A Narrative Review of the Diagnosis, Etiology, and Treatment of Halitosis Over the Past Three Decades
Stuart J. Froum, DDS; Ye Shi, DDS; Natacha Reis, DDS; and Tanatorn Asvaplungprohm, DDS
ABSTRACT
Although the term "halitosis" was first coined in 1874, people have become increasingly aware of this problem more recently during the COVID-19 pandemic due to extensive wearing of protective masks. In fact, following dental caries and periodontal disease, halitosis is the third most prevalent reason for patients going to the dentist. Due to multifactorial etiology, the diagnosis of halitosis requires a rigorous health/dental/social history, a clinical examination, and measurements. The treatment ranges from the use of dentifrices, mouthwashes, tongue scraping, and masking products, and more recently includes photodynamic therapy, probiotics, and ozone. The purpose of this narrative review was to examine the published literature concerning halitosis over the past 30 years and discuss the diagnosis, etiology, and treatment of the disease.
The term "halitosis" was coined in 1874 by Dr. Joseph William Howe in his book, The Breath and The Diseases Which Give It a Fetid Odor.1 "Halitosis" comes from the Latin word "halitus" ("breath") and the Greek suffix "-osis," which means a diseased state.2 The Oxford English Dictionary defines halitosis as, "A condition in which the breath smells unpleasant."3
While this condition has been identified for about 150 years, recent interest in halitosis has grown because of the need or even requirement in some locations for people to wear a mask due to the COVID-19 virus. Basically, whenever indoors, whether in supermarkets, on buses or subways, and in offices (except in some instances when the surrounding people have been vaccinated), people have been wearing masks. A television news broadcast in May 2020 aired a segment called, "Bad breath behind the coronavirus mask? 10 reasons and remedies for your halitosis."4 A 2021 review article listed halitosis as one of the oral manifestations of COVID-19.5
Most people experience oral malodor even occasionally in their lives. According to the National Institute of Dental Research, approximately 65 million Americans have halitosis at some point during their lives. Moreover, at least 50% of the population has persistent effects of oral malodor, and half of these people suffer from a chronic problem. Oral malodor is considered the third cause of dental office visits, behind dental caries and periodontal diseases.6
The worldwide prevalence of halitosis ranges from 22% to 50%, with the highest percentage being when self-reported. This wide discrepancy is due to perception, self-perceived, and diagnostic tools influenced by race and cultural differences.7-9 There is an increase of halitosis associated with age; however, there is no relationship between the severity of halitosis and gender.10 In addition to a lack of studies on prevalence, the data on prevalence may be inaccurate due to differences in methodologies among studies and to a high number of self-reported cases not considered to be true halitosis.6
The recent interest in halitosis due to mask wearing during the pandemic prompted the authors to examine the problem over the past 30 years, focusing on its diagnosis, etiology, and treatment, and whether any or all of these three aspects changed during this time. The purpose of the following narrative review was to examine the published literature concerning halitosis over the past three decades and discuss the diagnosis, etiology, and treatment of the disease.
Material and Methods
An electronic search was performed in PubMed, MedLine and Google Scholar databases using the following keywords: "halitosis" AND/OR "oral malodor" AND "etiology" AND "diagnosis" AND "treatment." A total of 2,083 articles were found. However, the search results were limited to articles published from 1990 to 2021 in the English language only with full-text access. In addition, the search results were restricted to systematic reviews, reviews, meta-analyses, randomized controlled trials, controlled clinical trials, clinical trials, case series, and case reports, only in humans. The inclusion criteria resulted in 136 articles included in this review of the literature, according to their relevance that was decided by authors' agreement (NR and TA).
The review was divided into four parts: diagnosis, method of measurements, etiology, and treatment.
Diagnosis
The diagnosis of halitosis should begin with the recognition of the problem by the patient or a close confidant of the patient. Determining the cause of halitosis requires a rigorous medical history and physical examination and knowledge of the possible etiology. In 1992, three separate diagnostic groups were considered when diagnosing halitosis: non-pathologic causes, pathologic causes, and, lastly, psychiatric conditions and psychosomatic halitosis.11 However, a systematic classification to distinguish and diagnose halitosis was not established until 2000 by Yaegaki and Coil.12
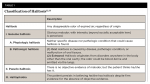
This classification of halitosis includes categories of genuine halitosis, pseudo-halitosis, and halitophobia (Table 1).12,13 Genuine halitosis is defined as obvious malodor beyond socially acceptable levels. It can be perceived by patients and quantified with measuring methods. Genuine halitosis is subclassified into physiologic halitosis and pathologic halitosis. Physiologic halitosis is described as malodor that arises through putrefactive processes within the oral cavity without any related pathologic condition. The origin of physiologic halitosis is mainly the dorsoposterior region of the tongue.14 Temporary halitosis due to dietary factors is excluded from physiologic halitosis even if there is no pathologic condition observed. Pathologic halitosis is subclassified into oral pathologic halitosis and extraoral pathologic halitosis. True pathologic etiology is found in this type of halitosis. Pseudo-halitosis is the condition in which patients stubbornly complain of the existence of oral malodor, but it is not perceived by others.
