Team Challenge
All-ceramic single anterior crowns with translucent zirconium-dioxide frameworks.
By Haristos Girinis, MDT; and Ernst Peter Drescher, DMD
The patient’s desire to have perfect teeth must be accompanied by the clinical responsibility of the treatment team. Successful results can only be established on a healthy foundation. This is where the monitoring of “biologic width” plays an important role. While this term is sufficiently well-known in the world of specialists, it is still not practiced by many dental practitioners. Nor is it practiced in the interaction between dental technology personnel and dental health professionals. In this case report, the authors demonstrate their well-coordinated teamwork for restoring six maxillary anteriors with zirconia-supported crowns.
A 70-year-old man consulted the dental practitioner regarding his desire to replace his anterior crowns, which had been fitted 15 years previously. He was unhappy with his old crowns as the color and shape no longer met his esthetic requirements. In addition, the patient’s wife previously had prosthetic treatment with the authors and was very satisfied with the results. This motivated the patient to get his anterior teeth re-crowned.
In order to better facilitate communication and teamwork, the clinical aspects were intentionally taken into consideration and highlighted at the presentation of the case.
Initial Situation
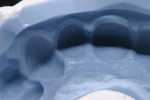
At presentation there was no presence of functional discomfort, and dental hygiene was good. Teeth Nos. 13 to 23 were fitted with all-porcelain crowns (Figure 1 and Figure 2), which were not loosened, and no pathological findings were revealed with the primary and X-ray examinations. The original crowns had been in place for 15 years and were no longer functioning in total harmony with the patient’s natural dentition. The periodontium seemed healthy at first glance. There was a periodontal biotype B, ie, a “robust” periodontium. An injury to the gingival structures could not be identified in the initial examination; however, with more precise examination, an inflammatory alteration to the gingiva in the anterior region was visible. The reason for gingival inflammation stemmed from the poor marginal fit of the existing crowns and the edges of the crowns protruding far into the subgingival region.
The infringement of biologic width due to the crown edges lying too close to the bony alveolar ridge (Limbus alveolaris) could mean a case of iatrogenic, chronic, marginal periodontitis. After removal of the unsatisfactory crowns, this suspicion was confirmed. The infringement of biologic width is clearly visible in Figure 3 —there was hardly any presence of gingival sulcus. Correctly assessing the type of soft tissue is an essential component of the authors’ treatment concept, as anterior teeth can only be successfully crowned with a satisfactory mix of white and red colors.
This case included several challenges:
- The biologic width had been damaged. Therefore, new crowns without the length of said crowns being extended to reconstruct the biologic width were not possible.
- Periodontal surgical intervention for the reconstruction of the biologic width required the removal of the existing, insufficient restorations.
- Only laboratory-produced, long-term temporaries sitting in exactly the right place would guarantee undisturbed healing after periodontal surgical intervention.
- Final crowning had to fulfill the requirements of the patient in terms of esthetics and functionality.
This article explains how these problems were successfully solved with collaboration between the dentist and the dental technician.
Biologic Width Reconstruction
The physiologic width of the connective tissue attachment and of the junctional epithelium is an average of 2 mm and is defined as the “biologic width.” The depth of the penetration of the periodontal sensor is dependent on three factors, which include force applied, the extent of the periodontal inflammation, and the location of the tooth. Therefore, it is clinically more practical to determine the entire width of the dento-gingival complex (connective tissue attachment, epithelial attachment, and sulcus).1
What is measured is the distance from the gum margin to the bony alveolar ridge. With a healthy periodontium, the buccal distance is around 3 mm and the interproximal distance typically ranges from 3 mm to 4.5 mm. The extent of proximal variance depends on the characteristics of the Limbus alveolaris. Clinically, it is determined whether the patient has a “high crest” (dento-gingival complex < 3 mm), a “normal crest” (dento-gingival complex = 3 mm), or a “low crest” (dento-gingival complex > 3 mm).
Markus Schlee, DMD, defined two possibilities for the reconstruction of the biologic width:
- The orthodontic extrusion of the tooth. Here, the tooth is moved out from the gum, a treatment method not considered for this patient due to the length of time it takes.
- Surgical crown lengthening. Here, a mucoperiosteal flap in the area of the marginal bone is activated and lifted. About 3 mm of the alveolar ridge is removed (ostectomy), and the “bone ridges” that result are modelled into a natural physiological shape (osteoplasty). With insufficient width of the keratinized gingiva, the soft tissue flap is apically repositioned in the form of a split flap and stitched in that position.
