Dens Invaginatus: A Case Report
Shantanu Choudhari, BDS, MDS; Saurabh R. Joshi, BDS, MDS; Namrata Patil, MDS; and Sai Kalyan, BDS, MDS
Abstract
Dens invaginatus, also known as dens in dente, is a rare anomaly affecting human dentition. The condition results in invagination of an amelodental structure within the pulp. This case report discusses the current management protocol of dens invaginatus as demonstrated in an adolescent female and describes treatment options. As with most conditions, early diagnosis and preventive measures help minimize complications in dens invaginatus cases.
Dens invaginatus, also known as dens in dente, is an anomaly of the tooth formation of embryologic origin. The condition results in invagination of an amelodental structure within the pulp. On radiographic evaluation, the deformation scan sometimes look like a tooth within a tooth, which explains the nomenclature dens in dente.1 Other names are invaginated odontome, dilated gestant odontome, dilated composite odontome, tooth inclusion, and dentoid in dente.2
Radiographic examination will show an infolding of enamel and dentin that may extend deep into the pulp cavity, root, and even the root apex.3 Ploquet first described this malformation in 17943 based on observations of the condition in a whale’s tooth.4
Hovland and Block4 estimated the incidence as 0.04% to 10%, possibly occurring in any tooth, affecting either deciduous5 or permanent dentition6 and commonly involving the upper lateral incisors.6,7 Bilateral occurrence has been reported in some patients,8-11 meaning that the affected tooth’s homologous counterpart should also be inspected for signs of the condition. Rarely, dens invaginatus is found in molars,11 premolars,12 and maxillary central incisors.13 It occurs in maxillary lateral incisors in 43% of all cases.14 The cause for dens invaginatus is unclear; however, some evidence suggests a hereditary component.15
This report describes a case of unilateral dens invaginatus associated with the maxillary lateral incisor.
Case Report
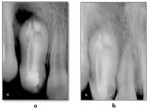
A 13-year-old female was referred to the Department of Pedodontics and Preventive Dentistry at Rural Dental College and Hospital in Loni, India, with a chief complaint of past swelling in the upper right front of the jaw. The patient described diffuse swelling in the right front of the cheek, which had resulted in elevation of the ala of her nose. On intraoral examination, a deep pit was observed in the permanent maxillary right lateral incisor with slight discoloration of the crown, and the tooth responded positively to vertical percussion. Examination of a preoperative radiograph showed the presence of dens invaginatus of the maxillary right lateral incisor with an apical radiolucent area (Figure 1A). A diagnosis of type III (Oehlers) dens invaginatus with dentoalveolar abscess was made. The patient had a noncontributory medical history.
Intraoral periapical radiographs were taken, and computed tomography scans were performed. Examination of the computed tomography scans revealed a complex anatomy of the tooth with multiple canals. The distal canal was C-shaped, opening medially. The palatal canal opening was at the distal side, and a central canal went as far as the depth of central invagination (Figure 1B and Figure 1C).
Magnifying loops were used to help locate the canals, and access to the pulp chamber was made. A No. 10 K-flex file was inserted, and radiographs were obtained. The working length was determined with No. 10K (Figure 1D), and the canals were cleaned and shaped with a No. 35 K file. Because the apical area of one canal was difficult to treat conventionally, apical surgery was planned for retrograde mineral trioxide aggregate placement with thermoplastisized gutta-percha obturation. Findings from routine blood tests were within normal limits. At a subsequent appointment, the tooth was prepared for surgical treatment. A full-thickness mucoperiosteal flap was reflected, and a fenestration on the cortical plate was noted at the level of the periradicular lesion (Figure 1E). After complete curettage of the soft tissue was performed and followed by removal of granulation tissue, a facial bevel was made at the tooth apex. After thorough cleaning, white mineral trioxide aggregate (ProRoot®, DENTSPLY, www.denstply.com) retro-filling (Figure 1F) was used, followed by obturation using thermoplasticized gutta-percha (Endo@pex, Cordless Obturation System, DXM, Korea, www.dxm.co.kr) (Figure 2A). A 5-0 blade silk suture was used to place the flap.
At the 1-week follow-up visit for suture removal, the tissues were noted to be healing uneventfully. At 1.5 months post-treatment, the patient had no symptoms. Signs of hard-tissue healing in the periradicular area could be appreciated on the radiographic examination (Figure 2B). Follow-up radiographic scans taken 6 months later showed evidence of complete healing.
