An Esthetic Makeover
Success utilizing technology-driven communication
Isam Estwani, DDS; Navneet Josan, DDS; and Joe Apap, CDT, TE, MDT
Creation of appealing facial characteristics is one of the primary elective goals of patients seeking dental care.1,2 The smile has a major impact on the perception of facial esthetics.3 Unfortunately, most of the time, dentists have limited themselves to the intraoral area. In reality, the restoration is just part of the process to create pleasing esthetics. Esthetic dentistry should not begin or end inside the lips. Teeth need to fit the entire framework of the face.4 The clinical ability to change the dentofacial form requires an understanding of facial beauty. This includes the evaluation of facial esthetics, proportions, and symmetry.5,6,7
Furthermore, communication of this vital information down the production process is critical to success. Every successful treatment plan has clear, streamlined communication behind it. The traditional process of writing down a prescription and drawing some illustrations has been replaced by advanced technology. The development of artificial intelligence-driven integrated practice/laboratory management platforms has streamlined the achievement of desired results in case planning. With communication, the dentist and the laboratory can efficiently achieve the targeted results without requiring extra appointments with the patient. Excellent communication also minimizes the cost of treatment, as well as the time spent by the dentist, the laboratory, and the patient. This approach to treatment is presented in the following case study.
Case Report
A 40-year-old female patient presented and expressed concerns about the appearance of her teeth. She reported that it was difficult to feel confident and smile openly. The patient expressed the desire for an esthetic smile makeover. Upon examination, significant apical dissymmetry was observed. This created an asymmetric appearance to the patient's smile. Also, the shade of the maxillary teeth visible in her smile was more than two shades darker than her mandibular anterior teeth. The patient's horizontal plane was also higher on her left side, as seen in the preoperative image (Figure 1).
Treatment Plan
After a thorough examination, laser gingivectomy was recommended at the time of the preparation based on the smile design work-up on teeth Nos. 4 through 13. This would be followed by the placement of layered lithium disilicate veneers (e.max®, Ivoclar) to restore her esthetically. The patient agreed to the treatment plan, and the procedure was scheduled. This treatment plan was conducted in two phases.
Phase one included the smile design work-up based on the corrections established in the clinical findings. The smile design was reviewed and the laboratory was approved to produce an esthetic wax-up. Lingual and facial reduction putty matrices were fabricated from the esthetic wax-up, along with clear reduction guides. A final silicone putty index was fabricated for chairside provisionalization. All scans, patient photos, and communications with the laboratory were done through the laboratory management platform (Cayster). Veneer preparations were done using the preparation guides and matrices provided by the laboratory. Finally, the veneer preparations were provisionalized using the silicone index provided, fabricated from the virtual diagnostic wax-up model.
Phase two included the fabrication and insertion of layered veneers.
Treatment Procedures
Preliminary photos and scans were taken and sent through the online platform for phase one of the procedure. It was determined that tooth No. 8 would be the guide for the proper gingival contour, length, width, and overall shape. Measurements were taken on tooth No. 8 and instructions sent to the laboratory. A smile design work-up was done at the laboratory based on the photos and preoperative scans (Figure 2). Smile design was submitted for review and approval (Figure 3). Once the smile design was approved, the clinicians requested the laboratory fabricate a set of lingual and facial matrices along with a clear reduction guide (Figure 4). A silicone putty matrix was fabricated using a model of the approved smile design for chairside provisionalization. The laboratory submitted the smile design within a few days and with a few minor adjustments, which were communicated directly on the laboratory management platform in real time. The case was able to quickly move toward the preparation and provisionalization stage.
Preparation and Provisionalization
The soft tissue recontouring was addressed first. The smile design plan ensured that the ideal proportions of length and width of restorations were maintained. The gingival recontouring of tooth No. 10 would be the most significant based on the clear reduction guide, which also showed the proposed gingival lines. The bone was sounded with a periodontal probe to establish that removing the soft tissue to the desired line would keep the margins 2.5 mm away from the bone, respecting the biological width. A diode laser was used for soft tissue recontouring. Once it was verified that the soft tissue was contoured to the clear index, preparation of the veneers could begin.
