Plan Well and Follow the Plan
To be executed well, implant cases require critical upfront planning.
Each case the dental team starts should be based on a solid plan with the final result in mind. Although we, as dental technologists, talk and write about the diagnostic process, the key elements to make the final restoration successful are sometimes skipped. The diagnostic wax-up is usually the starting point; however, the planning thought processes based on the provided patient information are much more critical at this early stage. Each case has its own set of challenges, and when implants are involved, the technologist must be able to diagnostically work through them as much as possible to achieve a predictable final result.
Usually, the dental technologist is unaware of the medical and dental history of patients whose cases are presented to the laboratory. The patient in this case, however, did present to the laboratory, and indicated at that time that she had several surgeries and had been through a long process. The ability to meet with the patient allows the technologist to understand his or her needs and esthetic concerns. In the future of dental technology, the patient evaluation process will take on an even larger role as the technologist begins to work more closely with the dentist and patient. The face-to-face evaluation process also helps the patient to understand the dental team’s needs and limitations and creates the environment to explore esthetic options, tooth parameters, and the view of what nature has provided. When taking any custom shade, the author spends time with patients—educating them on tooth color, position, and esthetics.
As we start the wax-up process for a case such as this, technologists must remember that the wax-up is nothing more than the esthetic vision of what is thought to best fit the patient, keeping in mind the patient’s variables and expectations. At the same time, the wax-up becomes the blueprint for implant placement (when possible), abutments, substructure frame and/or bar designs, and the actual substructure framework. If technologists have an opportunity to meet their patients, the information provided can be priceless.
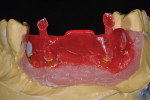
When waxing an implant case such as this, the author finds it useful to leave the implant access holes exposed to help determine where the implants are and how they will affect the final restorative options (Figure 1). The wax-up in this case also needed a gingival component, which always makes the work that much more difficult, as it will cover any information the implant cast may provide (Figure 2 and Figure 3). Using the implant screws as a guide also helps to evaluate the implant paths, which can help determine if secondary implant components are needed to improve the angulation (Figure 4). With challenging implant cases, the beginning stage is very critical to the final result. Tissue depth of the implant placement, angulation, and position were the main focus for this case during the diagnostic evaluation. Implant placement based on visualizing where the prosthesis needs to be helps determine if the angulation of the implants will need to be adjusted and brought to the height of the tissue to help improve tissue response and to maintain access for the health of the tissue. As with all implant cases, the ability to access or retrieve the components is crucial. When possible, the case should be designed with that prospect in mind.
Based on the diagnostic information, it was determined that a bar design would create the proper support for the future ceramic, and set-screws would allow the technologist to keep the final prosthetic retrievable. It is important to remember that the wax-up is merely the vision of what the author believes will be the best solution for the patient, but this hypothesis will need to be tested in the provisional stage for its esthetic outcome. When the wax-up is complete, the information it provides can help fabricate the final restoration only when it has been transferred to a provisional restoration and tested intraorally. Based on the wax-up plan and indexes, the provisional can be processed.
Creation of the Provisional
Several indexes were created from the diagnostic information and used to fabricate the provisional. This step provided a checking mechanism for the remainder of the prosthetics (Figure 5). The wax-up and cast were set into a duplicating flask, and putty was used to index the wax-up position. Once indexed, the putty and flask can be used for several different processes as well as allow the author to have a repeatable process when needed. This allowed the author to duplicate an exact replica of the wax-up with no dimensional changes (Figure 6). The wax-up was then removed from the cast, and temporary abutments were set in place to support the provisional (Figure 7). PMMa material was chosen and injected into the vacant mold of the flask to create a perfect reproduction of the original wax-up (Figure 8).
The Cutback
Working with acrylic and the reference indexes gave the author the ability to quickly modify to create a more esthetic provisional (Figure 9). The incisal edges were reduced to a mamelon-like structure based on the index. This provided space for staining materials and acrylic enamels (Figure 10 and Figure 11). After the staining process, the enamels could be re-injected into the original flask (Figure 12 and Figure 13). Pink composite would be built by hand to replicate the gingival portion of the case and would also be used in the future for gingival shade reference (Figure 14 and Figure 15). The provisional was tried in and evaluated for its functional and esthetic result. The key at this point was to evaluate the vision for esthetics and function and, if needed, to make any changes at this time. The provisional became the blueprint for the final result and needed to provide the proper functional information. The esthetic parameters could and did keep evolving. Another advantage of using the flask-type system is, if the first provisional is correct, the technologist could now re-inject resin material for scanning or for casting (Figure 16).
Creating the Framework
With the provisional finalized, the technologist could now design the retrievable supporting system for the final ceramic. Secondary implant components were used to bring the implant level to the tissue height and to alter the original poor implant angulation (Figure 17). A duplicated wax-up from the previous flask allowed the technologist to design the bar structure following the original or modified blueprint (Figure 18 through Figure 20). Many options exist today for this process, including scanning the resin- or wax-designed bar structure, CAD designing the bar and milling it in a multitude of materials, or having the technician wax and cast the bar using traditional techniques, which is still a very predictable process.
The bar design was critical for the ceramic support. The bar needed to be large enough to allow the secondary frame to be as minimal as possible and yet small enough to not take up space for the future ceramic. The bar would also support two set-screws that would retain the secondary frame and allow the final restoration to be removable. For this bar design, resin was used instead of wax, which allowed the author to reproduce the original pattern again and mill it to the desired bar design. The final bar was conventionally cast due to time constraints and its design complexity. However, the author likes the concept of having these bars CAM-milled
in titanium.
The index was used again to duplicate the wax-up over the newly cast bar with an underlying resin frame for support (Figure 21 and Figure 22). Using the indexes, the technician cut back the wax or resin frame for future ceramic. Set screws were tapped and resin was cured into the final frame for casting (Figure 23). Casting was completed using a broken-arm casting technique, and the metal was prepared for ceramic (Figure 24 and Figure 25).
Layering the Ceramic
When dealing with “white and pink” ceramics, there are several additional challenges for the ceramist. The frame was opaqued and the ceramic layering began (Figure 26). Opacious materials were used to create the base layering for the “white” portion and overlaid with dentin materials of several values. Mamelon materials and translucence were also used in the first bake, and, lastly, the “pink” base shades were applied (Figure 27 and Figure 28). Again, the index served as a guideline/blueprint for the final ceramic. After the first bake, a second bake was completed with more focus on the “pink” gingival portion of the restoration (Figure 29 through Figure 31). The height of the contours were checked and slightly adjusted. The ceramic was prepared for the final glaze bake. Ceramic was added in the glaze bake, but the author mixed in lower-fusing ceramic into the materials to adjust the firing parameters for the final glaze bake (Figure 32). The final restoration was polished with pumice and finished (Figure 33 through Figure 35).
The key to the success of this complicated restoration was to have a plan. In the author’s opinion, the ability to treatment plan with the dentist partner to achieve ongoing success will continue to be the key to the dental technologist’s esthetic, functional future (Figures 36 through Figure 38).
About the Author
Peter Pizzi, CDT, MDT, FNGS
Owner and Manager
Pizzi Dental Studio, Inc.
Staten Island, New York