In the end, the authors decided on the second method for the surgical crown-lengthening procedure.
In order to provide the patient with an interim dental prosthesis, the dental impression was made using a double-flap technique with hydrocolloid. The short-term interim prosthesis was manufactured with the help of the deep-drawing technique. This efficient method enabled the patient to be discharged with an adequate solution until the next appointment.
Surgical Crown Lengthening
At the beginning of the surgical intervention, the bony alveolar ridge was located and the thickness of the gingiva determined using “sounding” or manipulating the socket of the epithelial attachment (Figure 4 ). The epithelial attachment should lie about 2 mm apically from the preparation margin.
The course of the incision depends on the width of the gingiva. In this case, Dr. Drescher started with a sulcular incision, whereby the injured junctional epithelium must be left alone (Figure 5). This incision resulted in the preparation of a split palatal and labial flap. In order to prevent the interdental papilla from being damaged as much as possible and to keep tissue shrinkage and postoperative pain as low as possible, only as much gingiva was opened as was needed for a good overview.
Following the lifting of the split flap, the epithelial collar is then visible (Figure 6 and Figure 7). Then the junctional epithelium was detached from the tooth with an incision close to the tooth (Figure 8). With a horizontal incision, the periosteum was cut in two so that the junctional epithelium could be removed at the height of the papilla base (Figure 8 and Figure 9).
The apical repositioning of the Limbus alveolaris was carried out with a diamond-coated tip (Figure 10) and a diamond-coated cutting tool. In order to achieve a harmonious bone structure, approximately 3 mm to 4 mm of healthy subcrestal tooth enamel must be exposed during the bone re-section. With the help of a dental handpiece, the root surfaces were worked on to avoid any injury to the tooth. Subsequently, the root dentin was smoothened and conditioned with Emdogain (Straumann, www.straumann.us), and the positioned papilla was stitched (Figure 11, Figure 12 and Figure 13). The patient received a short-term interim prosthesis.
Long-Term Temporaries
Following the removal of the stitches and the healing of the tissue, an impression was taken. In the dental laboratory, the dental impressions were poured in order to finish the working model (Figure 14). On the basis of the articulated model, a plaster model was made that fulfilled both the esthetic and functional aspects. This plaster model served as a template for the creation of the long-term temporaries (LTTs). For the plaster model, palatal grinding was undertaken on the assembled prosthetic teeth and positioned in front of the prepared plaster die with wax (Figure 15). The shape of the teeth was completed basally and, in parts interdentally, with the same wax (Figure 16). The plaster model was then mounted on a silicone key (Figure 17). The silicone key and plaster die were then given an appropriate coating (Figure 18 and Figure 19) and transferred into teeth-colored plastic (auto-polymerizing) using the silicone key (Figure 20). The provisional plastic bridge was removed from the silicone key after polymerization (following manufacturer’s instructions) and roughly trimmed with a scalpel and rotating instruments so that it could be easily fitted back onto the model.
An important prerequisite for LTTs is their stability. Ultimately, they should be worn by the patient for 4 to 5 months. In this case, the requirement for stability was achieved through a palatal metal support. After marking the desired area for strengthening (Figure 21), the support was then cut with a milling machine and filled with stable modeling wax. Using the same wax, the fragile areas were strengthened and modeled (Figure 22). The support was provisionally attached, carefully taken off, and cast in non-noble metal. The resulting piece of metal was prepared and polymerized with the same tooth-colored plastic (Figure 23). The final controls and the bedding-in of the static and dynamic occlusion then took place on the articulator (Figure 24).
From a frontal position, the LTTs’ metal support cannot be seen (Figure 25). As the basal portion of the temporaries never conforms completely to the impression, a transfer key made of light-curing resin was produced (Figure 26). The LTTs were adjusted in the mouth and secured with carboxylate cement.
Impression for the Final Crowns
After the LTTs were in the patient’s mouth for 4 months, the six maxillary anterior teeth were further treated (Figure 27) and an impression was taken with hydrocolloid impression material. With the double-flap technique, the marginal tissue can be pushed back somewhat so that the preparation margin, located just underneath the gingival, can be molded precisely and without the use of any pressure. Hydrocolloid impressions are precise; however, they sometimes dry out and shrink when exposed to the air. Therefore, urgency is needed when working on them. Since the dental laboratory was located adjacent to the practice, hydrocolloid was the authors’ method of choice.
