cleaning devices; and
- “picking” or scratching at the gumline or using toothpicks inappropriately.
Suggestions for professionals include avoiding the following:
- over-instrumenting the root surfaces during scaling and root planing, particularly in the cervical area of the tooth;
- over-polishing exposed dentin during stain removal;
- violating the biologic width during restoration placement, as this may cause recession; and
- burning the gingival tissues during in-office bleaching and advising patients to be careful when using home-bleaching products.
Improper toothbrushing also has been associated with dentin hypersensitivity.1 The patient should be shown correct brushing techniques to prevent further loss of dentin that would contribute to dentin hypersensitivity. While it has been suggested that the use of a power toothbrush would be less damaging than a manual brush, it has been shown that both a manual and a power toothbrush used with a desensitizing toothpaste were almost equivalent in effectiveness.9 A new powered toothbrush, the Oral B Triumph™ with SmartGuide™ (Oral B, Mason, OH) has a pressure monitor that activates a red warning light when too much pressure is applied to the tooth.
Self-applied Products
OTC treatments for sensitive teeth, usually in the form of toothpastes, are a major category of dentifrice. Because the use of an OTC product can be the most cost-effective means for a patient to receive care, many people make the decision to self-medicate with desensitizing toothpastes.
Dentifrices claiming a desensitization effect come under scrutiny from the Federal Drug Administration (FDA) because the claim of desensitizing teeth is a therapeutic claim that must be substantiated by either clinical trials or the addition of an ingredient to the toothpaste that is recognized as being an effective, active agent for the treatment of the condition listed. Two potassium compounds have been added to toothpastes to reduce dentin hypersensitivity. The most popular ingredient for desensitizing in toothpastes is potassium nitrate. According to the FDA monograph, for a toothpaste to claim to be desensitizing, it needs to contain 5% potassium nitrate as an active ingredient.10 The mode of action of 5% potassium nitrate has been described as a penetration of the potassium ions through the tubules to the A-fibers of the nerves, decreasing the excitability of these nerves.11-13
Many desensitizing toothpastes that use 5% potassium nitrate will contain fluoride for an anti-caries effect and may contain anti-tartar, antigingivitis, and/or whitening ingredients (eg, the Sensodyne® [GlaxoSmithKline, Parsippany, NJ] brand line) so that multiple claims for treatment can be made by the manufacturer for a given toothpaste. Studies have evaluated the effectiveness of toothpastes containing 5% potassium nitrate and other additives.14-17 There is no doubt that toothpastes containing 5% potassium nitrate with other additives are effective in reducing dentin hypersensitivity and root sensitivity. Many clinical trials have provided evidence of a reduction in tooth sensitivity with dentifrices containing potassium nitrate.14,15,18-21 For best results, patients should use a desensitizing toothpaste twice a day as part of their oral care regimen. It may take 7 to 14 days for the patient to notice an appreciable decrease in sensitivity.
Another at-home but professionally prescribed treatment for dentin hypersensitivity that provides for both rapid and continued relief using a bioactive glass technology was introduced. SootheRx™ (3M ESPE, St. Paul, MN) contains a calcium sodium phosphosilicate bioactive glass (NovaMin®, NovaMin Technology, Inc, Alachua, FL) that induces the formation of hydroxyapatite to seal and clog open dentinal tubules. The basis for this use comes from a clinical trial using the same active ingredient for the treatment of dentinal hypersensitivity in toothpaste.22,23 In a prophylactic paste (NuCare™, Sunstar Butler, Chicago, IL), bioactive glasses have been added for their low abrasion and dentinal tubule surface sealing capacity for the treatment of dentinal hypersensitivity.
