The Maxillary Central Incisor Implant: A Guide for Ideal Esthetic Implant Placement
Michael K. Sonick, DMD
The surgical success of dental implants has become quite predictable.1 It is no longer enough to merely achieve osseointegration in dental implant therapy. Patients require implants that are esthetic as well as functional. The responsibility to deliver an ideal esthetic implant restoration begins with the surgeon.
Replacing a hopeless tooth presents a number of options for the clinician. Treatment options include a fixed, bonded pbodyial denture; a fixed, tooth-supported bridge; a removable pbodyial denture; and a dental implant. Fixed and removable pbodyial dentures are wrought with problems. Implant restorations are often chosen for the following reasons:
- They are non-removable and permanent.
- Adjacent teeth are preserved.
- The success rate is significantly higher than for a fixed bridge.
- The strength of the restoration is increased.
- The case is segmented.
- Extraction site bone is preserved and stabilized.
- The patient is able to floss.
- Cosmetics are enhanced.
- Future dental costs are decreased.2
Once a treatment plan is selected, the sequence of treatment must be determined. Many options exist, and there is no 1 correct sequence in implant treatment planning. Questions must be answered prior to performing any implant treatment, and they include, but are not limited to, the following:3
- When do you place the implant: immediately, 2-months post-extraction, or 6-months post-extraction?
- Is bone grafting needed?
- What do you graft with: autograft, allograft, synthograft, or xenograft?
- When do you graft: at extraction, 2-months post-extraction, or at the time of implant placement?
- Is it done as a single stage or 2-stage procedure?
- How many months do you wait for osseointegration?
- When do you perform second-stage surgery?
- How long thereafter do you begin the restoration process?
- Is a provisional restoration needed?
- If a provisional is used, how long do you keep the patient in a temporary?
The scope of this bodyicle cannot adequately answer all of these questions. Rather, 1 case (e.g., the extraction and replacement of a single hopeless central incisor with a dental implant) will demonstrate the options that were chosen to achieve an esthetic restoration. The replacement of a single tooth implant is one of the greatest challenges in restorative dentistry.4 The rationale for these decisions will be explored.
Case Presentation
The patient presented with a failing endodontically treated central incisor (Figure 1). The apicoectomy failed, and the tooth had an acute abscess and a fistula. Radiographically, she presented with a mutilated, shortened root (Figure 2). She expressed high cosmetic demands and refused to have her teeth prepared for a 3-unit bridge, or wear a removable pbodyial denture as a permanent solution.
The treatment plan was as follows:
- Extract, bone graft and provisionalize.
- Heal for 2 months.
- Place dental implant.
- Heal for 2 months.
- Expose implant and place a temporary healing abutment.
- Perform guided gingival growth (non-surgical gingival graft).
- Place permanent abutment and provisionalize.
- Modify the temporary to achieve soft tissue maturation.
- Take final impressions.
- Deliver the final restoration.
Extraction and Grafting
Step 1 requires an atraumatic extraction of the central incisor. The extraction site was degranulated. All soft issue was removed in order to favor the in-growth of new bone. A freeze-dried mineralized or demineralized bone graft was placed into the socket, and a bovine collagen plug was placed and closed with resorbable sutures (Figure 3).
The purpose of the graft is twofold: soft tissue in-growth is delayed and bone regeneration is favored; and the site plumped out, yielding a greater volume of tissue in which to place the implant in 2 months. The collagen membrane serves to maintain the graft and acts as a “poor man’s membrane” to retard epithelial down growth. While this is not the ideal form of bone regeneration, it does yield an increased amount of bone, especially in enclosed extraction site defects with intact labial plates, as seen in this patient.5
Heal for 2 Months
Healing was rapid once the infection was removed (Figure 4). At 2 months post-extraction, soft tissue maturation was achieved, and an adequate volume of bone existed for the placement of the implant (Figure 5). Note that the papillae adjacent to the extraction site were present despite the absence of contact points. This is due to sufficient bone to support the soft tissue. Delaying implant treatment for 2 months also allowed for soft tissue maturation. Since an immediate implant was not performed, primary closure at the time of extraction was not necessary. Therefore, a free gingival graft was not necessary, and there was no distortion of the gingival architecture in an attempt to achieve primary closure.
