Evolving Implant Design. The NobelActive Implant: Discussion and Case Presentations
Gary Orentlicher, DMD and Matthew Teich, DDS
The design and development of today’s dental implants has been an evolving process based on scientific research, clinician input, and manufacturers’ ingenuity. One new addition to the dental implant armamentarium, the NobelActive™ implant, was introduced worldwide by NobelBiocare® approximately 2 years ago. While many of the design features of the NobelActive implant are found individually in other dental implants, the implant’s combination of external and internal design characteristics provides for unique handling and applications in many difficult clinical situations. Although the NobelActive implant can be used in most all clinical situations, its design allows for high levels of initial stability even in situations with low density or compromised bone, making it a good implant choice for immediate extraction, immediate implant placement, and immediate load cases, as well as cases with less-than-ideal qualities and quantities of bone. In addition, the implant has the ability to be redirected if less-than-ideal implant placement occurs at the time of implant insertion, maximizing the potential prosthetic outcomes. Prosthetically, the implant has features designed to minimize crestal bone loss and maximize gingival architecture, while minimizing the prosthetic components and instrumentation. This article discusses the characteristics of the NobelActive implant in detail and employs case presentations to illustrate its clinical use.
Since the first smooth-surface titanium fixtures were introduced to dentistry in the 1980s, dental implant design has continually evolved as a result of evidence-based research and clinicians’ empirical experiences. Many of these design changes are still used today, while others have disappeared from memory. In the past few years, implant manufacturers have introduced a number of designs. Some are modifications of existing designs, and others are completely new additions to product lines. When new implant designs are examined as a whole, several common threads emerge as implant designs continue to evolve.
Implant body design appears to be moving toward a gradually tapered implant body with more widely spaced threads. A roughened titanium surface from the implant apex to the implant platform is common as are microthreads or grooves in the coronal portion of the implant. In addition to conventional lengths, many implants are now available in 8-mm and 9-mm lengths or shorter. Narrow-diameter implants (ie, 3.0 mm to 3.3 mm), some with internal prosthetic connections, are available in various lengths, as well.
Prosthetic platforms have migrated toward an internal prosthetic connection with a Morse taper interface to minimize the implant/abutment “microgap.” This also may facilitate the concept of “platform switching” that aids clinicians in minimizing crestal bone loss.1-4 Most prosthetic connections of this type have an antirotational feature at the base of the connection for orientation and to ensure the accuracy of the impression coping and abutment seating. In addition, manufacturers have attempted to simplify the prosthetic components and surgical instrumentation for their newer implants.
Recently introduced implants are designed to be placed at bone level while minimizing bone trauma and potential crestal bone loss. Implant neck and abutment contour designs, as well as new concepts of crestal implant soft-tissue attachment, are being used to maximize the maintenance of gingival architecture and support.5-7 Newer implants are designed to provide primary stability for use in immediate extraction and/or immediate loading cases.8,9
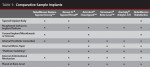
A complete discussion of these advances is beyond the scope of this article. It is clear that implant design continues to evolve in support of dental professionals’ treatment objectives and the daily practice of implant dentistry (Table 1).
NobelBiocare recently introduced NobelActive (https://www.nobelbiocare.com), which is available with an external (one-piece) and internal connection. During the prelaunch phase in the United States, the implant was available in both forms. Since May 2008, only the internal implant is available in North America; the external and internal implants are available in other markets worldwide.
The NobelActive implant has a tapered implant design with sharp, widely spaced (1.2 mm), gradually expanding, double-helical threads that have a steeper thread pitch than most implants. The implant has a roughened titanium surface from apex to platform and is designed to be placed at bone level. The implant design allows for preparing a narrower-than-typical initial implant osteotomy and placing the implant in a method similar to turning a “corkscrew.” This allows for gradual expansion of the bone as the implant advances, similarly to the use of an osteotome. It is designed to be placed at up to 70 Ncm of torque. These characteristics give the implant high levels of primary stability and make it an excellent choice for immediate extraction, immediate placement, and immediate load cases, as well as in cases with poor or questionable quality of bone. In addition, these implant design features allow for the redirection of the implant during placement while maintaining high levels of stability. The implant platform has an internal Morse taper with an inferior antirotational hex at its base. The platform allows for either “platform switching” or abutment fabrication directly on the platform. These design features are incorporated to minimize crestal bone loss and maximize the maintenance of gingival architecture. A much more in-depth discussion of the implant is found later in this article.