In the laboratory, the two molds were painstakingly poured and two models created: one master model, or working model, with detachable individual dies, and an unsectioned control model. While processing the model dies, it is best not to uncover the preparation margins; they uncover themselves during the grinding of the dies. The double-flap technique makes this possible. The sectioned model was cast and mounted against the lower jaw already articulated for the production of the LTTs.
Final Restorations
The esthetic planning of the final restorations was completed with the development of the plaster model. Again, this forms the prototype for the LTTs and provides information regarding the length, width, and position of the front teeth as well as the ability to check proper phonetics and functionality. All data gathered from the LTTs were, therefore, transferred piece by piece onto the final restorations.
In order to offer the patient the maximum level of esthetic quality and long-term stability from a prosthetic point of view, an all-ceramic restorative option was selected. Several forms of all-ceramic restorative options exist, including pressed-ceramic restorations and porcelain-layered crowns on ceramic-oxide frameworks. Various published articles attest to aluminium-oxide-based restorations having a better esthetic quality than zirconium-dioxide-based restorations with regard to light transmission.2
In contrast, pressed-porcelain restorations feature almost the same level of light transmission as natural dentin, with the former being 60% and the latter 58.69%. In a dissertation some years ago, Daniel Edelhoff, CDT, DMD, PhD, highlighted the fact that a higher level of light transmission is accompanied by lower flexural resistance. Partially stabilized zirconium dioxide performs somewhat worse here in direct comparison, with a light transmission level of 45.25%. Therefore, the choice of framework material or the form of the restoration is also always a compromise between the highest possible esthetic quality (higher light transmission levels) and stability (flexural resistance).
In this case, the opportunity presented itself to choose a new zirconium- dioxide material made by Wieland Dental (www.wieland-dental.de) for the production of the crown frameworks. The ZENO® Zr Bridge (translucent) is a translucent zirconium dioxide that the manufacturer has approved for bridges of up to 14 units.
Comparing the technical data stated in the data sheet with the data from the proven ZENO® Zr Bridge (white),3 it became clear that both materials feature the same level of flexural resistance of 1,100 MPa with the same composition.4 Therefore, it was determined that the frameworks would be manufactured from the new translucent zirconium dioxide.
Centrally Manufactured ZrO2 Frameworks
The frameworks were manufactured from the translucent zirconium dioxide ZENO Zr Bridge with the ZENOTEC CAD/CAM system (Wieland Dental). A dental laboratory specializing in this technique digitized the model data and constructed the framework. The authors’ partner laboratory used the key and the information from the plaster model to design and produce the frameworks so that they provided the desired functions. To avoid unwanted surprises, it is best to provide the milling center with all information available. In this case, both the sectioned model and the plaster model were provided to the center.
Using a double-scan technique, the technician in the partner laboratory designed a framework that was optimal in anatomical terms (Figure 28, Figure 29, Figure 30 and Figure 31). Figure 32 shows the milled ZrO2 frameworks on the sectioned model. The right-hand side of Figure 30 shows what was designed with the CAD software. Using diffused transmitted light, the nature of the material becomes clear (Figure 33) and the plaster die gleams—an indication that the material is very translucent. In the mouth, the natural tooth stumps extended into the dental restoration and, therefore, reinforced the positive effect. This is promising, as zirconium-dioxide-based restorations have been problematic in the past, particularly in the esthetically sensitive transition area between the gum and artificial crown.
Because the authors work with very low levels of veneer porcelain layer strengths, the “white” ZrO2 frameworks would have radiated through in this area, which is why, overall, the ZrO2 restorations would have appeared unnatural. Therefore, both requirements— esthetics and stability—were fulfilled with the translucent zirconium dioxide.
Although it sounds like a contradiction, the dark cervical area that appeared with LTT restorations with shoulders now was too bright with the ZrO2 restorations. This area—where the natural clinical crowns rise from the gum—is where all optical alterations lead to confusion, and clinicians tend to think something is wrong. Many of the authors’ colleagues, for example, have switched over to toning the throat area with pink effect material to imitate the natural radiation of the gingiva.5 The milled framework’s fit is noteworthy.