In recent years, vital bleaching to change the esthetic appearance of teeth has become very popular. Tooth sensitivity has been a primary adverse effect reported with at-home tooth whitening.24 The incidence of tooth sensitivity has been reported to range from 7% to 75%.25-28 While sensitivity when whitening has been reported to be transient, for many patients it is a barrier to continuing treatment. The recommendation for the use of desensitizing toothpastes containing 5% potassium nitrate have been made for patients with a chief complaint of sensitivity while using at-home bleaching agents.24,29-31 Two effective strategies using a 5% potassium-nitrate desensitizing toothpaste that have been clinically evaluated are brushing with the desensitizing toothpaste for 2 weeks before initiating bleaching24,30 and having the patient place a sensitivity toothpaste containing a 5% potassium nitrate into their bleaching tray and wearing the tray for 30 minutes a day 1 week before the initiation of bleaching.32 Both of these strategies take into account the mechanism for desensitizing that potassium nitrate provides. In the reported studies, these recommendations have been successful in controlling bleaching sensitivity. These recommendations should be made for patients to use desensitizing dentifrices with other ingredients based on a patient’s therapeutic needs for anti-caries, antigingivitis, whitening, and anti-tartar.
Amorphous calcium phosphate (ACP) compounds and additives to vital bleaching gels also have been demonstrated to control bleaching sensitivity.32-34 Two mouthguard bleaching gels (Night White® ACP and Day White® ACP, Discus Dental, Culver City, CA) have added ACP to their formulation. In a recent study comparing a 15% carbamide peroxide bleaching gel with potassium nitrate and fluoride to a 16% carbamide peroxide bleaching gel with ACP, the bleaching effect was not affected by the desensitizing additives and there was no difference in the desensitizing effect of the added desensitizing agents.35 Other ACP-containing products (MI Paste, GC America, Alsip, IL and Relief® ACP, Discus Dental) are recommended to be brushed on teeth before and after mouthguard or in-office bleaching.
In-office Treatment
Because recession is a major predisposing factor to exposed root surfaces and dentin hypersensitivity, gingival grafts should be considered as part of a treatment plan, particularly when the recession is progressive, there are esthetic concerns, or the sensitivity is unresponsive to more conserva-tive treatment.36,37 When the exposed sensitive root has surface loss because of abrasion, erosion, and/or abfraction leaving a notching of the root, consideration should be given to placing either an adhesive composite resin or glass ionomer restoration.38 These restorations will both restore the tooth to full contour and seal the exposed and open dentinal tubules.
Lasers have been used successfully to seal open dentinal tubules either by themselves or with surface treatments with other materials.39-41 The use of a Er: YAG laser has been shown to be effective for desensitizing hypersensitive dentin for up to 6 months.39 The desensitizing effect was attributed to the deposition of insoluble salts into the exposed dentinal tubules. Another study investigated the use of He:Ne laser and a combined He:Ne Nd:YAG laser for the treatment of dentin hypersensitivity.40 Their findings indicated that both treatments reduced dentin hypersensitivity by more than 60% for up to 3 months. Surface sealing of patent dentinal tubules using a combined bioglass paste with a Nd:YAP laser has also been demonstrated.41
Another treatment for dentin hypersensitivity that has been described is iontophoresis. This technique uses a low galvanic current to accelerate ionic exchanges and precipitation of insoluble calcium with fluoride gels to occlude open tubules.37
In-office, paint-on surface treatments are a more popular approach to treating root hypersensitivity. These are especially effective when localized conditions (single teeth) demonstrate dentin hypersensitivity. A variety of products have been re-ported to successfully reduce dentinal hyper-sensitivity. These products generally occlude and seal the dentin tubules. Resin-based materials have been reported to successfully reduce dentin hypersensitivity.42-46 Use of a 5% sodium fluoride varnish (Duraphat®, Colgate-Palmolive, New York, NY) painted over exposed root surfaces has been shown to be an effective treatment of dentin hypersensitivity.47 An aqueous solution of 5% glutaraldehyde and 35% hydroxyethylmethacrylate (HEMA), Gluma Desensitizer® (Heraeus Kulzer, Armonk, NY) has been reported to be an effective desensitizing agent for up to 9 months.44,48 The mechanism for tubule occlusion by Gluma Desensitizer appears to be a result of the glutaraldehyde’s effects.49 The use of oxalates for the treatment of dentin hypersensitivity has been shown to be effective.4,50 The oxalate precipitates on the open dentinal tubules, occluding them. This action reduces patient perception of pain to external stimuli. A dual-action oxalate desensitizer with potassium nitrate (D/Sense 2®, Centrix, Shelton, CT) has been shown to be an effective desensitizer.50 This product occludes open dentinal tubules and provides the desensitizing effect of potassium nitrate.