The following cases illustrate some of the unique features and applications of this implant.
Case Presentations
Case 1: Immediate Implant Placement, Maxillary Anterior Tooth
A 50-year-old male in good medical and dental health presented for replacement of tooth No. 9 because of a root fracture of the previously endodontically treated tooth (Figure 1 and Figure 2). Clinical examination revealed a normal dentition with no significant periodontal or occlusal issues. Tooth No. 9 presented with a normal zone of attached tissue and adequate gingival symmetry to the adjacent central incisor. The tooth had undergone prior treatment with root canal therapy and placement of an endodontic post/core and a porcelain-fused-to-metal crown. Due to the lack of infection and the excellent bone and gingival architecture, it was decided that this patient was a good candidate for immediate extraction, immediate implant placement, and immediate provisional restoration. A NobelActive implant was chosen because of the ability to redirect the implant if necessary, the implant’s high degree of primary stability at the time of insertion, and the characteristics of the internal implant platform.
Using standard techniques, tooth No. 9 was first extracted atraumatically. Using the established technique for the immediate placement and redirection of a NobelActive implant, an RP 4.3-mm x 13-mm implant was placed (Figure 3, Figure 4 and Figure 5), followed by placement of an immediate temporary abutment with bone graft material (DynaBlast™, Keystone Dental, https://www.keystonedental.com) (Figure 6), and the fabrication and insertion of an immediate provisional restoration (Figure 7). On insertion, the implant was stable to 60 Ncm of torque, measured with a manual torque wrench.
Four months postoperative (Figure 8 and Figure 9), an open-tray implant-level impression was made and tooth No. 8 was prepared for a porcelain veneer. A zirconia abutment (Procera® Zirconia, Nobel Biocare) was fabricated and inserted for implant No. 9 (Figure 10). A definitive zirconia-based crown layered with feldspathic porcelain was then fabricated and cemented provisionally. Tooth No. 8 was restored with a matching porcelain veneer that was bonded in place using the authors’ standard bonding protocol (Figure 11 and Figure 12).
This case illustrates the use of the NobelActive implant’s unique design characteristics, the technique for placement of an immediate implant in an anterior maxillary extraction site, the ability to redirect the implant, and the high initial stability in the successful immediate restoration of a fractured anterior tooth.
Case 2: Immediate Implant Placement, Mandibular Molar Tooth
A 50-year-old female presented with an asymptomatic nonrestorable tooth No. 19 and a space from a previously removed tooth No. 18 (Figure 13).
After a thorough evaluation, due to the lack of infection in the area and the good quality of the bone and soft tissue, it was determined that the patient was a good candidate for an immediate molar extraction, immediate implant placement, and immediate provisional restoration. NobelActive implants were used because of the potential for high initial stability.
A minimally traumatic extraction of tooth No. 19 and exposure of the crestal bone above the area of tooth No. 18 were first performed. Narrow osteotomies (3.6 mm) were then created using a portion of the intraradicular bone of tooth No. 19 and the bone in the region of tooth No. 18. Two NobelActive RP 5-mm x 10-mm implants were then placed in the osteotomies in the sites of teeth Nos. 19 and 18 (Figure 14). After insertion, the implants were stable to 50 Ncm, measured with a manual torque wrench. Porus® mineralized cancellous bone particles (Zimmer Dental Inc, https://www.zimmerdental.com) were then grafted into the socket of tooth No. 19, surrounding any area of exposed implant (Figure 15). Quick Temp™ immediate abutments (Nobel Biocare) were placed on the implants, and provisional restorations were fabricated and temporarily cemented (Figure 16 and Figure 17). Four months later, final restorations were fabricated and permanently cemented in place (Figure 18 and Figure 19).
This case is an example of the use of the NobelActive implant for immediate molar extraction, immediate implant placement, and immediate provisional restoration. The implant has high initial stability in some molar extraction sites and other difficult bony defects that traditionally would not be considered candidates for immediate implant placement and immediate restoration.