Halitophobia is the condition in which patients continue to insist that they have halitosis even after they have been treated for genuine or pseudo-halitosis without any physical or social evidence suggesting the presence of halitosis. The condition of halitophobia was confirmed in a study that showed those with a primary complaint of halitosis have a lower percentage of true halitosis than those with secondary complaints.15 This classification not only clearly demonstrates the different etiology and origin for each type of halitosis, but also allows the clinician to diagnose a psychological condition that may be present. It still remains the most cited and acknowledged classification.12
Measurement
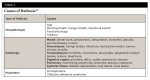
Due to the classification of pseudo-halitosis and halitophobia, the method of measuring halitosis is important for accurate diagnosis and effective management. To date, six major measurements have been used: self-assessment, organoleptic assessment, gas chromatography, sulfide monitor, microbial quantification, and tongue coating status. Each has its own advantages and disadvantages (Table 2).16-32
Since 2000, another measurement by chemical sensor, called "electronic nose," has been used both clinically and in research. The sensor is integrated into a probe and can perform measurement in periodontal pockets and on the dorsum of the tongue. The probe, which is 0.25" x 0.75" in size, is applied with light pressure at the test sites. Electrochemical voltage from the sulfide sensing monitor of the probe is generated in relation to the amount of sulfide ions. It has demonstrated results very comparable to organoleptic readings and gas chromatography measurements.17,33-35 Currently, chemical sensor is the most promising alternative method for both research and clinical purposes. In early 2000, another testing method, the cysteine challenge testing, was utilized to test the efficacy of intervention to reduce malodor in multiple studies. Subjects were instructed to rinse with cysteine to create malodor, and interventions were applied to determine which method could reduce the malodor created from cysteine rinse.36 In 2017, another method of measurement using copper or molybdenum oxide sensors, which have a high affinity and sensitivity to hydrogen sulfide, began gaining increased acceptance and use as a diagnostic tool for halitosis.37
Additional indirect methods for measuring halitosis have been proposed and documented such as the BANA test, which detects the presence of proteolytic obligate gram‐negative anaerobes, primarily those that form the red complex.The test strip shows a blue color in 5 minutes if the results are positive. It is user-friendly and can show a strong positive correlation with periodontal disease activity.34 Other tests include quantifying b‐galactosidase activity,38 lead acetate,22 ammonia monitoring,39 ninhydrin method,39-41 polymerized chain reaction, and more.42 These tests have been found to strongly correlate with standard volatile sulfur compound (VSC) and organoleptic scores, suggesting that they can serve as alternatives to other measurements.
Etiology
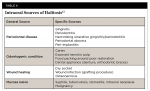
Halitosis has a multifactorial etiology. Understanding the etiology of halitosis is not only important for diagnosis but also for formulating multidisciplinary treatment. Another classification of halitosis reveals the complex etiologies of this disease, which can be divided into non-pathologic/physiologic causes, pathologic causes, and psychiatric causes (Table 3).18,43,44
Genuine halitosis can originate either intraorally or extraorally; however, approximately 80% to 90% of malodor cases originate from the oral cavity.18,43-48 Intraorally caused halitosis can be attributed to three main factors: host (salivary flow, topography of the tongue, external factors such as stress), bacteria, and substrate.19 Substrate can be exogenous (food) or endogenous (saliva).19,28,49-52 Saliva plays an important role in halitosis formation. Depending on the oxygen supply, the substrate provided, the flow rate, and the pH level, saliva can inhibit or favor halitosis production.28,45,49,50,53 The main cause of halitosis, however, is the accumulation of gram-negative anaerobic bacteria from tongue coating and subgingival plaque, which generate VSCs as microbial degradation products.43,45 The association between anaerobic bacteria that produce VSCs and halitosis has been well‐documented since the 1990s.49,54 In the 1990s, the etiology was thought to mainly consist of the three VSCs-hydrogen sulfide, methyl mercaptan, and dimethyl sulfide-with the first two gases contributing to 90% of the VSC in exhaled air.43,49,50 Since 2000, more compounds have been found to be associated with malodor. These include five groups: volatile aromatic compounds, short-chain fatty acids, alcohols, volatile aliphatic compounds, and aldehydes and ketones. However, hydrogen sulfide has a low threshold and high odor power, so the treatment is usually focused on this gas.51,52,55
Physiologic halitosis, as a subclassification of genuine halitosis, is so-called foul morning breath, affecting approximately half of adults.28,56 It is transient, occurs regardless of oral health status, usually is less intense, and can fluctuate at different times of the day.43,50,53,57 Its origin is mainly the dorsoposterior region of the tongue where the microbial putrefaction of food debris, desquamated cells, saliva, and blood are aggravated by the reduction of salivary flow during sleeping at night.19,50 The rough surface of the tongue with a complex papillary structure is a reservoir for anaerobic gram-negative bacteria, which are proficient at producing VSCs from food and epithelial debris. Clinically, higher tongue coating scores are strongly associated with more severe halitosis.18,47,56 Other physiologic causes of halitosis are hormonal changes, especially in women, some types of foods, such as garlic, onions, choline, those containing animal fats, curries, durian, spices, etc., or habits like smoking and drinking alcohol.18,19,45,50
Pathologic halitosis, as the other subclassification of genuine halitosis, can have both intraoral and extraoral etiologies and is more intense than physiologic halitosis.43,50 Intraoral halitosis has odor proliferating from only the mouth, while extraoral halitosis has odor coming from both the mouth and nose.46,47,54
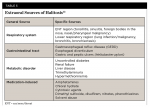
