Digital Technology and the Future of Dentistry
Using cutting-edge production methods to create industry-leading restorations
We are currently experiencing a very exciting time for dental laboratory owners and professionals. New technology is being developed on a consistent basis, simplifying workflows and digitizing an industry that formerly existed on a purely analog level. As an industry, we are just beginning to incorporate and adopt digital technologies into our daily production flows; when combined with newly available, innovative materials, these technologies will ultimately improve productivity and offer a better experience for patients.
As the cost of laboratory work becomes a major factor in production, some forward-thinking laboratories are adopting digital processes to minimize costs and set themselves apart from the competition. In addition, as dental laboratory professionals continue to improve practices and procedures, manufacturers continue to innovate and develop the next generation of products, systems, and technologies to aid in this improvement of dental products. Products designed with computer software have become commonplace, and many laboratories now have access to 3D printing technology, whether in the laboratory or via production centers. Among the benefits of working with 3D printing technology are access to new, almost defect-free, industrially prefabricated and controlled materials; higher quality and reproducibility; data storage commensurate with a standardized chain of production; and improved precision planning and efficiency.
Historically, removable dies were part of the work process required to fabricate gypsum models. Dies were cut out separately in order to view the margin line against a separated element. However, with the introduction of CAD/CAM dentistry came new production techniques, as well as fresh challenges. For example, when a laboratory creates dies using 3D printing technology, a large mass of these dies are printed in one tray. This means that someone needs to clean them, label them, identify which die belongs to which model, and ensure that each die is properly attached to its model. In mass production dental laboratories, it was learned that a separated die is an integral part of the validation process; however, it does not necessarily have to be removable. If a 3D printed stone model includes the die as a built-in element, and a removable die will be attached to this model, the industry can progress to the next stage of production simplicity.
A Game Changer
In this particular case, the patient had worn dentition, defective amalgam restorations, and visible cracks in some of the molars (Figure 1). The patient was aware of bruxism, but requested conservative treatment rather than a full-mouth reconstruction to rebuild the lost vertical dimension. A plan was developed to place full-coverage crowns where needed and replace some of the amalgams with direct composite fillings. Full-contour zirconia was chosen as the crown material based on its high strength, as well as its ability to provide the tooth-colored appearance that the patient desired. The fact that zirconia restorations require minimal reduction was also conducive to the treatment of a worn tooth with a short clinical crown.
Treatment began on the lower right quadrant. Teeth Nos. 28, 29, and 31 received new composite fillings. A composite core was placed in tooth No. 30, and the tooth was prepared for a full-contour zirconia crown (Figure 2). The clinician placed a gingival retraction cord to better reveal the margin for a digital impression, and the iTero® digital scanner (Align Technology, Inc., www.itero.com) was used to scan the operative quadrant, the opposing quadrant, and the patient’s bite. The resulting virtual model was evaluated on the monitor to ensure complete capture of data for an accurate restoration.
Designing and Manufacturing the Restoration
3Shape’s Dental Designer software (www.3shapedental.com) was used to enter the case, identify a crown for tooth No. 30, and digitally create both sectioned and unsectioned models. The open-format .stl scan file from iTero was then imported into Dental Manager (3Shape).
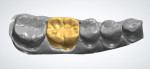
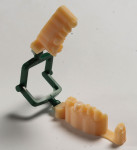
The Model Builder (3Shape) module was used to reorient the scan data, set the plane of occlusion, and identify prep tooth margins. After identifying the margins, the Model Builder software added bases to both arches. For the unsectioned model, a die was virtually extracted from the arch, and .stl files were generated for each model part—the operative arch, the opposing arch, and, in the case of the unsectioned model, the die (Figure 3). The crown was then designed using 3Shape design software (Figure 4) and milled and sintered overnight according to the material manufacturer’s recommendations.
For this case, a solid model, a detached die, and the opposing arch were generated. Current Model Builder software does not support this solution automatically, so a workaround was developed. The solid arch and detachable die were loaded into an industrial CAD software program (Figure 5). From there, a small rectangular shape was created and used to bridge the space between the solid arch and the detachable die (Figure 6). The three individual shapes were combined into one file (Figure 7) and sent to the Eden 260V printer for printing with other models (Figure 8). After sintering, the crown margins were finished to the printed detached die and contacts were finished to the solid model. The crown was stained, glazed, and delivered to the doctor for seating.
Seating
The Lava™ Plus (3M ESPE, www.3MESPE.com) zirconia crown was received from the milling center and evaluated on the model. The fit of the crown on the die was perfect, with no rock or rotation, and the margins were undetectable. Interproximal contacts on the solid model were broad and firm, as requested. Try-in of the crown in the mouth revealed undetectable margins and firm contacts identical to the solid model. After minimal occlusal adjustment, the crown was bonded with RelyX™ Ultimate Adhesive Resin Cement (3M ESPE) (Figure 9).
Conclusion
Digital dentistry is rapidly becoming the standard production tool for dental laboratories, offering the ability to cut production times, increase efficiency and accuracy, and enable new business growth. For dental laboratory owners and managers, choosing the right technologies to deliver the best return is not always so straightforward. The number of options available can be overwhelming, and learning new technology is often daunting.
At the heart of the new era in digital design is 3D printing. By combining oral scanning, CAD/CAM design, and 3D printing, dental laboratories can accurately and rapidly produce a vast range of dental and orthodontic appliances. With a 3D printing solution doing the detailed work, dental laboratories can eliminate the bottleneck of manual modeling and allow the business to expand and stay ahead of the competition.
The new production model concept presented by Stratasys’ 3D printing technology offers an innovative solution for printing models that addresses production issues that have prevented laboratories and milling centers from adopting this workflow. The detached die for margin finishing with the unsectioned solid model for contacts (Figure 10) simplifies the model design and construction, yet provides the details and precision that laboratories require (Figure 11). It is ideal for today’s monolithic-material milled restorations, and in the case presented, the accuracy of the new model concept was confirmed by the fit of the crown in the patient’s mouth.
Avi Cohen is the Director, Global Dental at Stratasys Ltd.
For more information, contact:
Stratasys Dental
P 800-801-6491
W www.stratasysdental.com
Disclaimer: The preceding material was provided by the manufacturer. The statements and opinions contained therein are solely those of the manufacturer and not of the editors, publisher, or the Editorial Board of Inside Dental Technology.