Recommendations and techniques for the use of in-office, paint-on desensitizing agents are product-specific. Clinicians need to understand the in-office, paint-on desensitizing agents to be able to select which one is appropriate. As previously noted, when the root surface is exposed with the presence of notching, the depth and size of the notching will in some cases require the placement of a restoration.38
An often overlooked remedy for the reduction of dentin hypersensitivity is the application of a steroid suspension to the root surface. In one of the authors’ (Dr. Serio’s) experience, the application of a 0.5% or 1% prednisolone suspension using a cotton pellet to burnish the suspension into a dry root surface for 2 minutes, repeated once if necessary, often brings relief when other topical approaches have not been successful. When this procedure works, the patient notices significant if not complete cessation of the sensitivity immediately after the application of the steroids. There is scant research in this area, but the approach may be a valid one.
Conclusion
Dental professionals need to understand the causes of dentin hypersensitivity. Questions about dentin hypersensitivity should be asked at all appointments. A patient should be evaluated based on risk factors that may be present. Once a diagnosis has been made and the factors have been identified, a treatment plan can be outlined to the patient for the treatment of dentin hypersensitivity. Depending on the severity of the condition, clinical management of dentin hypersensitivity may include both in-office and self-applied, at-home therapies. In most circumstances, the least-invasive, most cost-effective treatment is the recommendation to use an effective toothpaste that provides desensitizing effects. For individual teeth that are hypersensitive, an in-office treatment can provide the patient with pain relief. Once a tooth is predisposed to dentin hypersensitivity, it will need to be reevaluated for continued at-home treatment.
Disclosure
Dr. Strassler has received grant/research support from G.C. America and is a current consultant for Oral B, G.C. America, and Centrix. Dr. Serio is a current consultant for Oral B.
References
1. Dababneh RH, Khouri AT, Addy M. Dentine hypersensitivity—an enigma? A review of terminology, mechanisms, aetiology and management. Brit Dent J. 1999;18(11): 606-611.
2. Holland GR, Narhi MN, Addy M, et al. Guidelines for the design and conduct of clinical trials on dentine hypersensitivity. J Clin Periodontol. 1997;24(11):808-813.
3. Curro FA. Tooth hypersensitivity in spectrum of pain. Dent Clin North Am. 1990;34(3):429-437.
4. Camps J, Pashley D. In vivo sensitivity of human root dentin to air blast and scratching. J Periodontol. 2003;74(11):1589-1594.
5. Silverman G, Berman E, Hanna CB, et al. Assessing the efficacy of three dentifrices in the treatment of dentinal hypersensitivity. J Am Dent Assoc. 1996;127(2):191-201.
6. Orchardson R, Gillam GC. Managing dentin hypersensitivity. J Am Dent Assoc. 2006; 137(7):990-998.
7. Canadian Advisory Board on Dentin Hypersensitivity. Consensus-based recommendations for the diagnosis and management of dentin hypersensitivity. J Can Dent Assoc. 2003;69(4): 221-226.
8. Drisko CH. Dentine hypersensitivity—dental hygiene and periodontal considerations. Int Dent J. 2002;52(4): 385-393.
9. Sengupta K, Lawrence HP, Limeback H, Matear D. Comparison of power and manual toothbrushes in dentine sensitivity. J Dent Res (Special Issue A). 2005;84: Abstract no. 942.
10. Federal Register. 1992;57(91):20114-20115.
11. Markowitz K, Bilotto G, Kim S. Decreasing intradental nerve activity in the cat with potassium and divalent cations. Arch Oral Biol. 1991;36(1):1-7.
12. Peacock JM, Orchardson R. Effects of potassium ions on action potential conduction in A- and C- fibers of rat spinal nerves. J Dent Res. 1995;74(2):634-641.
13. Markowitz K, Kim S. The role of selected cations in the desensitization of intradental nerves. Proc Finn Dent Soc. 1992;88(Suppl 1):39-54.
