Using Computer-Guided Surgery for Partial Guidance of Zygoma Implants
Abstract
Patients with advanced atrophy of the maxilla benefit greatly from the use of dental implants. In the past, protocols recommended highly invasive bone grafting, which required months of maturation before implant placement. Over the past decade, zygoma implants have been used as an alternative procedure. While computer-guided surgery provides a great benefit, its use for complete placement of zygoma implants is not yet predictable. The following protocol provides a way to facilitate the placement of zygoma implants into the best position surgically and prosthetically using partially computer-guided surgery.
Extreme jaw atrophy poses a multitude of challenges prosthetically. Wearing removable dentures is a challenge for patients due to the lack of alveolar ridge support.1 Patients with advanced atrophy of the maxilla benefit greatly from the use of dental implants to provide stabilization of the prosthesis and better reduce painful soft-tissue irritation and embarrassing denture movements.
In patients with extreme atrophy of the maxillary arch, procedures involving extensive and highly invasive bone grafting to provide more bone volume for implant placement have been recommended over the years.2-5 Today sinus augmentation procedures are commonly used to provide bone under the floor of the maxillary sinus bilaterally to facilitate implant placement.3,6-11 These procedures often require months of bone graft maturation before implants can be placed. Bone grafts also have potential for infection and failure. Additionally, there is potential for donor site morbidity if autogenous bone is harvested from the iliac crest or other areas of the body.
Zygoma implants have been used for more than a decade as an alternative to sinus augmentation procedures.12-16 While computer-guided surgery provides a great benefit in implant placement,17-22 the use of a surgical template for complete placement of zygoma implants is not yet predictable or safe. The challenge of placing zygoma implants through a surgical template is related to the 45-degree angled head that not only makes the depth positioning of the implant critical, but also the timing pitch on the screw threads. There are also significant risks associated with drilling and placing an implant of that length in such close proximity to the orbit.
An open-flap technique and freehand placement is essential to providing safe and effective placement of zygoma implants. The following patient treatment approach demonstrates a way to facilitate the placement of zygoma implants into the best position surgically and prosthetically by partially guiding the zygoma implants.
Case Report
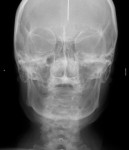
A 54-year old woman, who had been edentulous and wearing dentures for a total of 21 years (Figure 1 through Figure 3), presented with an interest in replacing her removable dentures with a fixed implant-supported reconstruction for both functional and psychological reasons. Her existing dentures, which were 7 years old, were deemed to be adequate from both an esthetic and functional perspective. She claimed to be in good health and a non-smoker, who had stopped smoking 6 years previously. The patient had a history of alcohol abuse, mitral-valve prolapse, some sinus trouble, headaches, and was hypothyroid. She was taking levothyroxine for her thyroid, amitriptyline for headaches, alprazolam when needed, and vitamin D daily.
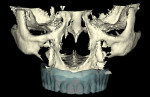
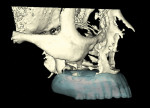
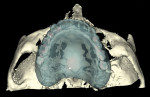
Ten radiopaque markers (gutta percha, Hygenic®, Coltène/Whaledent Group, www.coltene.com) were placed in the maxillary complete denture to prepare the denture for a specific guided- surgery protocol (NobelClinician™ Software, Nobel Biocare USA, LLC, www.nobelbiocare.com).23-30 This protocol uses a dual cone beam computed tomography (CBCT) scan procedure. The first CBCT scan (i-CAT®, Imaging Sciences International Inc., www.imagingsciences.com) was taken with the patient’s dentures in place, and a second CBCT scan was taken of the maxillary complete denture alone. The two scans were exported in Digital Imaging and Communications in Medicine (DICOM) format and loaded into the guided-surgery software, where a 3-dimensional (3-D) virtual working model of the patient was generated (Figure 4 through Figure 7) to enable virtual implant planning to be performed. Because the patient’s denture contained the approved esthetic arrangement of the teeth, the implants could be placed virtually in the most prosthetically favorable position.
A copy of the first CBCT scan was sent to an oral maxillofacial radiologist, and accomprehensive radiology report was generated. The findings were as follows: There was pneumatization of the great wing and pterygoid plates of the left sphenoid sinus, and severe atrophy was noted in both the maxillary and mandibular alveolar processes.
