Dental Treatment Issues for Patients With HIV/AIDS
Margaret I. Scarlett, DMD
Today, HIV/AIDS is being managed by medical and dental teams as they manage other chronic diseases. This article—the second part of a two-part series for dental assistants on AIDS—addresses the care and treatment of persons known to be infected with HIV/AIDS. This second article provides a thumbnail description of treatment issues for patients with HIV/AIDS and a body of resources for the dental team to review about the constantly changing issues in current medical treatment modalities for HIV/AIDS. Special oral conditions and the available evidence on appropriate treatments for conditions associated with HIV/AIDS are reviewed. Finally, because drug treatment, treatment monitoring, and the progression of illness varies among individuals living with HIV/AIDS, a customized approach to the spectrum of care is recommended, in consultation with the patient’s physician or case manager.
Medical Treatment for HIV/AIDS
Today, HIV is managed as a chronic disease, with impressive results. For example, the impact of highly active antiretroviral therapy (HAART)—also called ARV or antiretro-viral therapy—is dramatic. The number of deaths from AIDS declined rapidly by 43 percent between 1995 and 1997 when these drugs were introduced.1 Current estimates are that with proper treatment, persons living with HIV can survive up to 23 years and beyond.1 Therefore, it is reasonable that persons living with HIV would seek routine dental care and palliative care for conditions associated with HIV or declining immunity. The decrease in deaths and the large number of people living with HIV/AIDS (PLWHAs) means that more patients are living with AIDS.1
Dental team members should know that HAART or ARV therapy controls HIV infection only when combination drug therapies are used consistently, monitored, and appropriately prescribed. Oral healthcare providers can ask about drug regimens and note this on the chart if patients disclose their HIV status confidentially. It is important that PLWHA follow nearly complete adherence to prescribed drug treatments to receive the optimal benefit of drugs and prevent drug resistance. If drugs are not taken daily, the virus may change, as it self-replicates, resulting in drug resistance. Many of the drugs are taken throughout the day with multiple pills taken at several times. The dental team can reinforce the message to take drugs as prescribed, consistently and correctly.
Unfortunately, one-third of people infected with HIV/AIDS have either not been tested, or are unaware of their status because they did not obtain their test results.2 Only two-thirds of people living with HIV/AIDS are aware of their status, and fewer than half of these people are taking advantage of effective antiretroviral therapy.
More than 20 drugs have been approved by the Food and Drug Administration for treatment of persons living with HIV/AIDS. Usually, the drugs are given in combination, targeting different parts of the lifecycle of the virus. Each of these drugs has a variety of side effects. Treatment of HIV is extremely complex and best managed by a physician specializing in infectious diseases. On November 3, 2008, the Department of Health and Human Services revised the drug treatment recommendations for HIV3. At the time of this writing, drug treatments, based on patient needs, included combinations of the following: 8 nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs/NtRTIs), 4 nonnucleoside reverse transcriptase inhibitors (NNRTIs), 10 protease inhibitors, a single fusion inhibitor, an entry inhibitor (maraviroc), and an integrase inhibitor (raltegravir) available for the treatment of HIV infection. However, because of selected drug toxicities and reactions in some persons, drug resistance issues, and the rapidly changing nature of the virus, new drugs and new strategies continue to emerge. Check with your local infectious disease specialist for the latest trends in HIV care and updates on treatment.
Individuals with HIV should be in the care of a licensed health care provider, preferably one with experience treating people living with the virus. Internal medicine practitioners and infectious disease specialists can give patients important, up-to-date treatment information and guidance.3 In addition, the entire dental team can assist in providing support to patients by working in conjunction with the primary care provider and even the case manager or patient navigator.
To assist healthcare professionals, the Health Resources and Services Administration (HRSA) has published A Guide to Primary Care for People with HIV/AIDS4. It covers a comprehensive range of topics, from basic elements of care to where additional sources of information can be found to help providers keep up to date on the latest therapies and drugs. HRSA also publishes and constantly updates guidelines for antiretroviral treatments. A Pocket Guide to Adult HIV/AIDS Treatment, February 20065 (available at hab.hrsa.gov/tools/HIVpocketguide/index.htm) includes drug information and occupational HIV postexposure prophylaxis issues. Should someone on the dental team accidentally incur a needlestick or puncture wound from an instrument used to treat a person with HIV, immediate referral and management of this exposure is necessary, as explained in this document. At a minimum, HAART for a month under a physician’s supervision is recommended to prevent infection for health workers.