Intraoral sources of halitosis are listed in Table 4.13 Many studies have shown periodontal health to have a direct correlation to halitosis.8,28,49,56,58,59 Patients with periodontitis are three times more prone to halitosis and have eight times more VSCs and four times more tongue coating.8,49 The incidence of halitosis in elderly people can be due to higher prevalence and severity of periodontal disease.49 Patients with chronic periodontitis and deep periodontal pockets suffer from halitosis due to higher amounts of gram-negative anaerobic bacteria, accumulation of debris, and increased putrefaction. The microbiological link between halitosis and periodontal disease is that the main microbial (anaerobic gram-negative) generating VSCs is present in the latter. In addition, coating of the dorsum of the tongue by subgingival bacteria and gingival fluid are also factors promoting VSCs.8,19,28,56,58,60Other odontogenic conditions associated with halitosis can cause retention of food debris, including deep caries, poor restorations, fixed orthodontic appliances, and overwearing of acrylic dentures at night; conditions that cause wound infection, such as a dry socket or foreign graft material exposure, also are culprits. Additionally, several mucosal lesions are oral sources of the disease.18,47,48,61 The absence of saliva or hypofunction causing dry mouth (xerostomia) will result in an increased bacteria accumulation and microbial putrefaction, which will increase VSCs.50,60,62 However, from 2010 on, dry mouth has generally been considered a risk or predisposing factor rather than an etiology of halitosis.47
Extraoral sources of halitosis are listed in Table 5.13 Although approximately only 10% of halitosis cases have an extraoral origin, it is still important to understand the potential sources to complete a proper diagnosis and treatment plan.63 As most authors in the 1990s suggested, main origins are the ear/nose/throat region, with the most common origin being the tonsils64 followed by the pharynx and sinus due to the presence of streptococcal species.65 The lower respiratory tract is a source of the problem due to inflammation or infection,66 trapped foreign bodies are a less frequent cause, and metabolic or gastric dysfunction is a rare cause.28,43,45,50 Since 2000, however, more studies have shown the relationship between gastrointestinal disease and halitosis, especially gastroesophageal reflux disease (GERD) and Helicobacter pylori, both of which are common diseases.19,48 Although much less common, some metabolic disorders also can cause halitosis. In these systemic diseases, odiferous agents circulating in the bloodstream can be exhaled through alveolar gas exchange and cause halitosis. This is also known as blood- borne halitosis. The dimethyl sulfide of the three VSCs is the main contributor to extraoral or blood-borne halitosis.46,48,62 The systemic diseases inducing halitosis include uncontrolled diabetes, pancreas, liver, and renal dysfunction, and the genetic metabolic disorder trimethylaminuria (fish odor syndrome).28,66 More rarely, halitosis can arise as a side effect of medications containing a dimethyl sulfide structure that can appear in breath.18 In 2020, medications causing halitosis were categorized into 10 groups: acid reducers, aminothiols, anticholinergics, antidepressants, antifungals, antihistamines and steroids, antispasmodics, chemotherapeutic agents, dietary supplements, and organosulfur substances.67 The malodor varies according to the systemic condition: diabetic ketoacidosis is presented with fruity odor, bowel obstruction produces a fecal odor, chronic renal failure produces an ammonia- or urine-like odor, and hepatic cirrhosis produces a musty odor.43,45,48,50
Delusional/hallucinatory/imaginary halitosis is caused by psychiatric disorders; it is also known as pseudo-halitosis or halitophobia.28,62 These patients complain of bad breath, however, after rigorous clinical examination, history taking, and halitosis treatment, the symptoms persist and are not detected by other people.43,45,47 These types of halitosis can be caused by mineral and vitamin deficiencies changing the person's taste buds and sense of taste, structural anatomical injuries and abnormalities causing taste disorders, neurodegenerative diseases, or exposure to some types of chemicals.62 Patients experiencing imaginary halitosis can demonstrate specific behaviors such as covering their mouth and keeping distance from others. However, it is difficult for these patients to accept the relation between their halitosis and their psychological condition. The clinician, therefore, should try to convince the patient, without being argumentative, to see a specialist in psychology.28,47,48
Treatment
The first step in the treatment of halitosis is to determine the etiology, then treat accordingly.18,68-70 A thorough medical, dental, and dietary history will help in establishing an accurate diagnosis and effective treatment plan.69 Treatment can be specified according to the extraoral or intraoral cause. Halitosis, however, can also have a detrimental effect on a patient's psychological status. Therefore, it is important to include psychological intervention if needed.71
Since the 1990s, treatments have included dental treatment, mouthrinses, dentifrices, tongue scrapers, masking agents, behavioral modification, and herbal treatments as described in Table 6.15,18,35,70-104 The combination of mechanical and chemical modalities, however, is the most effective and potent treatment for halitosis.105-108
In the late 2000s, the concepts of vaccine therapy and photodynamic therapy (laser) were introduced.109 However, laser treatment was found to be inferior to regular scaling/root planing treatment for malodor reduction in patients with periodontitis.110 In 2009, an oral function program that included facial and tongue muscle exercises, salivary gland massage, and education about oral anatomy was utilized and proved to effectively reduce halitosis and improve salivary flow and overall speech pronunciation.111,112 After 2010, newer halitosis treatments included lactoferrin and lactoperoxidase tablets.113 A review by Scully and Greenman also included metronidazole in the management of persistent halitosis cases.13
In a more recent review in 2016, the authors developed a management strategy based on the type of halitosis, as shown in Figure 1.114