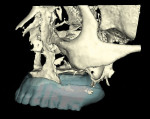
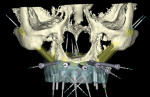
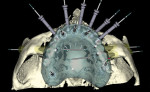
The finalized virtual implant plan (Figure 8 through Figure 12) consisted of two 10-mm implants and one 13-mm implant in the maxillary anterior region, which engaged the cortical bone at the inferior border of the nasal cavity. The plan called for two 18-mm implants to be placed in the pterygomaxillary31,32 region at an approximately 45-degree angle to the occlusal plane. These pterygomaxillary implants would provide posterior support for the restoration and eliminate a posterior cantilever.33-36 In order to shorten the span between the three anterior and two posterior implants, three zygoma implants were planned on the pre-surgica lcomputer model to transect through the sinus cavity and engage the zygoma bone. All implants in the virtual planning were external-connection regular-platform implants (Brånemark® System, Nobel Biocare).
Technique
The inability to precisely deliver zygoma implants through a surgical template in a clinical trial has delayed thecommercial release of hardware for guided zygoma implants. Therefore, while a surgical template could be fabricated for the five standard-length implants, it could not be fabricated for zygoma implants. In an effort to provide some benefit from the surgical-planning process and maximize the prosthetically driven nature of this protocol, the following technique was performed.
Once the zygoma implants were positioned virtually, the sizes of each zygoma implant were recorded and screenshots of the planning were taken. The virtual zygoma implants were then switched to standard-length implants in the exact same axis (Figure 13). The appropriate surgical template sleeve accompanied the standard-length implants, which could be incorporated into the surgical template. While these standard Brånemark sleeves would not permit actual zygomatic implant placement, they would enable the surgeon to create a starting point for the access of the zygoma position into the alveolar bone. This provided the ability to put the coronal aspect of the zygoma implant in the best prosthetic position, which is a tremendous advantage for laboratory construction of the final prosthesis. It also gives the surgeon an opportunity to study the 3-D anatomy of the patient prior to the surgery.
The standard-length implants were installed following the normal guided-surgery protocol.23-30 The pterygomaxillary implant on the patient’s left side had much higher primary stability than anticipated from the virtual planning; therefore, only one of the two zygoma implants was installed on that side. Then, using a 3-mm twist drill through the surgical template (Figure 14), the zygomatic implant entry through the alveolus into the sinus was made. The surgical template was then removed. A crestal-palatal incision was then made connecting the implants in the pterygomaxillary region and establishing the access points for the zygoma implants. A vertical releasing incision was made in the canine region. With the full flap reflected, Caldwell-Luc type sinus entry was made to then completely visualize the path of drilling for the zygoma implant. The implant was then placed freehand through the entry position marked by the template through the sinus and through the lateral wall of the zygoma bone. While the zygoma implant length used surgically via this partially guided approach may not be exactly the same length as the zygoma implant virtually planned, the advantage of knowing the ideal coronal position reduced the complexity of the implant placement and optimized the prosthetic orientation of the implant.
In this patient example, implants were placed both on the left and right side in the zygomatic area to provide additional support for the full, fixed, implant-supported restoration. While the five regular implants allowed for laboratory fabrication of a screw-retained, implant-supported, all-acrylic resin provisional prosthesis prior to surgery (Figure 15), the zygoma implants needed to be connected to the prefabricated provisional prosthesis using the Teeth In A Day® protocol (Pi Dental Center, www.pidentalcenter.com) (Figure 16).37,38 When the prosthetic cylinders for the zygoma implants were rigidly connected, the entire prosthesis was removed from the patient, and the area of connection was contoured and highly polished. The prosthesis was then redelivered to the patient at the same surgical session (Figure 17 through Figure 20). This patient will function with the all-acrylic resin provisional screw-retained prosthesis for approximately 3 months until the time of final impression. At that time, the final prosthesis construction will commence and the patient will present for final delivery a few weeks later.
Conclusion
The advantage of the partial guided zygoma technique is that it allows for a faster, safer, and more efficient surgical and prosthodontic procedure.
References
1. Tallgren A. The effect of denture wearing on facial morphology. A 7-year longitudinal study. Acta Odont Scand. 1967;25(5):563-592.
2. Isaksson S, Alberius P. Maxillary alveolar ridge augmentation with onlay bone-grafts and immediate endosseous implants. J Craniomaxillofac Surg. 1992;20(1):2-7.
3. Wood R, Moore D. Grafting of the maxillary sinus with intraorally harvested autogenous bone prior to implant placement. Int J Oral Maxillofac Implants. 1988;3(3):209-214.