The silicone reduction guides were used as the preparation sequence for the veneering of teeth Nos. 4 through 13. Preparations were done on all 10 teeth. A 0.5-mm depth cutting bur was utilized across the facial surfaces of teeth Nos. 4 through 13, making horizontal cuts 4 mm apart. Then incisal reduction was made using a 1.5-mm depth reduction cutting bur. A KS0 diamond bur was used to prepare each tooth down to the cuts which the depth cutting burs had created, making certain to eliminate all sharp edges. A coarse grit diamond bur was used to start with gross cutting, and then a finer grit KS2 fine diamond bur was used for smoother preparation. The lingual and facial putty matrices were used to verify adequate reduction. Once verified, the patient was readied for the scanning of the preparations. Stump shades were taken and photo-documented for upload to the integrated platform that directly connected the dental office to the laboratory (Figure 5 and Figure 6). A latex-free lip and cheek retractor (OptraGate®, Ivoclar) was used for retraction, and retraction paste (Traxodent®, Premier Dental) was injected at the gumline of all the preparations and left on for 1 minute. Scanning was done using an intraoral scanner (iTero Element™, Align Technology).
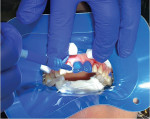
The provisionals were made chairside using an autocure provisional material (Luxatemp® [B1], DMG America) injected inside of the silicone index provided by the laboratory and seated fully in the patient's mouth over the veneer preparations (Figure 7). The final restoration shade established was VITA Bleachedguide 3D-MASTER® shade 0M2. A slightly darker shade was chosen for the provisionals, which was approved by the patient through the platform that managed all scans, which linked to the practice and the preferred laboratory. Instructions were sent regarding shade and layering of the veneers (Figure 8 through Figure 10). The patient was very happy with the outcome, as were the dentists (Figure 11).
Laboratory Procedures
The laboratory received this case on their integrated online laboratory management platform. The instructions were to create a smile design with specific requirements and submit for approval. Virtual smile design software (3Shape Smile Design, 3Shape) was used to import photos that were attached to the laboratory communication platform. The technicians then followed smile design protocol by plotting an interpupillary line and running a parallel line down to the incisal plane of the upper anterior teeth on a photo of the patient smiling broadly (Figure 12). These lines were then transferred to the preoperative scan of the patient (Figure 2). Additional lines were added showing various limiting heights and incisal lengths. Note the second vertical line from the top, in line with tooth No. 10, and the first vertical line, in line with tooth No. 9. Teeth Nos. 7 and 8 would have gingival contouring done to correct this asymmetry. Tooth No. 10 was in labial version and too long. Also, the smile line needed to drop down, starting from mid to distal of tooth No. 8 so that it would be symmetrical bilaterally to the bottom horizontal plane line. A smile design was created to correct the gingival dissymmetry and horizontal plane smile line, particularly on the patient's left. The laboratory respected the 11.5-mm length of tooth No. 8 and used the gingival height of tooth No. 7 as a limiting factor in establishing the proportions of the smile design. The laboratory submitted its design to the clinicians, and after a few minor adjustments were made through the instant messaging feature of the laboratory management platform, the design was finalized in a matter of minutes (Figure 3).
Once the smile design was approved, it was converted to STL format and sent to the 3D printer (Einstein™ 3D Dental Printer, Desktop Health). Also printed were the preoperative model and opposing arch for mounting on a semi-adjustable articulator (Panadent) using the facebow mounting jig sent from the practice. Magnetic plates were used, and both the smile design and preoperative models were split mounted to the opposing arch. Silicone matrices (Siltex) were made on the smile design model—one palatal matrix to show adequate incisal reduction and one facial matrix to show adequate reduction. A full coverage matrix (Siltex) was also produced for the dentist to use for chairside temporary fabrication. This was delivered to the dentist for the preparation and provisionalization phase.
The laboratory received the new preparation scan, provisional scan, and photos through the platform. There was no need to pull them from the scanner portal. Everything that was needed to continue with the case was there in the patient case file. Again, the smile design software was used to import the smile design and create individual veneers based on the preparation scan the clinician had sent. A virtual articulator was used to check for any lateral interference, a few simple adjustments were made based on the criteria set forth by the clinician, and the case was closed. The STL files that were created were sent to a mill (Roland DGA) to mill the wax to be used for pressing the lithium disilicate glass-ceramic (e.max, Ivoclar) in shade. A stump shade of ND3 was taken (Figure 15). A lithium disilicate ingot (IPS e.max® Press, Ivoclar) was chosen in LT BL1 shade to offset the darker stump shade. All margins were sealed on the printed model and dies of each veneer preparation. The wax-ups were then sprued and invested using a phosphate-bonded universal investment material (IPS® PressVEST, Ivoclar) investment and a 300 g ring. The ring was placed in a furnace (Programat EP5010, Ivoclar). After the pressing cycle was complete, the veneers were carefully divested and placed in a stone cleaner solution, and the ultrasonic was run for 5 minutes. The pressed veneers were then carefully separated from the sprues for final contouring, layering, staining, and glazing.