14. Schiff T, Zhang YP, DeVizio W, et al. A randomized clinical trial of the desensitizing efficacy of three dentifrices. Compend Contin Educ Dent Suppl. 2000;21(Supple 27):4-10.
15. Sowinski JA, Battista GW, Petrone ME, et al. A new desensitizing dentifrice A: an 8-week clinical investigation. Compend Contin Educ Dent. 2000;21(Supple 27):11-16.
16. Wara-aswapati N, Krongnawakul D, Jiraviboon D, et al. The effect of a new toothpaste containing potassium nitrate and triclosan on gingival health, plaque formation and dentine sensitivity. J Clin Periodontol. 2005;32(1):53-58.
17. Schiff T, Bonta Y, Proskin HM, et al. Desensitizing efficacy of a new dentifrice containing 5.0% potassium nitrate and 0.454% stannous fluoride. Am J Dent. 2000;13(3):111-115.
18. Sowinski J, Ayad F, Petrone M, et al. Comparative investigations of the desensitizing efficacy of a new dentifrice. J Clin Periodontol. 2001;28(11):1032-1036.
19. Sowinski JA, Bonta Y, Battista GW, et al. Desensitizing efficacy of Colgate Sensitive Maxium Strength and Fresh Mint Sensodyne dentifrices. Am J Dent. 2000; 13(3):116-120.
20. Ayad F, Berta R, DeVizio W, et al. Comparative efficacy of two dentifrices containing 5% potassium nitrate on dentinal sensitivity: a twelve-week clinical study. J Clin Dent.1994;5 (Spec No):97-101.
21. Conforti N, Battista GW, Petrone DM, et al. Comparative investigation of the desensitizing efficacy of a new dentifrice: a 14-day clinical study. Compend Contin Educ Dent Suppl. 2000;21(Suppl 27): 17-22.
22. Gillam DG, Tang JY, Mordan NJ, Newman HN. The effects of a novel Bioglass dentifrice on dentine sensitivity: a scanning electron microscopy investigation. J Oral Rehabil. 2002;29(4):305-313.
23. Du MQ, Tai BJ, Jiang H, et al. Efficacy of dentifrice containing bioactive glass (NovaMin®) on dentine hypersensitivity. J Dent Res. 2003;83(Special Issue A): Abstract no. 1546.
24. Haywood VB. Treating sensitivity during tooth whitening. Compend Contin Educ Dent. 2005;26(9 Suppl 3):11-20.
25. Haywood VB, Leonard RH, Nelson CF, Brunson WD. Effectiveness, side effects and long-term status of nightguard vital bleaching. J Am Dent Assoc. 1994;125(9):1219-1226.
26. Swift EJ Jr, May KN Jr, Wilder AD Jr, et al. Six-month clinical evaluation of a tooth whitening systems using an innovative experimental design. J Esthet Dent. 1997;9(5): 265-274.
27. Matis BA, Cochran MA, Eckert G, et al. The efficacy and safety of a 10% carbamide peroxide bleaching gel. Quintessence Int. 1994;29(9):555-563.
28. Leonard RH, Bentley C, Eagle JC, et al. Nightguard vital bleaching: a long-term study on efficacy, shade retention, side effects, and patient’s perceptions. J Esthet Restor Dent. 2001;13(6):357-369.
29. Geiger S, Matalon S, Blashalg J, et al. The clinical effect of amorphous calcium phosphate (ACP) on root surface sensitivity. Oper Dent. 2003;28(5):496-500.
30. Haywood VB, Cordero R, Wright K, et al. Brushing with a potassium nitrate dentifrice to reduce bleaching sensitivity. J Clin Dent. 2005;16(1): 17-22.
31. Leonard RH Jr, Smith LR, Garland GE, Caplan DJ. Desensitizing agent efficacy during whitening in an at-risk population. J Esthet Restor Dent. 2004;16:49-55.
32. Strassler HE. Tooth whitening—now and in the future: Part 2. Contemporary Esthetics and Restorative Practice. 2004;8(9):50-55.