Common Oral Conditions Associated with HIV/AIDS
Common oral conditions found in persons who are HIV-positive include a host of conditions. While PLWHAs often develop oral health issues similar to those encountered by healthy people, there are some conditions that occur concomitantly with HIV/AIDS infection. The science of the relationship between oral-systemic health and HIV progression has not been fully explored: science arrives at partial answers slowly, and this is certainly true for HIV and oral health issues.
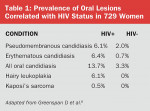
The exact range and timing of any oral conditions in the progression of HIV is not fully known. However, the best science is from cohorts of prospective epidemiologic studies.6 For example, researchers correlated oral health with other features of HIV disease among 729 women. Baseline oral examinations were performed by dental clinicians on 577 HIV-positive and 152 HIV-negative women. There were significant differences between the infected and uninfected women for certain oral lesions (see Table 1).6 Among the women who were HIV-positive, the presence of oral candidiasis was associated with CD4 cell counts below 200, cigarette smoking, and heroin/methadone use. A high viral load of HIV was associated with hairy leukoplakia.6
Some of these common conditions associated with HIV infection are listed in Table 2. Since early in the epidemic, oral lesions have been identifiers for HIV/AIDS, including oral candidiasis, oral hairy leukoplakia, severe herpetic ulcers, and oral Kaposi’s sarcoma.
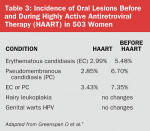
Data on oral lesions with HAART is still in progress: it is important to remain current with the literature on this topic. The same study of women with HIV mentioned above was analyzed after HAART initiation.7 In the analysis, new oral lesions with erythematous candidiasis (EC), pseudomembranous candidiasis (PC), hairy leukoplakia (HL), and warts were computed in follow-up visits. The authors compared conditions after HAART initiation with those before HAART initiation. There was a significant decrease in candidiasis after HAART initiation7 (see Table 3). Higher viral loads were associated with greater likelihood of candidiasis and HL, but not warts. Analysis of these data indicates that recurrence and incidence of candidiasis are reduced by HAART, and that recurrence is reduced independently of CD4 and HIV-RNA.
HIV Testing
How do you know if a person is infected with HIV? The answer is: if they have a test and disclose this to you with the medical history. Because of new test procedures, testing is more widely available. In 2006, new guidelines on testing and counseling from the Centers for Disease Control and Prevention promote testing in healthcare and non-medical settings.2 Many people do not know that they are infected with HIV, although knowledge of test status is essential to receiving the benefits of available treatments. However, even when patients know their test results, they might not disclose them to the dental team for fear of stigma, discrimination, or loss of confidentiality.
Types of HIV Tests
According to the CDC, “The standard screening test used in the United States to detect the presence of HIV antibodies is the EIA (enzyme immunoassay).” This test is performed on blood drawn from a vein. If the EIA is positive (reactive), it must be followed by a second confirmatory test, such as the Western blot, to make a positive diagnosis.1
EIA tests that use body fluids other than blood to screen for HIV antibodies include the following:
- Oral Fluid Tests use oral fluid (not saliva) collected from the mouth using a special collection device. This is an EIA antibody test similar to the standard blood EIA test and requires a follow-up confirmatory Western blot using the same oral fluid sample.
- Urine Tests use urine instead of blood. The sensitivity and specificity (accuracy) are somewhat less than that of the blood and oral fluid tests. Urine tests use an EIA antibody test similar to blood EIA tests and require a follow-up confirmatory Western blot using the same urine sample.1-3
Rapid test is a screening test that produces very quick results. This is not a confirmatory test, but a screening test that takes 20-60 minutes with blood or oral fluids. In addition, there are home collection test kits available in some consumer outlets for purchase. The patient collects blood from a finger prick or saliva and mails the kit into a laboratory for testing. Results are requested through a customer identification number assigned to each test kit. Regardless of the type of test, remember that testing should occur at least 2 to 8 weeks after any exposure to detect sufficient quantities of antibodies.2
Results Management and Data Storage
Positive or negative HIV test results should be documented in the patient’s confidential medical record and should be readily available to all healthcare providers involved in the patient’s clinical management. HIPAA guidelines should be followed at all times. It is not recommended that the HIV status of the patient be written on the outside of the record.2 Check with your state and local regulations or state board of dentistry for requirements in this regard.