Discussion
Dens invaginatus is the result of an invagination of one portion of a tooth into the other; it is not a twin formation, but a malformation of only one tooth germ.16 In 1957 Oehlers17 created a classification system of these malformations according to severity: type I, confined within the crown; type II, blind sac extending beyond the cementoenamel junction with second foramen extending into the periradicular tissues, and type III with second foramen in the apical area.
Explanations for the etiology of dens invaginatus malformation are controversial and remain unclear. For decades researchers have been proposing theories to help address this. Some have suggested that growth pressure of the dental arch leads to the enamel organ buckling.1,18 Kronfeld19 postulated a focal failure of growth of the internal enamel epithelium while the surrounding normal epithelium continues to proliferate and engulf the static area. Rushton20 proposed rapid and aggressive proliferation of part of the internal enamel epithelium invading the dental papilla. He called this a “benign neoplasm of limited growth.” Oehlers17 suggested a distortion of the enamel organ during tooth development. He noted that subsequent protrusion of a part of the enamel organ leads to the formation of an enamel-lined channel ending at the cingulum or occasionally at the incisal tip. The latter may be associated with irregular crown form. The twin theory21 suggested a fusion of two tooth germs. Gustafson and Sundberg22 thought trauma may be a cause but could not provide sufficient explanation as to why just maxillary lateral incisors were affected and not central incisors.
Early diagnosis of dens invaginatus is crucial and requires thorough clinical examination of all teeth, especially lateral incisors. The examination should check for the presence of palato-radicular groove and deep pits on the palatal surfaces of maxillary anterior teeth, particularly the lateral incisors. The present condition can be seen as soon as the maxillary anterior teeth erupt in the oral cavity by the age of 7 to 10 years. The condition can be diagnosed based on clinical and radiographic findings. The invagination provides a place for bacterial growth and may endanger the integrity of the main canal. Early detection and sealing of the invagination’s opening with acid-etch resin can effectively prevent these complications.23,24 If no entrance to the invagination can be detected and no signs of necrosis are visible clinically and radiographically, no treatment is indicated. However, strict observation is recommended.25-27
Rendering root canal treatment may present several problems because of the irregular shape of the root canal system. (Identification of root canal orifices and complex irregular morphology of root canals makes the treatment difficult.) If no radiographic signs of pulp necrosis are present and no communication exists between the invagination and root canal, a composite or amalgam filling of the invagination will be adequate.28 Root canal treatment is indicated when the invagination has a separate apical or lateral foramen,29 as in the present case report. In some situations, burring through the invagination to reach the apical foramen may be possible. When minor forms of invaginations are eliminated, root canal treatment typically will not present further problems. Fore example, if the invaginations are minor, burring through the invagination reduces the chance of lateral perforation and, hence, the root canal treatment of such teeth can be carried out more easily. Sometimes, the invagination must be treated as a separate root canal.30,31 In the present case, the invagination was left for two important reasons. The first reason was the invagination was thick and its removal would have weakened the tooth structure. The second reason was the inadequate length of bur and insufficient accessibility to the invagination. As a result, the canal in the invagination was treated as a separate canal, and we performed root canal treatment.
Because of the enamel invagination, the dens invaginatus filling has a wide and bulky cavity, requiring an obturation with filling material. The use of thermoplasticizing techniques can facilitate the procedure and provide a more efficient sealing,23 as was accomplished in the present study.
Surgical treatment should be considered in certain cases. These would include endodontic failure and in teeth that cannot be treated nonsurgically because of anatomic problems or failure to gain access to all parts of the root canal system.24,31 In the present case, apical surgery was conducted in order to access the untreated apical one-third of the root, and apical sealing was performed using white mineral trioxide aggregate.
Extraction can be indicated only in teeth that have severe anatomic irregularities that cannot be treated nonsurgically or by apical surgery and in some cases of supernumerary teeth. Extraction is also suggested when abnormal crown morphology creates esthetic or functional problems.23
Conclusion
Early diagnosis and preventive measures are helpful to prevent complications in dens invaginatus cases. Because of the complications presented by dens invaginatus type III and a chronic periapical lesion, a combined nonsurgical and surgical endodontic therapy was indicated in this case.
References
1. Atkinson SR. The permanent maxillary lateral incisor. Am J Orthod. 1943;29(12): 685-698.
2. Hülsmann M. Dens invaginatus: aetiology, classification, prevalence, diagnosis, and treatment considerations. Int Endod J. 1997;30(2):79-90.
3. Shafer WG. Dens in dente. N Y State Dent J. 1953;19:220-225.
4. Hovland EJ, Block RM. Nonrecognition and subsequent endodontic treatment of dens invaginatus. J Endod. 1977;3(9):360-362.