Alternatively, oil pulling has been comparatively effective in reducing malodor in many randomized controlled studies. The mechanism behind oil pulling is that microbes with hydrophobic coats adhere to oil droplets and are expectorated along with the oil. Rice bran oil and sesame oil showed effects comparative to chlorhexidine in reducing halitosis.115-117
The treatment of halitosis has been consistent over the past three decades; only in the last decade has probiotics been advocated as an effective treatment. A recent study indicated that daily consumption of probiotic tablets could help to control halitosis.118-126 Although probiotics did not create permanent colonization, the lasting effect of probiotics could range from 3 days to 2 weeks.119 In 2019, the concept of prebiotics, carbohydrates in the form of fibers, was used along with probiotics in the treatment of halitosis and was shown to successfully reduce halitosis parameters tested in a study.125 Another study used Escherichiacoli to successfully treat gut-caused extraoral halitosis.127 Despite probiotics leading to improved halitosis parameters in many studies, different strains and vehicles have been used, contributing to the need for more standardized research regarding the topic.122,123 In 2018, significant reduction in halitosis parameters was shown after rapid maxillary expansion treatment.128 In 2019, ozone was proposed to be delivered in either gas form, water form, or oil form to kill bacterial pathogens contributing to halitosis.129
Another emerging trend since 2010 is photodynamic or laser treatment. Laser therapy for halitosis treatment involves light-sensitive dye (photosensitizer), a light source with high power energy, and oxygen. The combination will create reactive oxygen species and result in bacterial cell death. Laser treatment was found to produce short-term resolution of halitosis after a single treatment.130-136 A systematic review reported that laser therapy can be an effective adjunct to mechanical debridement, but its effectiveness requires further study.136
A Cochrane review that included multiple studies mentioned in the present review reported that most studies have a low level of evidence, and, consequently, a conclusion cannot be made as to which intervention is the most effective.137
Conclusion
Because of the multifactorial complexity of halitosis, proper diagnosis, identification of the etiology, and timely referrals are important for effective treatment. An interdisciplinary approach in treating halitosis is crucial to prevent misdiagnosis and/or unnecessary treatment. If the etiology is dentally related (eg, caries, periodontal disease, poor oral hygiene), elimination of halitosis can be achieved by correcting these factors, which the patient and dentist may be able to accomplish. However, if systemic factors are contributing to the problem, an interdisciplinary approach is required. Regardless, more controlled studies are needed to determine the most effective treatment of the various types of halitosis.
ABOUT THE AUTHORS
Stuart J. Froum, DDS
Adjunct Clinical Professor and Director of Clinical Research, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York; Private Practice, New York, New York
Ye Shi, DDS
Clinical Assistant Professor, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York
Natacha Reis, DDS
Fellow at Advanced Program for International Dentists in Implant Dentistry, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York; Diplomate, International Congress of Oral Implantologists
Tanatorn Asvaplungprohm, DDS
Fellow at Advanced Program for International Dentists in Implant Dentistry, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York; Diplomate, International Congress of Oral Implantologists
REFERENCES
1. Howe JW. The Breath and the Diseases Which Give It a Fetid Odor. New York, NY: Appleton & Co; 1874.
2. Messadi DV, Younai FS. Halitosis. Dermatol Clin. 2003;21(1):147-155.
3. Oxford English Dictionary. 7th ed. Oxford University Press; 2013.
4. LaMotte S. Bad breath behind the coronavirus mask? 10 reasons and remedies for your halitosis. CNN. May 5, 2020.
5. Iranmanesh B, Khalili M, Amiri R, et al. Oral manifestations of COVID-19 disease: a review article. Dermatol Ther. 2021;34(1):e14578.
6. Loesche WJ, Kazor C. Microbiology and treatment of halitosis. Periodontol 2000. 2002;28:256-279.
7. Akaji EA, Folaranmi N, Ashiwaju O. Halitosis: a review of the literature on its prevalence, impact and control. Oral Health Prev Dent. 2014;12(4):297-304.
8. Silva MF, Leite FRM, Ferreira LB, et al. Estimated prevalence of halitosis: a systematic review and meta-regression analysis. Clin Oral Investig. 2018;22(1):47-55.
9. Paradowska A, Marczewski B, Pawlowska-Cierniak E. Self-perception of halitosis among students of Wroclaw Medical University. Adv Clinical Exp Med. 2007;16(4):543-548.
10. Feller L, Blignaut E. Halitosis: a review. SADJ. 2005;60(1):17-19.
11. Masui I. Perception and behaviors toward oral malodor and psychosomatic factors. Jpn J Dent Practice Admin. 1997;32:107-125.
12. Yaegaki K, Coil JM. Examination, classification, and treatment of halitosis; clinical perspectives. J Can Dent Assoc. 2000;66(5):257-261.
13. Scully C, Greenman J. Halitosis (breath odor). Periodontol 2000. 2008;48:66-75.
14. Roldán S, Herrera D, Sanz M. Biofilms and the tongue: therapeutical approaches for the control of halitosis. Clin Oral Investig. 2003;7(4):189-197.
15. Outhouse TL, Fedorowicz Z, Keenan JV, Al-Alawi R. A Cochrane systematic review finds tongue scrapers have short-term efficacy in controlling halitosis. Gen Dent. 2006;54(5):352-368.
16. Rosenberg M. Bad breath, diagnosis and treatment. Univ Tor Dent J. 1990;3(2):7-11.
17. Clark GT, Nachnani S, Messadi DV. Detecting and treating oral and nonoral malodors. J Calif Dent Assoc. 1997;25(2):133-144.
18. Ayers KM, Colquhoun AN. Halitosis: causes, diagnosis, and treatment. N Z Dent J. 1998;94(418):156-160.
19. Porter SR, Scully C. Oral malodour (halitosis). BMJ. 2006;333(7569):632-635.
20. Greenman J, Lenton P, Seemann R, Nachnani S. Organoleptic assessment of halitosis for dental professionals-general recommendations. J Breath Res. 2014;8(1):017102.
21. Saad S, Greenman J, Duffield J, Sudlow K. Use of n-butanol as an odorant to standardize the organoleptic scale of breath odour judges. Oral Dis. 2005;11 suppl 1:45-47.
22. Aydin M, Bollen CM, Özen ME. Diagnostic value of halitosis examination methods. Compend Contin Educ Dent. 2016;37(3):174-178.