Case 3: Staged Implant Placement Using CT-Guided Surgery
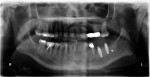
A 17-year-old female presented with multiple congenitally missing teeth and desired permanent tooth replacement. The patient had received orthodontic treatment prior to the dental examination. A comprehensive patient examination, including mounted study casts, radiographs, and intra- and extraoral photographs, was performed first. The patient was in excellent health, and her remaining dental and periodontal examination was unremarkable. Examination revealed congenitally missing maxillary teeth Nos. 4, 6, 7, 10, and 13, and over-retained primary teeth C and D. Clinical examination revealed inadequate bone in width in the areas of Nos. 4, 6, 7, and 10. Panoramic evaluation revealed inadequate height (8 mm to 8.2 mm) in the areas of Nos. 4 and 13 (Figure 20). Due to the age of the patient and the desire for very long term implant success, the authors felt the need to maximize the lengths of the implants. Because the patient presented with multiple congenitally missing teeth and the clinical and radiographic examinations revealed potential atrophy of the bone in all areas where implant placement was planned, further 3-dimensional diagnostic evaluation of the patient was indicated to better evaluate all sites for potential bone grafting prior to implant placement. The CT scan confirmed the deficiencies found on clinical and panoramic examination.
Mounted study models were forwarded to a dental laboratory for fabrication of a diagnostic wax-up. A barium radiographic stent, following the Simplant® protocol (Materialise Dental, https://www.materialise.com), was created from the wax-up to allow the restorative team to visualize the ideal locations of the planned restorations as related to the underlying bony anatomy. The patient wore this appliance during a medical computed tomography (CT) scan evaluation. The CT images were imported into the SimPlant software for evaluation (Figure 21). Based on the CT scan, it was determined that the patient required a staged surgical approach of bone grafting followed by implant placement.
After the removal of teeth C and D, based on the CT scan evaluation of the bone in all implant sites, bone-grafting procedures were performed as follows: in the area of planned tooth No. 4, a sinus lift bone graft for height and a block chin bone graft for width (Figure 22); in the areas of planned teeth Nos. 6 and 7, a “ridge splitting” bone graft for width (Figure 22); in the area of No. 10, a block chin graft for width (Figure 23); and in the area of No. 13, a sinus-lift bone graft for height. Three months after the grafting procedures, a radiographic guide using the NobelGuide™ (NobelBiocare) protocol was fabricated. While wearing this radiographic guide, the patient received a second CT scan (Figure 24).
Implant placement in the areas of teeth Nos. 4, 6, 10, and 13 were then treatment-planned using the NobelGuide software. A pontic was planned for tooth No. 7. Four months after the grafting procedures, a NobelGuide was used to guide the depth, position, and angulations of the implant osteotomies. NobelActive implants were placed in sites of Nos. 4, 6, 10, and 13 (Figure 25 and Figure 26). The procedure required small crestal mini-flaps for final implant-depth determination. Although excellent primary stability was achieved in all sites (45 Ncm measured with a manual torque wrench), it was decided that because the implants were placed largely in grafted bone, healing abutments would be placed. A temporary relief-type removable denture was inserted accordingly.
Four months after implant insertion, excellent soft-tissue adaptation of the gingiva at all the implant sites was observed. Open-tray impressions were made at each site (Figure 27). These records were used in the fabrication of zirconia abutments (Procera Zirconia) that were inserted in each site (Figure 28, Figure 29, and Figure 30).
All final crowns were fabricated with zirconia-based crown layered with feldspathic porcelain. Individual crowns were fabricated to restore teeth Nos. 4, 10, and 13; a cantilevered bridge was fabricated to replace teeth Nos. 6 and No. 7. All units were fitted and cemented with Improv® cement (Nobel Biocare) (Figure 31, Figure 32, Figure 33, Figure 34 and Figure 35).
This case illustrates the evaluation and clinical management of a difficult case of multiple congenitally missing teeth in a young adult patient. An evaluation of the patient’s 3-dimensional bone atrophy as it related to the planned restorations was first performed. This information resulted in appropriate bone grafting procedures performed in each implant site. Using techniques of computer-guided implant surgery, NobelActive implants were then ideally placed in each implant site according to the locations of the planned restoration and the distorted grafted underlying bone. Narrow implant osteotomies were performed followed by the placement of wider NobelActive implants in order to minimize the trauma to the grafted bone, use the implant’s bone expansion osteotome-like features, minimize potential crestal bone loss in a young patient, and maximize the maintenance of the gingival architecture.