5. Mupparapu M, Singer SR. A review of dens invaginatus (dens in dente) in permanent and primary teeth: report of a case in a microdontic maxillary lateral incisor. Quintessence Int. 2006;37(2):125-129.
6. Caldari M, Monaco C, Ciocca L, Scotti R. Single-session treatment of a major complication of dens invaginatus: a case report. Quintessence Int. 2006;37(5):337-343.
7. Bimstein E, Shteyer A. Dilated type of dens invaginatus in the permanent dentition: report of a case and review of the literature. ASDC J Dent Child.1976;43(6):410-413.
8. Swanson WF, McCarthy FM Jr. Bilateral dens in dente. J Dent Res.1947;26(2):167-171.
9. Burton DJ, Saffos RO, Scheffer RB. Multiple bilateral dens in dente as a factor in the etiology of multiple periapical lesions. Oral Surg Oral Med Oral Pathol.1980;49(6):496-499.
10. Canger E, Kayipmaz S, Celenk P. Bilateral dens invaginatus in the mandibular premolar region. Indian J Dent Res. 2009;20(2):238-240.
11. Costa WF, SousaNeto MD, Pécora J D. Upper molar dens in dente—case report. Braz Dent J. 1990;1(1):45-49.
12. Girsch WJ, McClammy TV. Microscopic removal of dens invaginatus. J Endod. 2002;28(4):336-339.
13.Vasudev SK, Goel BR. Endodontic management of dens evaginatus of maxillary central incisors: a rare case report. J Endod. 2005;31(1):67-70.
14. Grahnen H, Lindahl B, Omnell K. Dens invaginatus. I. Aclinical, roentgenological and genetical study of permanent upper lateral incisors. Odontol Revy. 1959;10:115137.
15. Kitchin PC. Dens in dente. Oral Surg Oral Med Oral Pathol. 1949;2(9):1181-1193.
16. Erausquin R, Pellegrini AJ, Ponte JJR. Dens in dente. Revista Odontologica. 1932;20:537.
17. Oehlers FA. Dens invaginatus (dilated composite odontome). I. Variations of the invaginatus and associated anterior crown forms. Oral Surg Oral Med Oral Pathol. 1957;10(11):1204-1218.
18. Euler H. Die Anomalien, Fehlbildungen und Verstümmelungen der menschlichen Zähne. München, Germany: Lehmann; 1939:62-67.
19. Kronfeld R. Dens in dente. J Dent Res. 1934;14:49-66.
20. Rushton MA. A collection of dilated composite odontomas. Br Dent J. 1937;63:65-85.
21. Bruszt P. Über die Entstehung des ‘Dens in dente.’ Schweizer Monatsschrift für Zahnheilkunde.1950;60:534-542.
22. Gustafson G, Sundberg S. Dens in dente. Br Dent J. 1950;88: 83-88,111-122,144-146.
23. Rotstein I, Stabholz A, Heling I, Friedman S. Clinical considerations in the treatment of dens invaginatus. Endod Dent Traumatol. 1987;3(5):249-254.
24. Hülsmann M, Radlanski R. Möglichkeiten der konservativen therapie des dens invaginatus. Deutsche Zahnärztliche Zeitschrift. 1994;49:804-908.
25. Hülsmann M. Therapie des dens invaginatus. Schweizer Monatsschrift für Zahnmedizin. 1995;105:1323-1334.
26. Hülsmann M, Hengen G. Severe dens invaginatus malformation. Report of two cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82(4):456-458.
27. Duckmanton PM. Maxillary permanent central incisor with abnormal crown size and dens invaginatus: case report. Endod Dent Traumatol. 1995;11(3):150-152.
28. De Smit A, Demaut L. Nonsurgical endodontic treatment of invaginated teeth. J Endod. 1982;8(11):506-511.
29. Grossman LI. Endodontic case reports. Dent Clin North Am. 1974;18(2):509-527.
30. Cole GM, Taintor JF, James GA. Endodontic therapy of a dilated dens invaginatus. J Endod. 1978;4(3):88-90.
31. Harnisch H. Apicoectomy in dens in dente. Quintessence Int (Berl). 1970;1(3):21-22.
About the Authors
Shantanu Choudhari, BDS, MDS
Professor
Department of Pedodontics
Rural Dental College
Loni, India
Saurabh R. Joshi, BDS, MDS
Senior Lecturer
Department of Pedodontics
Rural Dental College
Loni, India
Namrata Patil, MDS
Former Post Graduate Student
Department of Pedodontics
Rural Dental College
Loni, India
Sai Kalyan, BDS, MDS
Senior Lecturer
Department of Conservative Dentistry & Endodontics
Rural Dental College
Loni, India