Dental Treatment for Persons Living with HIV/AIDS
Immunosuppression for patients with HIV is a critical factor associated with oral lesions.6,7 As with other immunosuppressed patients, such as cancer patients, proper nutrition is important. For these patients, keeping them comfortable so that they can eat is very important, especially as many drugs must be taken in conjunction with food. Treating patients who have painful oral lesions with appropriate analgesics or medicines for oral lesions is especially important. Treat these lesions as you would for patients who are HIV-negative. In addition, you may wish to consider saliva enhancements or lemon drops for dry mouth, which may be a side effect of HAART.3 The appropriate treatment and prevention of Candida is especially important.8 Many dental offices refer hairy leukoplakia and Kaposi’s to an oral surgeon or oral pathologist for follow-up. Other periodontal conditions may require referral to a periodontist, if the severity of the condition cannot be managed in your office.
As with other issues, the science base for management of persons with HIV is still advancing as drug treatments evolve. It is clear that lower viral loads in patients who are on HAART are associated with fewer oral lesions.7 More information will be available over time as the science progresses. Although evidence based reviews by the Cochrane Collaboration are planned, they have not yet been released.8 The Agency for Healthcare Quality and Review contracted for an evidence based review of dental and medical literature in 2002 to determine the quality of evidence related to the management of dental patients who are HIV positive.9 The questions included whether:
- invasive but common dental procedures present added risk of complications for patients with HIV/AIDS;
- selected oral conditions are useful (A) markers of recent change in HIV serostatus or (B) indicators of immunosuppression; and
- specific available antifungal drugs can (A) efficaciously prevent or (B) effectively treat oral candidiasis.
In general, evidence-based information about the effectiveness of management of dental patients who are HIV-positive is uneven. There is lack of evidence that persons with HIV/AIDS have any greater risks from routine dental treatment, such as prophylaxis or restorations, than any other patients.9
There is fair evidence that two conditions (oral candidiasis and Kaposi’s sarcoma) are reasonable clinical indicators of severe immunosuppression based on their positive predictive values, and that another (oral ulcers) is not. The evidence is good that hairy leukoplakia is not a reasonable indicator of severe immunosuppression, even in a clinical setting.9
In reviewing the literature, only four studies addressed whether persons with HIV/AIDS are at greater risk of complications from specific invasive dental procedures than similar patients without HIV/AIDS. Invasive procedures were defined only as extractions and endodontics. This did not include a full range of services, such as orthognathic surgery, periodontal therapy, dental implants, prophylaxis, or root planing and scaling. The reviewers found insufficient evidence to judge the impact of endodontic treatment and the safety of extractions.9 More and better research is needed to address this question.
For this review performed in 2002, there was insufficient evidence that certain conditions, such as hairy leukoplakia, oral candidiasis, necrotizing ulcerative periodontitis, oral ulcers, or parotid swelling, could be markers of recent HIV seroconversion. There was evidence—judged as fair to good—that hairy leukoplakia and oral candidiasis are indicators of HIV infection.9
Regarding treatment of HIV-related conditions, there was insufficient evidence for the prophylactic effectiveness of treating any HIV-specific conditions, except fluconazole for oral candidiasis, among available antifungal agents. The evidence was judged to be good that fluconazole is effective in preventing new and recurrent episodes of oral candidiasis. The evidence was insufficient with regard to amphotericin B suspension as a treatment for oral candidiasis. Although all treatments were found to be effective, fluconazole and itraconazole seemed to be more effective than the other antifungals reviewed. The evidence of effectiveness was best for questions involved with prevention or treatment of oral candidiasis in persons who were HIV-positive. The evidence of effectiveness as a preventive treatment was good for fluconazole and nystatin, but insufficient for other antifungals. There was also good evidence of treatment effectiveness against oral candidiasis for fluconazole, itraconazole, nystatin, ketoconazole, and clotrimazole. Other studies indicate that managing candidiasis prophylactically10,11 with fluconazole makes patients more comfortable in obtaining adequate nutrition.