Cervically, the framework can even be prepared to be thin, which benefits light transmission and the veneering. The big advantage to CAD/CAM-produced frameworks lies in the fact that there is no more elaborate preparation work needed to fabricate the framework. This time-saving benefit ensures a less stressful, more comfortable time working on the framework, allowing more energy and dental expertise to be concentrated on imitating the subtle tooth structures.
The processing of sintered zirconium-dioxide frameworks is a controversial subject. For example, if sandblasting the framework, how much pressure should be used and with what size of grain? One thing is sure, when sandblasting the zirconium-dioxide surface, the structure changes. Presently, there is no universally accepted evidence, meaning that dental technicians have to decide on their own approach. The frameworks in this case were sandblasted equally using aluminium oxide (Al2O3) and a grain size of 50 µm at low pressure (around 1.5 bar). The framework was cleaned and all fat and other impurities were removed. The framework was then placed in a ceramic oven at 1,050°C for 15 minutes to “fire cure.”6 This then leads to the framework being purified and, therefore, an increase in the wettability.
Individual Veneering Porcelain
The patient wanted that famous “perfect smile” and chose tooth color A2. Zirconium dioxide is not fluorescent. However, because the fluorescence of porcelain is important for the natural look of an artificial tooth, the use of fluorescent shoulders was necessary. In such cases, the implementation of fluorescent liner materials is not suggested as they are too opaque and would lead to a ridiculously positive side effect with regards to the zirconium dioxide. The shoulder was, therefore, in correspondence with the selected tooth color, separated from the framework surface, wetted with modeling liquids, and fired at 980°C.
At this temperature, the porcelain fuses more strongly, meaning that the surface of the framework is wetted better. This improves the bond at the problematic ZrO2 veneering porcelain interface. In addition, the surface is given a grainy quality through the sandblasting. This prevents the framework from being too strongly defined underneath the veneering porcelain, and the rough surface allows the subsequent layers of porcelain to be applied more easily. The frameworks that were modified in this way are shown in Figure 34.
First Firing
For the first firing, the crowns were assembled from a cervical direction to an incisal direction. The layering was done from the inside outward, as if the tooth was growing again. By firing in several layers, the esthetic effect of the crown becomes predictable. A clear and well-developed procedure is extremely helpful in achieving reproducible results. For the first firing, three types of material were used (in this case red, blue, and yellow). As the chroma decreases incisally, layering started from the root with a highly chromatized material (red) and phased out with less dentin (blue). A smooth transition is important to avoid having unnaturally defined lines of separation (Figure 35). The dentin core was layered at a smaller anatomical scale, following the anatomical requirements of the ZrO2 framework. Then the fluorescent dentin material, which increases the light transmission in the interior of the crowns, was soaked incisally—as that is where the light comes from—in the already coated materials (yellow). Again, no hard transitions should be imitated, rather soft and flowing ones (Figure 36).
After the first firing, the base of the restorations guided the geometry of the tooth stump from the inside to the outside, and supplemented it with a further characteristic feature (Figure 37). In this way, each porcelain layer, and the desired effect associated with it, remains under control and the dimensions can be better controlled. Following this procedure prevents the color effect and the chroma of the crown to distort through the application of too much enamel material or transparent material. Each porcelain layer was divided into different firings to apply full technical expertise to each layer. Consequently, a second dentin firing and then an incisal firing followed.
Second Firing
The tooth structures were supplemented with dentin (rosé). Because the papilla should be illuminated, the proximal contact areas were joined with fluorescent dentin material (yellow), which was also mixed with dentin modifiers (Figure 38). This generated an extremely intensive color and therefore, contrast and vitality, or depth and the light transmission into the papilla, were controlled. With the help of the so-called “enamel cone,” the outer frame of the vestibular veneer was roughly defined (Figure 39). Therefore, the existing information regarding the outer contours of the teeth to be copied was transmitted tooth-for-tooth onto the layering palette using the aforementioned enamel cone or palatal ridges, upon which the centric contact later came to rest (Figure 40).
A palatal base, or so-called enamel plate was created (Figure 41), upon which—in a similar way to a picture frame—the dentin was submerged from the vestibular side. However, before this procedure could start, a flat surface on the enamel plate had to be created using a dental tool. The palatal enamel base indicates the outer contour of the tooth (Figure 42 and Figure 43). If one was to cut through the layering at the sagittal layer, then it would become apparent that the dentin and the plate are similar to a ying/yang situation. In the cervical area the amount of dentin is greater and this amount then reduces in the incisal direction, and the amount of enamel then subsequently increases.