Dental Implant Placement: Incision Design and Implant Alignment
The radiograph taken at 2 months post-extraction (Figure 6) revealed adequate bone in a mesial-distal and occlusal-apical direction. Bony fill was intimated in the space previously occupied by the tooth root. Given the excellent healing response of the patient, it was decided to proceed with dental implant placement.
The incision design enabled visualization of the buccal plate, without causing gingival recession over the adjacent teeth or papillary loss. A vertical incision was made over the interradicular bone, 1 tooth distal to the implant site (Figure 7a and Figure 7b). A sharp incision was made perpendicular to the bone, extending from the alveolar mucosa to the height of gingiva of the adjacent tooth. A secondary incision began at a right angle to the vertical incision and continued into the sulcus of the tooth adjacent to the implant site. The incision was carried interproximally into the sulcus to the palatal line angle of the tooth. At the palatal line angle, the incision made a 90° turn to connect horizontally with the palatal line angle of the other tooth adjacent to the implant site (Figure 8). The incision was carried intrasulcularly through the interproximal and buccal sulcus. If necessary, a second vertical incision could have been made in the same place on the contralateral side. This would only be necessary when extensive bone grafting, visualization, and reflection are required.
Following completion of the incision to bone, a full-thickness flap was reflected buccally. Full-thickness flap reflection was necessary to visualize bony anatomy. Without flap reflection, fenestrations and dehiscences go undiagnosed, leading to less bone-to-implant contact. The opportunity to graft these areas at implant surgery is lost if a flap is not elevated. It is the author’s opinion that flapless surgery is difficult and rarely indicated because it “handcuffs” the surgeon and frequently results in less than optimal regenerative treatment.
Implant placement requires a 3-dimensional mindset: mesial-distal, buccal-palatal and occlusal-apical.6, 7
Mesial-distal
The gingival zenith (i.e., most apical point of gingival tissue) of the maxillary central incisors is located distal to the long axis of the tooth.8 Therefore, placement of the maxillary central incisor is slightly distal to the midline of the tooth. Also, the nasal palatine foramina frequently dictates distal placement to avoid hitting the nerve. The clinician should attempt to keep the implant 1.5 mm to 2.0 mm from adjacent teeth (Figure 7a, Figure 7b and Figure 8) so that bone may be preserved, leading to retention of the papillae.7,9
Buccal-palatal
Ideal implant placement is slightly palatal to the palatal-incisal line angle (Figure 8). This creates a proper buccal emergence profile. If the implant is angled palatal to this line, a ridge lap restoration may be necessary. Conversely, angling the implant too labially will result in a loss of labial gingival height and an uneven gingival margin.
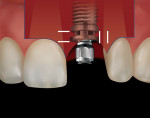
Occlusal-apical
Ideal position is 3 mm to 4 mm from the “anticipated” dento-gingival junction (Figures 7a and 7b).10 This provides room to develop a proper emergence profile, or running room. Deeply placed implants are difficult to clean and may trap debris or excess cement. Shallow implants are at risk of exposure and may not allow adequate space for a properly formed restoration.
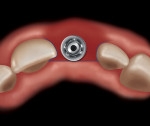
Second-stage Surgery
The implant was allowed to heal for 2 months before exposure. Second-stage surgery presents the surgeon with an opportunity to increase tissue thickness, increase keratinized gingiva and provide proper ridge contour. The incision connected the interproximal-palatal line angles of the adjacent teeth and extended interproximally (Figure 9a, Figure 9b and Figure 10). This allowed the flap to be raised buccally, creating additional gingival tissue without the need for a gingival graft. A titanium temporary healing abutment was placed, and the gingiva was pulled coronal to the abutment and secured with 2 resorbable (gut) sutures (Figure 11).
Guided Gingival Growth
Titanium is “gingiva loving”. Gingiva will grow to completely cover a titanium temporary healing abutment if placed slightly coronally (Figure 12). This technique is used when gingival tissue is desired (Figure 11 and Figure 12). The author has called this a “non-surgical gingival graft” because the body creates additional gingiva without the need for performing gingival surgery. A certain amount of recession is anticipated the first year after the implant restoration.11 Therefore, it is recommended to over build up the gingival tissue by 25%.12 It is always easier to subtract than to add.