23. Greenman J, Duffield J, Spencer P, et al.Study on the organoleptic intensity scale for measuring oral malodor. J Dent Res. 2004;83(1):81-85.
24. Rosenberg M, McCulloch CA. Measurement of oral malodor: current methods and future prospects. J Periodontol. 1992;63(9):776-782.
25. Murata T, Yamaga T, Iida T, et al. Classification and examination of halitosis. Int Dent J. 2002;52 suppl 3:181-186.
26. Bosy A. Oral malodor: philosophical and practical aspects. J Can Dent Assoc. 1997;63(3):196-201.
27. Rosenberg M, Kulkari GV, Bosy A, McCulloch CA. Reproducibility and sensitivity of oral malodor measurements with a portable sulphide monitor. J Dent Res. 1991;70(11):1436-1440.
28. van Steenberghe D. Breath malodor. Curr Opin Periodontol. 1997;4:137-143.
29. Salako NO, Philip L. Comparison of the use of the Halimeter and the Oral Chroma™ in the assessment of the ability of common cultivable oral anaerobic bacteria to produce malodorous volatile sulfur compounds from cysteine and methionine. Med Princ Pract. 2011;20(1):75-79.
30. Miyazaki H, Sakao S, Katoh Y, Takehara T. Correlation between volatile sulphur compounds and certain oral health measurements in the general population. J Periodontol. 1995;66(8):679-684.
31. Danser MM, Gómez SM, Van der Weijden GA. Tongue coating and tongue brushing: a literature review. Int J Dent Hyg. 2003;1(3):151-158.
32. Shimizu T, Ueda T, Sakurai K. New method for evaluation of tongue-coating status. J Oral Rehabil. 2007;34(6):442-447.
33. Tanaka M, Anguri H, Nonaka A, et al. Clinical assessment of oral malodor by the electronic nose system. J Dent Res. 2004;83(4):317-321.
34. Figueiredo LC, Rosetti EP, Marcantonio Jr E, et al. The relationship of oral malodor in patients with or without periodontal disease. J Periodontol. 2002;73(11):1338-1342.
35. Aylikci BU, Colak H. Halitosis: from diagnosis to management. J Nat Sci Biol Med. 2013;4(1):14-23.
36. Kleinberg I, Codipilly DM. Cysteine challenge testing: a powerful tool for examining oral malodour processes and treatments in vivo. Int Dent J. 2002;52 suppl 3:221-228.
37. Yoon JW, Lee JH. Toward breath analysis on a chip for disease diagnosis using semiconductor-based chemiresistors: recent progress and future perspectives. Lab Chip. 2017;17(21):3537-3557.
38. Yoneda M, Masuo Y, Suzuki N, et al. Relationship between the β-galactosidase activity in saliva and parameters associated with oral malodor. J Breath Res. 2010;4(1):017108.
39. Amano A, Yoshida Y, Oho T, Koga T. Monitoring ammonia to assess halitosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94(6):692-696.
40. Quirynen M, Zhao H, Avontroodt P, et al. A salivary incubation test for evaluation of oral malodor: a pilot study. J Periodontol. 2003;74(7):937-944.
41. Iwanicka-Grzegorek K, Lipkowska E, Kepa J, et al. Comparison of ninhydrin method of detecting amine compounds with other methods of halitosis detection. Oral Dis. 2005;11 suppl 1:37-39.
42. Suzuki N, Yoshida A, Nakano Y. Quantitative analysis of multi-species oral biofilms by TaqMan real-time PCR. Clin Med Res. 2005;3(3):176-185.
43. Touyz LZ. Oral malodor - a review. J Can Dent Assoc. 1993;59(7):607-610.
44. Johnson BE. Halitosis, or the meaning of bad breath. J Gen Intern Med. 1992;7(6):649-656.
45. Scully C, el-Maaytah M, Porter SR, Greenman J. Breath odor: etiopathogenesis, assessment and management. Eur J Oral Sci. 1997;105(4):287-293.
46. Tangerman A, Winkel EG. Intra- and extra-oral halitosis: finding of a new form of extra-oral blood-borne halitosis caused by dimethyl sulphide. J Clin Periodontol. 2007;34(9):748-755.
47. Wu J, Cannon RD, Ji P, et al. Halitosis: prevalence, risk factors, sources, measurement and treatment - a review of the literature. Aust Dent J. 2020;65(1):4-11.
48. Mokeem SA. Halitosis: a review of the etiologic factors and association with systemic conditions and its management. J Contemp Dent Pract. 2014;15(6):806-811.
49. Ratcliff PA, Johnson PW. The relationship between oral malodor, gingivitis and periodontitis. A review. J Periodontol. 1999;70(5):485-489.
50. Messadi DV. Oral and nonoral sources of halitosis. J Calif Dent Assoc. 1997;25(2):127-131.
51. Ye W, Zhang Y, He M, et al. Relationship of tongue coating microbiome on volatile sulfur compounds in healthy and halitosis adults. J Breath Res. 2019;14(1):016005.
52. Nachnani S. Oral malodor: causes, assessment, and treatment. Compend Contin Educ Dent. 2011;32(1):22-31.
53. Kleinberg I, Westbay G. Salivary and metabolic factors involved in oral malodor formation. J Periodontol. 1992;63(9):768-775.
54. Krespi YP, Shrime MG, Kacker A. The relationship between oral malodor and volatile sulfur compound-producing bacteria. Otolaryngol Head Neck Surg. 2006;135(5):671-676.
55. van den Velde S, Quirynen M, van Hee P, van Steenberghe D. Halitosis associated volatiles in breath of healthy subjects. J Chromatogr B Analyt Technol Biomed Life Sci. 2007;853(1-2):54-61.