4. Isaksson S, Ekfeldt A, Alberius P, Blomqvist J. Early results from reconstruction of severely atrophic (Class IV) maxillas by immediate endosseous implants in conjunction with bone grafting and Le Fort I osteotomy. J Oral Maxillofac Surg. 1993;22(3):144-148.
5. Barone A, Ricci M, Mangano F, Covani U. Morbidity associated with iliac crest harvesting in the treatment of maxillary and mandibular atrophies: a 10-year analysis. J Oral Maxillofac Surg. 2011;69(9):2298-2304.
6. McDermott NE, Chuang SK, Woo VV, Dodson TB. Maxillary sinus augmentation as a risk factor for implant failure. Int J. Oral Maxillofac Implants. 2006;21(3):366-374.
7. Garlini G, Redemagni M, Donini M, Maiorana C. Maxillary sinus elevation with an alloplastic material and implants: 11 years of clinical and radiologic follow-up. J Oral Maxillofac Surg. 2010;68(5):1152-1157.
8. Bernardello F, Righi D, Cosci F, et al. Crestal sinus lift with sequential drills and simultaneous implant placement in sites with <5 mm of native bone: a multicenter retrospective study. Implant Dent. 2011;20(6):439-444.
9. Özkan Y, Akoğlu B, Kulak-Özkan Y. Maxillary sinus floor augmentation using bovine bone grafts with simultaneous implant placement: a 5-year prospective follow-up study. Implant Dent. 2011;20(6):455-459.
10. Cricchio G, Sennerby L, Lundgren S. Sinus bone formation and implant survival after sinus membrane elevation and implant placement: a 1- to 6-year follow-up study. Clin Oral Impl Res. 2011;22(10):1200-1212.
11. Deppe H, Mücke T, Wagenpfeil S, Hölzle F. Sinus augmentation with intra- vs extraorally harvested bone grafts for the provision of dental implants: clinical long-term results. Quintessence Int. 2012;43(6):469-481.
12. Parel S, Brånemark PI, Ohrnell L, Svensson B. Remote implant anchorage for the rehabilitation of maxillary defects. J Prosthet Dent. 2001;86(4):377-381.
13. Bedrossian E, Stumpel L III, Beckley ML, Indresano T. The zygomatic implant: Preliminary data on treatment of severely resorbed maxillae. Int J Oral Maxillofac Implants. 2002;17(6):861-865.
14. Malevez C, Abarca M, Durdu F, Daelemans P. Clinical outcome of 103 consecutive zygomatic implants: A 6-48-months follow-up study. Clin Oral Implants Res. 2004;15(1):18-22.
15. Bedrossian E, Rangert B, Stumpel L, Indresano T. Immediate function with the zygomatic implant: a graftless solution for the patient with mild to advanced atrophy of the maxilla. Int J Oral Maxillofac Implants. 2006;21(6):937-942.
16. Boyes-Varley JG, Howes DG, Lownie JF, Blackbeard GA. Surgical modifications to the Brånemark zygomaticus protocol in the treatment of the severely resorbed maxilla: a clinical report. J Oral Maxillofac Implants. 2003;18(2):232-237.
17. Wittwer G, Adeyemo WL, Schicho K, et al. Navigated flapless transmucosal implant placement in the mandible: a pilot study in 20 patients. Int J Oral Maxillofac Implants. 2007;22(5):801-807.
18. Van Assche N, van Steenberghe D, Guerrero ME, et al. Accuracy of implant placement based on pre-surgical planning of three-dimensional cone-beam images: a pilot study. J Clin Periodontol. 2007;34(9):816-821.
19. Cantoni T, Giovanni P. Implant treatment planning in fresh extraction sockets: use of a novel radiographic guide and CAD/CAM technology. Quintessence Int. 2009;40(9):773-781.
20. Pettersson A, Kero T, Gillot L, et al. Accuracy of CAD/CAM-guided surgical template implant surgery on human cadavers: Part I. J Prosthet Dent. 2010;103(6):334-342.
21. Widmann G, Keiler M, Zangerl A, et al. Computer-assisted surgery in the edentulous jaw based on 3 fixed intraoral reference points. J Oral Maxillofac Surg. 2010;68(5):1140-1147.
22. Tahmaseb A, De Clerck R, Eckert S, Wismeijer D. Reference-based digital concept to restore partially edentulous patients following an immediate loading protocol: a pilot study. Int J Oral Maxillofac Implants. 2011;26(4):707-717.