Permanent Abutment Placement and Provisionalization
Four weeks after uncovering the implant and “non-surgical gingival grafting,” an implant level impression was taken, and a gold GingiHue™ Post (Implant Innovations Inc, Palm Beach Gardens, Florida) was fabricated (Figure 13). A provisional restoration was made and cemented with temporary cement (Figure 14).
Modification of the Temporary to Achieve Soft Tissue Maturation
All implants in the esthetic zone are provisionalized, which enables the clinician to refine the esthetics prior to fabricating the final restoration. The patient also has the opportunity to approve the restoration at this time. Acrylic can be added or subtracted in an attempt to guide the formation of the papillae and develop the proper emergence profile. A papilla will form if the contact point of the provisional is within 4 mm to 5 mm of the alveolar bone (Figure 15).7,13 It is not uncommon to keep the patient in the provisional for 3 months before the final impression is made.
Delivery of the Final Restoration
The final restoration was a recapitulation of the provisional restoration. A comparison of the final restoration to the initial tooth revealed little difference in shape and soft tissue architecture (Figure 1, Figure 16 and Figure 17). One month after the placement of the final restoration, excess labial gingiva was seen on the implant restoration when compared to the contralateral natural central incisor (Figure 16 and Figure 17). At 1 year, if the patient is not satisfied with the excess gingival tissue, it can be easily removed to achieve symmetry.
Conclusion
This case serves as a guide by which to perform an ideal esthetic maxillary central incisor implant restoration. The concepts provided are proven and supported by both clinical experience and evidence-based literature. However, there are many treatment alternatives available today that would have achieved a similarly satisfactory esthetic result, and there are advantages and disadvantages to each. Each treatment scenario presents unique challenges and opportunities for clinicians to serve our patients with ideal esthetic, functional and long-lasting implant dentistry. It is up to the individual clinician to explore the various treatment options and decide which works most predictably and easily so that patients will be better served.
References
1. Adell R, Eriksson B, Lekholm U, et al. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants. 1990;5(4):347-359.
2. Priest, G. The economics of implants for single missing teeth. Dental Economics. 2004;94(5):130-8.
3. Sonick M. Bone sculpting to achieve papilla regeneration around dental implants. Contemp Esthet Restor Pract. 2002;6(6):46-53.
4. Jansen CE, Weisgold A. Presurgical treatment planning for the anterior single-tooth implant restoration. Compend Contin Educ Dent. 1995;16(8):746-61.
5. Fugazzotto P. Treatment options following single-rooted tooth removal: a literature review and proposed hierarchy of treatment selection. J Periodontal. 2005;76(5): 821-31.
6. Sonick M. Hard and soft tissue regeneration for implants in the esthetic zone. Contemp Esthet Restor Pract. 2001;5(10):64-76.
7. Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Peridontics Restorative Dent. 2005;25(2): 113-19.
8. Rufenacht CR. Fundamentals of Esthetics. Chicago: Quintessence Pub Co. 1990;127.
9. Esposito M, Ekestubbe A, Grondahl K. Radiographic evaluation of marginal bone loss at tooth surfaces facing single Branemark implants. Clin Oral Implants Res. 1993; 4(3):151-7.
10. Parel S, Sullivan D. Esthetics and Osseointegration. Osseointegration Seminars, Inc. Dallas: Taylor Publishing Company; 1989.
11. Small PN, Tarnow DP. Gingival recession around implants: a 1-year longitudinal prospective study. Int J Oral Maxilofac Implants. 2000;15(4): 527-32.
12. Jovanovic SA, Paul S, Nishimura R. Anterior implant-supported reconstructions: a surgical challenge. Pract Periodontics Aesthet Dent. 1999;11(5):551-8.
13. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontal. 2000;71(4):546-9.
About the Author
Michael K. Sonick, DMD
Diplomate, American Board of Periodontology
Private Practice of Periodontics and Dental Implants
Fairfield, Connecticut