Often, the palatal area is prepared to a lesser extent than the vestibular area. This fact must be compensated for with porcelain layering complementing the palatal proportion of the tooth with enamel.
Another positive effect of the enamel plate is that the natural moisture balance of the materials in the vestibular area is secured. In addition, the dentin used can be submerged, which avoids well-defined transitions and gives the impression of a tooth that has grown naturally. The fired dentin core acts as an additional control over the dimensions of the structures and is a controlling factor in the cutback process.
More fluorescent dentin was then applied to the dentin layer, which radiated through to the dentin. With the fluorescent dentin layer, the dentin cones were imitated, as these cones are easily visible with naturally growing teeth (Figure 44). Using effect materials, intuition is required. Here the age-old saying really counts: less is more. Having moist porcelain is just as important as the correct handling of the effect materials. A good modeling fluid is worth its weight in gold. The porcelain materials should be stable but also be able to be molded.
The artificial teeth grew slowly, and the space visualized with the silicone key from the plaster model disappeared. With the dentin set, the enamel and incisal layers were begun. Before this, an intermediate layer was created representing the transition from dentin to enamel. In cross-sections of teeth, this enamel-dentin border is always represented as a transparent strip, which is sometimes tinged a little gray or blue.6 This layer is imitated by covering the dentin layer in a thin coat of transparent material (Figure 45). The transparent layer provides the entire restoration with a certain degree of three-dimensionality and depth. In this case, Transpa Neutral (Ivoclar Vivadent, www.ivoclarvivadent.com) was used. The last ridges of this transparent layer were applied with a slight blue tinge. The material used was salmon-colored in the incisal area (Figure 46 ). This area later develops into the so-called “incisal fire,” meaning that the interplay between the dentin cones and the enamel generates the impression that the tooth is natural.7 Now, the second layer can be fired at 900°C. As the incisal edge is somewhat worn down during the development of the occlusion and the function of the restoration, the bluish edges remain in place.
Results After the Second and Third Firing
The results directly after the second firing can be seen in Figure 47. The bluish transparent effects are quite clear in this image, and it is evident how the dentin radiates into the incisal layer. From the overview, the spatial depth of the veneer is seen more clearly (Figure 48). The similar structure of the fired porcelain is shown in Figure 49. So-called “black triangles” were created in the proximal area to close up this space.
Before proceeding to the enamel layer, any existing problematic structures must be ground away. In this case, as the authors proceeded in a step-by-step fashion, no grinding was necessary.
The most important factor for the reproduction of natural layering is to work in as high a contrast as possible. The inside of the tooth is highly chromatic and as a more definitive tooth shape takes form in the layering process, the tooth becomes brighter and whiter. Depth is simulated with the aforementioned transparent layer that separates the two-colored layer, one color from another.
Again, this was followed by application of enamel material in the palatal area. This enamel was supplemented by a small amount of Opal Incisal (Figure 50). By starting from the palatal area, the anatomy of the tooth was defined, which merely had to be supplemented by the appropriate incisal materials in the frontal area. In this case it was a transition layer from incisal 2 and 3 (Figure 51).
The authors started cervically and guided chromatic opal material (Opal Incisal and Opal Effect) along the mesial ridge in an incisal direction (Figure 52). The prominent parts of the shape of the tooth were accentuated more strongly, as these parts were milled the most during the finalization of the fired crowns. Through the application of a belt-like diagonal band, it was possible to add torsion to the crowns, which gave the impression of three-dimensionality (Figure 53). Then the restorations were fired at 900°C once again. With ZrO2, the heating rate is dependent on the volume of the framework as ZrO2 tends to act as an insulator and not transport heat like metal frameworks. Reducing the heating rate counteracts the heat being drawn off by the framework.
Finalizing the Fired Crowns
The fully fired and relatively unspectacular result is shown in Figure 54. The level of transmitted light again makes the framework material’s high translucency clear (Figure 55). The condition of having been fired, but not yet ground roughly, shows the slightly oversized shape of the tooth (Figure 56).