23. van Steenberghe D, Naert I, Andersson M, et al. A custom template and definitive prosthesis allowing immediate loading in the maxilla: a clinical report. Int J Oral Maxillofac Implants. 2002;17(5):663-670.
24. Parel SM, Triplett RG. Interactive imaging for implant planning, placement and prosthesis construction. J Oral Maxillofac Surg. 2004;62(9 suppl 2):41-47.
25. van Steenberghe D, Glauser R, Blombäck U, et al. A computed tomographic scan-derived customized surgical template and fixed prosthesis for flapless surgery and immediate loading of implants in fully edentulous maxillae: a prospective multicenter study. Clin Implant Dent Relat Res. 2005;7(suppl 1):S111-120.
26. Balshi SF, Wolfinger GJ, Balshi TJ. Surgical planning and prosthesis construction using computer technology and medical imaging for immediate loading of implants in the pterygomaxillary region. Int J Periodontics Restorative Dent. 2006;26(3):239-247.
27. Balshi SF, Wolfinger GJ, Balshi TJ. Surgical planning and prosthesis construction using computed tomography, CAD/CAM technology, and the Internet for immediate loading of dental implants. J Esthet Rest Dent. 2006;18(6):312-325.
28. Scotti R, Pellegrino G, Marchetti C, et al. Diagnostic value of NobelGuide to minimize the need for reconstructive surgery of jaws before implant placement: a review. Quintessence Int. 2010;41(10):809-814.
29. Vasak C, Watzak G, Gahleitner A, et al. Computer tomography-based evaluation of template (NobelGuide™)-guided implant positions: a prospective radiological study. Clin Oral Impl Res. 2011;22(10):1157-1163.
30. Bentz RM, Balshi SF. Complete oral rehabilitation with implants using CAD/CAM technology, stereolithography, and conoscopic holography. Implant Dent. 2012;21(1):8-12.
31. Tulasne J. Implant treatment of missing posterior dentition. In: Albrektsson T, Zarb G, eds. The Brånemark Osseointegrated Implant. Chicago, IL: Quintessence Publishing. 1989:103-116.
32. Balshi S, Wolfinger G, Balshi T. Analysis of 164 titanium oxide-surface implants in completely edentulous arches for fixed prosthesis anchorage using the pterygomaxillary region. Int J Oral Maxillofac Implants. 2005;20(6):946-952.
33. Gallucci GO, Doughtie CB, Hwang JW, et al. Five-year results of fixed implant-supported rehabilitations with distal cantilevers for the edentulous mandible. Clin Oral Impl Res. 2009;20(6):601-607.
34. Aglietta M, Siciliano VI, Zwahlen M, et al. A systematic review of the survival and complication rates of implant supported fixed dental prostheses with cantilever extensions after an observation period of at least 5 years. Clin Oral Impl Res. 2009;20(5):441-451.
35. Cassel B, Dan L, Dan K. Deflections of an implant-supported cantilever beam subjected to vertically directed loads. In vitro measurements in three dimensions using an optoelectronic method. II Analysis of methodological errors. Clin Oral Impl Res. 2011;22(6):645-650.
36. Aglietta M, Siciliano V, Blasi A, et al. Clinical and radiographic changes at implants supporting single-unit crows (SCs) and fixed dental prostheses (FDPs) with one cantilever extension. A retrospective study. Clin Oral Impl Res. 2012;23(5):550-555.
37. Balshi SF, Wolfinger GJ, Balshi TJ. A prospective study of immediate functional loading, following the Teeth in a Day protocol: a case series of 55 consecutive edentulous maxillas. Clin Implant Dent Relat Res. 2005;7(1):24-31.
38. Balshi SF, Wolfinger GJ, Balshi TJ. A retrospective analysis of 110 zygomatic implants in a single-stage immediate loading protocol. Int J Oral Maxillofac Implants. 2009;24(2):335-341.
About the Authors
Thomas J. Balshi, DDS, PhD, FACP
Founder and Prosthodontist
Pi Dental Center
Institute for Facial Esthetics
Fort Washington, Pennsylvania
Glenn J. Wolfinger, DMD, FACP
Prosthodontist
Pi Dental Center
Institute for Facial Esthetics
Fort Washington, Pennsylvania
Stephen F. Balshi, MBE
Director of Research
Pi Dental Center
Institute for Facial Esthetics
Fort Washington, Pennsylvania
President, CM Prosthetics, Inc.
Fort Washington, Pennsylvania