Conclusion
Today, HIV is a chronic disease that is carefully managed, much like other chronic diseases. Treatment of HIV by medical providers is complex and requires periodic adjustments over time. Following initial diagnosis of HIV by appropriate testing procedures, proper medical treatment will vary among patients. Current recommendations for medical treatment are continually revised as new medical research becomes available.
The dental team provides care to patients living with HIV/AIDS in consultation with the medical home for these patients. Many treatment issues for persons living with HIV/AIDS are similar to other patients; some unique oral conditions associated with HIV infection and immune compromised function have been summarized in this review. Common therapies for these conditions for prevention and treatment and the evidence to support their use were also reviewed.
References
1. Centers for Disease Control and Prevention. Fact sheets on HIV/AIDS. www.cdc.gov/hiv/resources/factsheets/.
2. Branson BM, Handsfield HH, Lampe MA, et al. Centers for Disease Control and Prevention. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep.2006;55(RR14);1-17. www.cdc.gov/mmwr/preview/mmwrhtml/rr5514a1.htm .
3. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1 infected adults and adolescents. Department of Health and Human Services. November 3, 2008. 1-139. Available at aidsinfo.nih.gov/contentfiles/AdultandAdolescentGL.pdf .
4. Health Resources and Services Administration. A Guide to Primary Care for People with HIV/AIDS. Rockville, MD: HRSA; 2004: 1-167.
5. Health Resources and Services Administration. A Pocket Guide to Adult HIV/AIDS Treatment. Rockville, MD: HRSA; 2006:1-57.
6. Greenspan D, Komaroff E, Redford M, et al. Oral mucosal lesions and HIV viral load in the Women’s Interagency HIV Study (WIHS). J Acquir Immune Defic Syndr. 2000;25(1):44-50.
7. Greenspan D, Gange SJ, Phelan JA, et al. Incidence of oral lesions in HIV-1-infected women: reduction with HAART. J Dent Res. 2004;83(2): 145-150.
8. Kuteyi,Teslim. Topical treatments for HIV-induced oral ulcerations. Title registered 26 April 2007. https://summaries.cochrane.org/CD007975/topical-treatments-for-hiv-related-oral-ulcers.
9. Bonito AJ, Patton LL, Shugars DA, et al. Management of dental patients who are HIV-positive. Evidence Report/Technology Assessment No. 37 (Contract 290-97-0011 to the Research Triangle Institute-University of North Carolina at Chapel Hill Evidence-based Practice Center). AHRQ Publication No. 01-E042. Rockville (MD): Agency for Healthcare Research and Quality. March 2002.
10. Goldman M, Cloud GA, Wade KD, et al. A randomized study of the use of fluconazole in continuous versus episodic therapy in patients with advanced HIV infection and a history of oropharyngeal candidiasis: AIDS Clinical Trials Group Study 323/Mycoses Study Group Study 40. Clin Infect Dis. 2005;41(10):1473-1480.
11. Cauda R, Tacconelli E, Tumbarello M, et al. Role of protease inhibitors in preventing recurrent oral candidiasis in patients with HIV infections: a prospective case control study. J Acquir Immune Defic Syndr. 1999;21(1): 20-25.
Web Resources
- Centers for Disease Control and Prevention (CDC): www.cdc.gov/hiv
- Food and Drug Administration (FDA), Center for Biologics Evaluation and Research (information on HIV testing): www.fda.gov/cber/products/testkits.htm
- HIVDent (basic information about dentistry or items related to dental treatment and HIV): www.hivdent.org
- Health Resources and Services Administration (HRSA), HIV/AIDS Bureau: www.hab.hrsa.gov
- National HIV and STD Testing Resources: www.hivtest.org or call the CDC at 1-800-CDC-INFO (232-4636), 1-888-232-6348 (TTY)
- National Institutes of Health (NIH): www.niaid.nih.gov/publications/aids.htm and https://www.nih.gov/about/discovery/infectiousdiseases/hiv.htm
About the Author
Margaret I. Scarlett, DMD
President
Scarlett Consulting International
Atlanta, Georgia