56. Calil C, Liberato FL, Pereira AC, et al. The relationship between volatile sulphur compounds, tongue coating and periodontal disease. Int J Dent Hyg. 2009;7(4):251-255.
57. Rosenberg M. Clinical assessment of bad breath: current concepts [erratum in J Am Dent Assoc. 1996;127(5):570]. J Am Dent Assoc. 1996;127(4):475-482.
58. Morita M, Wang HL. Association between oral malodor and adult periodontitis: a review. J Clin Periodontol. 2001;28(9):813-819.
59. Amou T, Hinode D, Yoshioka M, Grenier D. Relationship between halitosis and periodontal disease - associated oral bacteria in tongue coatings. Int J Dent Hyg. 2014;12(2):145-151.
60. Frydman A. Oral malodor: a review. J West Soc Periodontol Periodontal Abstr. 2004;52(1):5-10.
61. Huang J, Li CY, Jiang JH. Effects of fixed orthodontic brackets on oral malodor: a systematic review and meta-analysis according to the preferred reporting items for systematic reviews and meta-analyses guidelines. Medicine (Baltimore). 2018;97(14):e0233.
62. Falcão DP, Vieira CN, de Amorim RFB. Breaking paradigms: a new definition for halitosis in the context of pseudo-halitosis and halitophobia. J Breath Res. 2012;6(1):017105.
63. Delanghe G, Ghyselen J, Feenstra L, van Steenberghe D. Experiences of a Belgian multidisciplinary breath odour clinic. Acta Otorhinolaryngol Belg. 1997;51(1):43-48.
64. Bollen CM, Beikler T. Halitosis: the multidisciplinary approach. Int J Oral Sci. 2012;4(2):55-63.
65. Rösing CK, Loesche W. Halitosis: an overview of epidemiology, etiology and clinical management. Braz Oral Res. 2011;25(5):466-471.
66. Preti G, Clark L, Cowart BJ, Feldman RS, Lowry LD, Weber E, Young IM. Non-oral etiologies of oral malodor and altered chemosensation. J Periodontol. 1992;63(9):790-796.
67. Mortazavi H, Rahbani Nobar B, Shafiei S. Drug-related halitosis: a systematic review. Oral Health Prev Dent. 2020;18(1):399-407.
68. Froum SJ, Salaverry KR. The dentist's role in diagnosis and treatment of halitosis. Compend Contin Educ Dent. 2013;34(9):670-677.
69. Neiders M, Ramos B. Operation of bad breath clinics. Quintessence Int. 1999;30(5):295-301.
70. Akaji EA, Folaranmi N, Ashiwaju O. Halitosis: a review of the literature on its prevalence, impact and control. Oral Health Prev Dent. 2014;12(4):297-304.
71. He M, Lu H, Cao J, et al. Psychological characteristics of Chinese patients with genuine halitosis. Oral Dis. 2020;26(7):1576-1585.
72. da Conceição MD, Marocchio LS, Tárzia O. Evaluation of a new mouthwash on caseous formation. Braz J Otorhinolaryngol. 2008;74(1):61-67.
73. Scully Cbe C, Porter S. Halitosis. BMJ Clin Evid. 2008;2008:1305.
74. Deutscher H, Derman S, Barbe AG, et al. The effect of professional tooth cleaning or non-surgical periodontal therapy on oral halitosis in patients with periodontal diseases. A systematic review. Int J Dent Hyg. 2018;16(1):36-47.
75. Guentsch A, Pfister W, Cachovan G, et al. Oral prophylaxis and its effects on halitosis-associated and inflammatory parameters in patients with chronic periodontitis. Int J Dent Hyg. 2014;12(3):199-207.
76. Quirynen M, Avontroodt P, Soers C, et al. The efficacy of amine fluoride/stannous fluoride in the suppression of morning breath odour. J Clin Periodontol. 2002;29(10):944-954.
77. Grigor J, Roberts AJ. Reduction in the levels of oral malodor precursors by hydrogen peroxide: in-vitro and in-vivo assessments. J Clin Dent. 1992;3(4):111-115.
78. Shinada K, Ueno M, Konishi C, et al. Effects of a mouthwash with chlorine dioxide on oral malodor and salivary bacteria: a randomized placebo-controlled 7-day trial. Trials. 2010;11:14.
79. Lee SS, Suprono MS, Stephens J, et al. Efficacy of stabilized chlorine dioxide-based unflavored mouthwash in reducing oral malodor: an 8-week randomized controlled study. Am J Dent. 2018;31(6):309-312.
80. Hur MH, Park J, Maddock-Jennings W, et al. Reduction of mouth malodour and volatile sulphur compounds in intensive care patients using an essential oil mouthwash. Phytother Res. 2007;21(7):641-643.
81. Dobler D, Runkel F, Schmidts T. Effect of essential oils on oral halitosis treatment: a review. Eur J Oral Sci. 2020;128(6):476-486.
82. Fine DH, Furgang D, Sinatra K, et al. In vivo antimicrobial effectiveness of an essential oil-containing mouth rinse 12 h after a single use and 14 days' use. J Clin Periodontol. 2005;32(4):335-340.
83. Fedorowicz Z, Aljufairi H, Nasser M, et al. Mouthrinses for the treatment of halitosis. Cochrane Database Syst Rev. 2008;(4):CD006701.
84. Roldán S, Herrera D, O'Connor A, et al. A combined therapeutic approach to manage oral halitosis: a 3-month prospective case series. J Periodontol. 2005;76(6):1025-1033.
85. van den Broek AM, Feenstra L, de Baat C. A review of the current literature on management of halitosis. Oral Dis. 2008;14(1):30-39.