Important Features of the Implant Design
External Implant Body Characteristics
The NobelActive implant has a gradually expanding tapered implant body with a gradually expanding thread width, allowing for self-drilling, self-cutting, and self-condensing capabilities. The implant has an expanding central core, with 35° elongated threads (compared to a typical root-form implant’s 60° thread pitch). Inserting it clockwise reportedly allows the implant to compact bone as it is advanced, drawing the surrounding bone into the implant. Two reverse cutting flutes (one on each side of the implant) allow for cutting of the bone when the implant is turned counterclockwise. The sharp apical threads allow for a smaller-diameter osteotomy. The reverse-cutting action of the threads gradually expands the narrower osteotomy and allows the clinician to alter the compressive forces on the bone by using an alternating clockwise and counterclockwise implant insertion technique.
The NobelActive implant is designed to be placed at bone level. The coronal portion of the implant has a back taper, which is intended to maximize the alveolar bone around the collar of the implant and improve soft-tissue support.
The implant’s threads are double helical. There is 1.2 mm between adjacent threads and 2.4 mm between contiguous threads compared with 0.6 mm to 0.7 mm of spacing between threads found in a standard root-form implant. For each rotation, the NobelActive implant advances 2.4 mm—at least three times faster than conventional root-form implants. A clinician who places this implant should consider this. The implant is designed to be placed at up to 70 Ncm of insertion torque. In dense bone, a larger-diameter osteotomy is created, which allows only the implant thread tips to engage the bone, with excellent primary stability. Space between the threads enables new vessel and bone formation.
The NobelActive implant has an osseoconductive-roughened titanium external surface with a unique porous surface structure, which has been documented to enhance osseointegration.10-13 The roughened surface is present from the implant apex to the platform edge. The implant has grooved threads and grooved rings around the inset collar. It has been shown that bone grows more rapidly within the grooves compared with implants without grooves.14
Internal Connection Characteristics
The NobelActive implant has a dual-function connection with a 12°-internal Morse taper with an internal hex at its base for accuracy of abutment seating, orientation, and antirotation. This connection is used in cases in which an internal conical seal with abutment “platform switching” is desired. The platform switch concept, in combination with the back-tapered implant collar, can aid in crestal bone and soft-tissue preservation.1-4 The implant platform has a 0.25-mm shoulder for cases in which a restoration is planned to rest at implant level on the implant platform. The conical seal provides intimate contact between the external abutment surface and the 12°-internal Morse taper surface of the implant.
Prosthetics
To simplify the restoration and the number of prosthetic components necessary to restore a NobelActive implant, the manufacturer produces the implant in three diameters (3.5 mm, 4.3 mm, and 5.0 mm) but on two prosthetic platforms. The 3.5-mm diameter implant has a 3.5-mm platform and its own prosthetic components. The 4.3-mm and 5-mm diameter implants both have the same 3.9-mm implant platform and use the same prosthetic components. Because the NobelActive implant has a dual-function connection, open- and closed-tray impression copings are available for use in cases in which only the internal conical connection—but not the implant shoulder—requires capturing. Copings are also available for situations in which capturing the implant shoulder—but not the conical connection—is required.
Unique Implant Use
A manual or motorized insertion technique can be used for the placement of the NobelActive implant. Manual insertion can be accomplished by using either a hand driver or a manual torque wrench, which is designed to place the implant at up to 70 Ncm of torque. Sometimes a conventional motorized insertion option may be desired. Because the diameter of the osteotomy is frequently narrower than the implant to be placed, the implant often stops before it is fully seated to depth, leaving much of the implant exposed. Completion of the implant insertion using one or both of the manual insertion options will then be necessary. The motorized insertion option is typically used in posterior regions where carrying the implant to the osteotomy site manually can be difficult due to access.
The manual insertion technique—in combination with the cutting characteristics of the implant design, the clinician’s ability to alternate between compression and cutting of the bone, the smaller-diameter initial osteotomy, the 70-Ncm maximal initial implant insertion torque, and the implant’s initial stability—allows the experienced clinician to adjust or redirect the implant orientation during insertion. For placement of an implant in any area of the mouth, the clinician is able to alter the final depth and orientation of the prosthetic connection to optimize the esthetic result. If an alteration of the final depth or platform orientation is desired, the technique of redirecting the implant at the time of implant insertion involves withdrawing the implant, with a counter-clockwise rotation, approximately halfway from within the osteotomy, and then slowly reinserting the implant, in a clockwise rotation, while placing a light pressure on the implant in the direction that the clinician would like to redirect it. This feature is of benefit in any healed bony site or in immediate extraction–immediate placement cases (with or without immediate temporary restorations), particularly in the maxillary anterior region.
