A Digital Workflow for Single Unit Implant Restorations
Digital design and surgical guides make implant placement easy and predictable
Michael J. Boudreaux, DDS
Digital technology has the potential to take what once would have been a challenging case and make it relatively easy and predictable. Today, this is especially true for implants because the utilization of intraoral scan and cone-beam computed tomography (CBCT) data along with implant planning software and 3D printed surgical guides makes implant placement and delivery of the final restoration stress-free. The procedure can be reverse engineered with the final prosthesis in mind, which makes the process predictable from start to finish.
Case Report
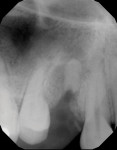
A young female patient presented to the practice with a decayed single premolar (tooth No. 5) that required extraction (Figure 1). The patient had healthy dentition adjacent to the extraction site, so a fixed bridge was an option, but due to her age and the strong esthetics of the adjacent teeth, an implant-supported restoration was preferable.
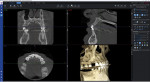
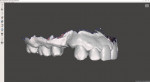
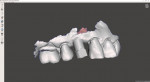
Four months after extraction, a CBCT scan and intraoral scan were acquired (Figure 2 and Figure 3), and the data was then used to place the virtual tooth and visualize the final restoration (Figure 4 through Figure 6). At this stage, when the quantity and quality of the bone is sufficient, the clinician can plan the implant placement. Bone grafting may be necessary in some cases, but for this patient, the bone allowed for ideal placement. After an implant was selected from the library, it was placed in the virtual planning software, and a surgical guide was created to facilitate its ideal trajectory (Figure 7 through Figure 9). The surgical guide was then fabricated on a 3D printer, which provided the necessary level of precision for it.
When the patient arrived on the day of surgery, the surgical guide fit perfectly (Figure 10). The implant was placed (Figure 11), followed by a healing abutment, and the patient entered a healing phase prior to receiving the final restoration. Over the course of approximately 3 weeks, the patient developed a good emergence profile. When she returned to the office for restoration, a scan body was placed, the site was scanned (Figure 12), and the scan data was imported into the CAD software (Figure 13). The final restoration was then designed on an abutment (Figure 14 and Figure 15) and milled from zirconia (Figure 16 and Figure 17). It was delivered and fit perfectly.
This author has found 3D printed surgical guides to be almost 100% effective. Other than in rare cases, such as when the bone is softer than anticipated, surgical guides help clinicians accomplish the desired outcome every time. 3D printing technology has evolved in recent years, but perhaps just as critically, a seemingly endless amount of resources are now available to help any practice implement the technology. As a result, the process is not nearly as daunting as it was even just 4 years ago.
So many errors can occur with analog processes for single implants. Even when precision is not an issue, the arbitrary placement of an implant without consideration of the final restoration can lead to an angulation that makes restoring it a huge challenge. Fully guided surgery may not be considered the standard of care yet, but in this author's practice, it is the bare minimum. Implant placement is made easy and completely predictable with this workflow because everything lies in the planning and fabrication of the guides.
About the Author
Michael J. Boudreaux, DDS
Private Practice
Houma, Louisiana