86. Quirynen M, Zhao H, van Steenberghe D. Review of the treatment strategies for oral malodour. Clin Oral Investig. 2002;6(1):1-10.
87. Rösing CK, Jonski G, Rølla G. Comparative analysis of some mouthrinses on the production of volatile sulfur-containing compounds. Acta Odontol Scand. 2002;60(1):10-12.
88. Roldán S, Herrera D, Santa-Cruz I, et al. Comparative effects of different chlorhexidine mouth-rinse formulations on volatile sulphur compounds and salivary bacterial counts. J Clin Periodontol. 2004;31(12):1128-1134.
89. Rölla G, Jonski G, Young A. The significance of the source of zinc and its anti-VSC effect. Int Dent J. 2002;52 suppl 3:233-235.
90. Ademovski SE, Lingström P, Winkel E, et al. Comparison of different treatment modalities for oral halitosis. Acta Odontol Scand. 2012;70(3):224-233.
91. Dadamio J, Van Tournout M, Teughels W, et al. Efficacy of different mouthrinse formulations in reducing oral malodour: a randomized clinical trial. J Clin Periodontol.2013;40(5):505-513.
92. Pedrazzi V, do Nascimento C, Mardegan Issa JP, Fedorowicz Z. Interventions for managing halitosis. Cochrane Database Syst Rev. 2016;5:CD012213.
93. Brunette DM, Proskin HM, Nelson BJ. The effects of dentifrice systems on oral malodor. J Clin Dent. 1998;9(3):76-82.
94. Niles HP, Vazquez J, Rustogi KN, et al. The clinical effectiveness of a dentifrice containing triclosan and a copolymer for providing long-term control of breath odor measured chromatographically. J Clin Dent. 1999;10(4):135-138.
95. Sharma NC, Galustians HJ, Qaquish J, et al. The clinical effectiveness of a dentifrice containing triclosan and a copolymer for controlling breath odor measured organoleptically twelve hours after toothbrushing. J Clin Dent. 1999;10(4):131-134.
96. Farrell S, Baker RA, Somogyi-Mann M, et al. Oral malodor reduction by a combination of chemotherapeutical and mechanical treatments. Clin Oral Investig. 2006;10(2):157-163.
97. Sreenivasan P. The effects of a triclosan/copolymer dentifrice on oral bacteria including those producing hydrogen sulfide. Eur J Oral Sci. 2003;111(3):223-227.
98. Vazquez J, Pilch S, Williams MI, Cummins D. Clinical efficacy of a triclosan/copolymer/NaF dentifrice and a commercially available breath-freshening dentifrice on hydrogen sulfide-forming bacteria. Oral Dis. 2005;11 suppl 1:64-66.
99. Nogueira-Filho GR, Duarte PM, Toledo S, et al. Effect of triclosan dentifrices on mouth volatile sulphur compounds and dental plaque trypsin-like activity during experimental gingivitis development. J Clin Periodontol. 2002;29(12):1059-1064.
100. Newby EE, Hickling JM, Hughes FJ, et al. Control of oral malodour by dentifrices measured by gas chromatography. Arch Oral Biol. 2008;53 suppl 1:19-25.
101. Faveri M, Hayacibara MF, Pupio GC, et al. A cross-over study on the effect of various therapeutic approaches to morning breath odour. J Clin Periodontol. 2006;33(8):555-560.
102. Pedrazzi V, Sato S, de Mattos Mda G, et al. Tongue-cleaning methods: a comparative clinical trial employing a toothbrush and a tongue scraper. J Periodontol. 2004;75(7):1009-1012.
103. Van der Sleen MI, Slot DE, Van Trijffel E, et al. Effectiveness of mechanical tongue cleaning on breath odour and tongue coating: a systematic review. Int J Dent Hyg. 2010;8(4):258-268.
104. Muniz FW, Friedrich SA, Silveira CF, Rösing CK. The impact of chewing gum on halitosis parameters: a systematic review. J Breath Res. 2017;11(1):014001.
105. Aung EE, Ueno M, Zaitsu T, et al. Effectiveness of three oral hygiene regimens on oral malodor reduction: a randomized clinical trial. Trials.2015;16:31.
106. Ademovski SE, Persson GR, Winkel E, et al. The short-term treatment effects on the microbiota at the dorsum of the tongue in intra-oral halitosis patients-a randomized clinical trial. Clin Oral Investig. 2013;17(2):463-473.
107. Feres M, Figueiredo LC, Faveri M, et al. The efficacy of two oral hygiene regimens in reducing oral malodour: a randomised clinical trial. Int Dent J. 2015;65(6):292-302.
108. Quirynen M, Zhao H, Soers C, et al. The impact of periodontal therapy and the adjunctive effect of antiseptics on breath odor-related outcome variables: a double-blind randomized study. J Periodontol. 2005;76(5):705-712.
109. Liu PF, Zhu WH, Huang CM. Vaccines and photodynamic therapies for oral microbial-related diseases. Curr Drug Metab. 2009;10(1):90-94.
110. Betsy J, Prasanth CS, Baiju KV, et al. Efficacy of antimicrobial photodynamic therapy in the management of chronic periodontitis: a randomized controlled clinical trial. J Clin Periodontol. 2014;41(6):573-581.
111. Hakuta C, Mori C, Ueno M, et al. Evaluation of an oral function promotion programme for the independent elderly in Japan. Gerodontology. 2009;26(4):250-258.
112. Nishimura T, Takahashi C, Takahashi E. Dental hygiene residential care in a 3-year dental hygiene education programme in Japan: towards dysphagia management based on the dental hygiene process of care. Int J Dent Hyg. 2007;5(3):145-150.