In the hands of the laboratory's master ceramists, the veneers were fitted to individual dies. Then the contacts were checked and adjusted where needed on the solid printed prep model.
Mounted on the articulator, the occlusion was checked in centric, lateral, and protrusive movements (Figure 13). Layering was accomplished by cutting back the incisal third of the veneers (Figure 14), creating mamelons, and adding shaded add-on material (IPS e.max Ceram Add-On Incisal, Ivoclar) for a more vital and lifelike appearance on teeth Nos. 6 through 11. Final staining and glazing were done to achieve the final 0M2 shade the clinicians and patient requested. Ivoclar Natural Die Material was used in shade ND2 to replicate the preparation shade for teeth Nos. 7 through 10, and shade ND3 was used to replicate preparation shade for teeth Nos. 4 through 6 and Nos. 11 through 14 (Figure 15). The final stain and glaze application was finished and checked using the ND2 and ND3 natural shaded dies (Figure 16). Add-on porcelain, staining, and glazing were done in another furnace (Programat P710, Ivoclar) using its preconfigured programs. After the veneers were cool, etching gel (IPS Ceramic Etching Gel, Ivoclar) was applied on the intaglio surfaces of the veneers to pre-etch. The clinician was instructed to refresh this etch when ready to seat the veneers.
Seating Appointment
After receiving the layered veneers from the laboratory and checking on the model, the clinicians prepared the patient for final seating. After removing the provisionals and thoroughly cleaning the area (Figure 17 through Figure 20), try-in paste (Variolink® II Try-In Paste, Ivoclar) was used to check the contacts and general esthetics of the veneers. A total etch was chosen for optimal bond strength, and bonding was accomplished by following a detailed protocol (Figure 21 and Figure 22). A final polish was performed with diamond-impregnated rubber points and cups (Figure 23). The patient was handed a mirror, and she was ecstatic with the results (Figure 24).
Outcome
The patient's reluctance to smile was immediately resolved after the provisional procedure. She was pleased with the appearance of her new smile. The areas of teeth Nos. 4 through 13 restored the patient's confidence and offered her an enhanced quality of life. The patient was advised to maintain proper oral hygiene practices, including brushing and flossing daily and attending regular dental check-ups to ensure the long-term success of the treatment. The patient has been seen several times since the final veneer seating, and she continues to say how happy she is.
The authors would like to acknowledge Town & Country Dental Studios in Freeport, New York, for their work on this case.
About the Authors
Isam Estwani, DDS
Fellow
Academy of General Dentistry
Private Practice
Herndon, VA
Navneet Josan, DDS
Member
Academy of General Dentistry
Private Practice
Woodbridge, VA
Joe Apap, CDT, TE, MDT
Technical Support Manager
CreoDent
New York, NY
References
1. Machado AW. 10 commandments of smile esthetics. Dental Press J Orthod. 2014;19(4):136-157.
2. Mack MR. Perspective of facial esthetics in dental treatment planning. J Prosthet Dent. 1996;75(2):169-176.
3. Havens DC, McNamara JA Jr, Sigler LM, Baccetti T. The role of the posed smile in overall facial esthetics. Angle Orthod. 2010;80(2):322-328.
4. Greenberg JR, Bogert MC. A dental esthetic checklist for treatment planning in esthetic dentistry. Compend Contin Educ Dent. 2010;31(8):630-638.
5. Shah R, Nair R. Comparative evaluation of facial attractiveness by laypersons in terms of facial proportions and equate it’s deviation from divine proportions - a photographic study. J Oral Biol Craniofac Res. 2022;12(5):492-499.
6. Apa M. Facial esthetics—the framework. Inside Dentistry. 2012;8(2):60-67.
7. Pisulkar S, Nimonkar S, Bansod A, et al. Quantifying the selection of maxillary anterior teeth using extraoral anatomical landmarks. Cureus. 2022;14(7):e27410.