33. Dunn J, Wilson AC, Arambula M, Kim JS. Effects of TiON gel applications on in-office tooth whitening. J Dent Res. 2006;85 (Special Issue A): Abstract no. 1369.
34. Giniger M, Macdonald J, Ziemba S, Felix H. The clinical performance of professionally dispensed bleaching gel with added amorphous calcium phosphate. J Am Dent Assoc. 2005;136(3):383-392.
35. Matis B, Cochran MA, Ekert GJ, Matis JL. In vivo study of two carbamide peroxide gels with different desensitizing agents. Oper Dent. 2007;32(6):549-555.
36. Fombellida Cortazar F, Sanz Dominguez JR, Keogh TP, et al. A novel surgical approach to marginal soft tissue recessions: two-year results of 11 case studies. Pract Proced Aesthet Dent. 2002;14(9):749-754.
37. Gangarosa LP Sr. Iontophoretic application of fluoride in tray techniques for desensitizing multiple teeth. J Am Dent Assoc. 1981;102(1): 50-52.
38. Starr GB. Class 5 restorations. In: Summitt JB, Robbins JW, Schwartz RS, eds. Fundamentals of Operative Dentistry a Contemporary Approach. 2nd ed. Quintessence Books; Chicago: 386-400.
39. Schwarz F, Arweller N, Georg T, Reich E. Desensitizing effects of an Er:YAG laser on hypersensitive dentine: A controlled, prospective clinical study. J Clin Periodontol. 2002;29(3):211-215.
40. Gelskey SC, White JM, Pruthi VK. The effectiveness of the Nd:YAG laser in the treatment of dentin hypersensitivity. J Can Dent Assoc. 1993;59(4):377-386.
41. Lee B, Chang C, Chen W, et al. In vitro study of dentin hypersensitivity treated by Nd:YAP laser and bioglass. Dent Mater. 2005;21(6): 511-519.
42. Duran I, Sengun A. The long-term effectiveness of five current desensitizing products on cervical dentine sensitivity. J Oral Rehabil. 2004;31(4): 351-356.
43. Dondi dall’Orologio G, Lorenzi R, Anselmi M, Opisso V. Dentin desensitizing effects of Gluma Alternative, Health-Dent Desenstizer, and Scotchbond Multi-Purpose. Am J Dent. 1999;12(3):103-106.
44. Kakaboura A, Rahiotis C, Thomaidis S, Doukoudakis S. Clinical effectiveness of two agents on the treatment of tooth cervical hypersensitivity. Am J Dent. 2005;18(4):291-295.
45. Pamir T, Dalgar H, Onal B. Clinical evaluation of three desensitizing agents in relieving dentin sensitivity. Oper Dent. 2007;32(6):544-548.
46. Kakaboura A, Rahiotis C, Thomaidis S, Doukoudakis S. Clinical effectiveness of two agents on the treatment of tooth cervical hypersensitivity. Am J Dent. 2005;18(4):291-295.
47. Gaffar A. Treating hypersensitivity with fluoride varnishes. Compend Contin Educ Dent. 1999;20(1 Suppl):27-33.
48. Schüpback P, Lutz F, Finger WJ. Closing of dentinal tubules by Gluma desensitizer. Eur J Oral Sci. 1997;105(5 Pt 1):414-421.
49. Yiu CK, Hiraishi N, Chersoni S, Breschi L, et al. Single bottle adhesives behave as permeable membranes after polymerisation. II. Differential permeability reduction with an oxalate desensitiser. J Dent. 2006;34(2):106-116.
50. Crispin BJ. Dentin sensitivity and the clinical evaluation of a unique dual-action dentin desensitizer. Contemporary Esthetics and Restorative Practice. 2001;8(3 Suppl):3-7.
About the Authors
Howard E. Strassler, DMD
Professor and Director of Operative Dentistry
Department of Endodontics, Prosthodontics, and Operative Dentistry
University of Maryland School of Dentistry
Baltimore, Maryland
Francis Serio, DMD, MS, MBA
Professor and Chair
Department of Periodontics and Preventive Sciences
University of Mississippi School of Dentistry
Jackson, Mississippi