113. Shin K, Yaegaki K, Murata T, et al. Effects of a composition containing lactoferrin and lactoperoxidase on oral malodor and salivary bacteria: a randomized, double-blind, crossover, placebo-controlled clinical trial. Clin Oral Investig. 2011;15(4):485-493.
114. Kapoor U, Sharma G, Juneja M, Nagpal A. Halitosis: current concepts on etiology, diagnosis and management. Eur J Dent. 2016;10(2):292-300.
115. Sheikh FS, Iyer RR. The effect of oil pulling with rice bran oil, sesame oil, and chlorhexidine mouth rinsing on halitosis among pregnant women: a comparative interventional study. Indian J Dent Res. 2016;27(5):508-512.
116. Rosenberg M, Gelernter I, Barki M, Bar-Ness R. Day-long reduction of malodor by two-phase oil:water mouthrinse as compared to chlorhexidine and placebo rinses. J Periodontol. 1992;63(1):39-43.
117. Asokan S, Kumar RS, Emmadi P, et al. Effect of oil pulling on halitosis and microorganisms causing halitosis: a randomized controlled pilot trial. J Indian Soc Pedod Prev Dent. 2011;29(2):90-94.
118. Benic GZ, Farella M, Morgan XC, et al. Oral probiotics reduce halitosis in patients wearing orthodontic braces: a randomized, triple-blind, placebo-controlled trial. J Breath Res. 2019;13(3):036010.
119. Flichy-Fernández AJ, Alegre-Domingo T, Peñarrocha-Oltra D, Peñarrocha-Diago M. Probiotic treatment in the oral cavity: an update. Med Oral Patol Oral Cir Bucal. 2010;15(5):e677-e680.
120. Teughels W, Van Essche M, Sliepen I, Quirynen M. Probiotics and oral healthcare. Periodontol 2000. 2008;48:111-147.
121. Meurman JH, Stamatova IV. Probiotics: evidence of oral health implications. Folia Med (Plovdiv). 2018;60(1):21-29.
122. Georgiou AC, Laine ML, Deng DM, et al. Efficacy of probiotics: clinical and microbial parameters of halitosis. J Breath Res. 2018;12(4):046010.
123. Yoo JI, Shin IS, Jeon JG, et al. The effect of probiotics on halitosis: a systematic review and meta-analysis. Probiotics Antimicrob Proteins. 2019;11(1):150-157.
124. Pietri FK, Rossouw PE, Javed F, Michelogiannakis D. Role of probiotics in oral health maintenance among patients undergoing fixed orthodontic therapy: a systematic review of randomized controlled clinical trials. Probiotics Antimicrob Proteins. 2020;12(4):1349-1359.
125. Mousquer CR, Della Bona A, Milani DC, et al. Are Lactobacillus salivarius G60 and inulin more efficacious to treat patients with oral halitosis and tongue coating than the probiotic alone and placebo? A randomized clinical trial. J Periodontol. 2020;91(6):775-783.
126. Bonifait L, Chandad F, Grenier D. Probiotics for oral health: myth or reality? J Can Dent Assoc. 2009;75(8):585-590.
127. Henker J, Schuster F, Nissler K. Successful treatment of gut-caused halitosis with a suspension of living non-pathogenic Escherichia coli bacteria-a case report. Eur J Pediatr. 2001;160(10):592-594.
128. Erhamza TS, Ozdıler FE. Effect of rapid maxillary expansion on halitosis. Am J Orthod Dentofacial Orthop. 2018;154(5):702-707.
129. Suh Y, Patel S, Kaitlyn R, et al. Clinical utility of ozone therapy in dental and oral medicine. Med Gas Res. 2019;9(3):163-167.
130. da Mota Ciarcia ACC, Gonçalves MLL, Horliana ACRT, et al. Action of antimicrobial photodynamic therapy with red leds in microorganisms related to halitose: controlled and randomized clinical trial. Medicine (Baltimore). 2019;98(1):e13939.
131. Krespi YP, Kizhner V, Wilson KA, et al. Laser tongue debridement for oral malodor - a novel approach to halitosis. Am J Otolaryngol. 2021;42(1):102458.
132. Llanos do Vale K, Ratto Tempestini Horliana AC, Romero Dos Santos S, et al. Treatment of halitosis with photodynamic therapy in older adults with complete dentures: a randomized, controlled, clinical trial. Photodiagnosis Photodyn Ther. 2021;33:102128.
133. Alshahrani AA, Alhaizaey A, Kamran MA, Alshahrani I. Efficacy of antimicrobial photodynamic therapy against halitosis in adolescent patients undergoing orthodontic treatment. Photodiagnosis Photodyn Ther. 2020;32:102019.
134. Lopes RG, Costa da Mota AC, Soares C, et al. Immediate results of photodynamic therapy for the treatment of halitosis in adolescents: a randomized, controlled, clinical trial. Lasers Med Sci. 2016;31(1):41-47.
135. Costa da Mota AC, Franca CM, Prates R, et al. Effect of photodynamic therapy for the treatment of halitosis in adolescents - a controlled, microbiological, clinical trial. J Biophotonics. 2016;9(11-12):1337-1343.
136. Kellesarian SV, Malignaggi VR, Al-Kheraif AA, et al. Effect of antimicrobial photodynamic therapy and laser alone as adjunct to mechanical debridement in the management of halitosis: a systematic review. Quintessence Int. 2017;48(7):575-583.
137. Nagraj SK, Eachempati P, Uma E, et al. Interventions for managing halitosis. Cochrane Database Syst Rev. 2019;12(12):CD012213.