The expanding external body taper with a wide-spaced, double-helical thread design, narrower initial osteotomies, and the bone-cutting characteristics of the NobelActive implant provides for high initial stability in most clinical situations. In many cases, the implant can be placed with favorable initial stability in challenging sites with compromised bone, such as the posterior maxilla, narrow ridges, grafted sites, and immediate placement molar extraction sites.
Conclusion
The recently introduced NobelActive implant was designed with external and internal features that make it a good implant choice for many clinical applications. The design allows for high levels of initial stability even in compromised bone, redirection of the implant if necessary at the time of surgery, a prosthetic platform for most restorative situations, and a prosthetic connection designed for maintenance of crestal bone and soft-tissue architecture.
Acknowledgment
The authors thank Robert Rawdin, DDS, for the prosthetics shown in Figure 12 through Figure 18.
Disclosure
Dr. Orentlicher has received lecture honoraria from Nobel Biocare.
References
1. Gardner DM. Platform switching as a means to achieving implant esthetics. NY State Dent J. 2005;71(3):34-37.
2. Vela-Nebot X, Rodríguez-Ciurana X, Rodado-Alonso C, et al. benefits of an implant platform modification technique to reduce crestal bone resorption. Implant Dent. 2006;15(3):313-320.
3. Lazzara RJ, Porter SS. Platform switching: a new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006;26(1):9-17.
4. Baumgarten H, Cocchetto R, Testori T, et al. A new implant design for crestal bone preservation: initial observations and case report. Pract Proced Aesthetic Dent. 2005;17(10):735-740.
5. Rompen E, Raepsaet N, Domken O, et al. Soft tissue stability at facial aspect of gingivally converging abutments in the esthetic zone: a pilot clinical study. J Prosthet Dent. 2007;97(suppl 6):S119-S125.
6. Klinge B, Meyle J; Working Group 2. Soft-tissue integration of implants. Consensus report of Working Group 2. Lin Oral Implants Res. 2006;17(suppl 2):82-92.
7. Touati B, Rompen E, Van Dooren E. A new concept for optimizing soft tissue integration. Pract Proced Aesth Dent. 2005;17(10):711-712, 714-715.
8. Irinakis T, Wiebe C. Initial torque stability of a new bone condensing dental implant. A cohort study of 140 consecutively placed implants. J Oral Implantol. 2009;35(6): 277-282.
9. Tabassum A, Meijer GJ, Wolke JG, et al. Influence of the surgical technique and surface roughness on the primary stability of an implant in artificial bone with a density equivalent to maxillary bone: a laboratory study. Clin Oral Implants Res. 2009;20(4):327-332.
10. Hall J, Lausmaa J. Properties of a new porous oxide surface on titanium implants. Appl Osseointegration Res. 2000;1:5-8.
11. Glauser R, Zembic A, Ruhstaller P, et al. Five-year results of implants with an oxidized surface placed predominantly in soft quality bone and subjected to immediate occlusal loading. J Prosthet Dent. 2007;97(suppl 6):S59-S68.
12. Schüpach P, Glauser R, Rocci A, et al. The human bone-oxidized titanium implant interface: a microscopic, scanning electron microscopic, back-scatter scanning electron microscopic, and energy-dispersive X-ray study of clinically retrieved implants. Clin Implant Dent Relat Res. 2005;7(suppl 1):S36-S43.
13. Huang YH, Xiropaidis AV, Sorensen RG, et al. Bone formation at titanium porous oxide (TiUnite) oral implants in type IV bone. Clin Oral Impl Res. 2005;16(1): 105-111.
14. Hall J, Miranda-Burgos P, Sennerby L. Stimulation of directed bone growth at oxidized titanium implants by macroscopic grooves: an in vivo study. Clin Implant Dent Relat Res. 2005;7(suppl 1):S76-S82.
About the Authors
Gary Orentlicher, DMD
Private Practice
Scarsdale, New York
Matthew Teich, DDS
Private Practice
White Plains, New York