Fabrication was now switched from an additive, step-by-step process to a subtractive one. Now the untreated, fired crowns were adjusted in terms of the following functional factors. Nature serves as the role model: the virgin tooth grows from the inside out (in layers) and adjusts itself to functional factors through attrition and abrasion (development of the functional and guidance surfaces as well as contact relationships through mechanical abrasion). The natural erosion of the tooth is simulated through mechanical processing not only by grinding the protrusion and later obtrusion movements using stone and diamond, but also by developing the growth striations and other morphological characteristics. After this was done, the teeth were polished, which likewise orientates itself on the natural form (food that is abrasive both mechanically and chemically). Through this, the enamel layer was reduced in a manner corresponding to natural factors (eg, more strongly in the protruding areas than in the grooves). The surface radiance of the teeth was adjusted with age due to mechanical and chemical influences.8
In a lateral view of the canine tooth crown, the three horizontal curved surfaces on the vestibular surface of the tooth are visible (exaggerated). The first is the curved surface, which marks the cervical area, then a central level, from which the tooth tilts strongly in the incisal direction (Figure 57). From the frontal view, the three curved surfaces, as well as the ridges, are again visible with synthetic supports transferred onto all of the crowns. The latter defines the visible width of the tooth (Figure 58). The vestibular surface was roughly smoothed down and then the curved surfaces added accordingly. From then on, all other features were not applied in layers anymore, rather, they were systematically introduced with precision rotating tools. The aforementioned ridges or light reflection layers allow adjusting the visible width of the tooth with the space available—for example, making a wider tooth narrower. Generally, during processing with rotating tools, it is important not to ruin what was so carefully constructed in the first place. With mechanical processing, it is not about fixing mistakes; it is about mechanically highlighting applied characteristics and features.
When the vestibular surface is processed according to the markings, three vertical surfaces are created that are separated from one another and get even closer to the natural anatomy of a tooth (Figure 59): a mesial proximal surface, a vestibular surface, and a distal proximal surface. In addition, a central ridge applied on the vestibular surface breaks off at the bulge of one of the hollows and, following the root of the tooth, appears to originate from the gum. A second ridge, which is marked distally and above the first one, marks the upper bulge of the hollow. Both hollows meet in a cervical direction. With these hollows, the tooth’s torsion was supported, which was highlighted during the layering process (Figure 60). In addition, these hollows guaranteed that the vestibular surface would not emerge from the gum in a rounded fashion, but rather flat. The porcelain crowns already looked like teeth. The basis form was there and the precise structures were able to be developed even further. To see exactly where and to what extent adjustments would need to be made, the crowns were sprayed with water from a vaporizer.
The next step was the arrangement of the incisal triangle, which had to be opened. Doing this creates a kind of gateway for the palatal and vestibular surfaces (Figure 61), and this generates the so-called curved features of the teeth ( Figure 62). Then the authors drew the distal-incisal third from the vestibular area in a palatal direction (Figure 63), creating smooth transitions for the crowns in the disto-incisal area and giving the individual crowns physical characteristics (Figure 64). The physical form of the crown surface was now addressed. The idea was to create a virgin tooth as a basis (Figure 65) and then—just as in nature—adjust correspondingly to the abrasion of the impression.
Initially, the growth striations were marked and then processed correspondingly. The growth striations in natural teeth start in small arches in the incisal area and progress in parallel, increasing in size and then thickening in the area of the vestibular center of the tooth so that they then drift away from each other in a cervical direction. It was necessary to transfer this onto the artificial crowns (Figure 66). It is important that these growth striations run around the whole of the body of the tooth because these lines survive to be stronger in the protected areas whereas those in the areas that are more active suffer more abrasion (Figure 67). By observing and imitating this, natural effect reflections can be achieved with artificial teeth.
Finally, the surface structures that developed in an exaggerated manner were then smoothed with a sandpaper cone—starting with rough sandpaper and finishing with fine sandpaper. Overall, it can be said that younger teeth are rougher and wilder, and older teeth have a smoother surface. The surface on which the sandpaper was used had to then be pre-polished with a rubber wheel (Figure 68).
Developing the Contact Zones
After the shape and surface of the artificial crowns were completed, occlusion and function could begin to be addressed. In the articulator, the centric stops on the palatal bulges were marked with black occlusion foil. This foil may not be removed at all (Figure 69). As will transpire, the esthetic quality of the crowns was also refined through functional development. As appropriate free space was created at the incisal edges, the typical tooth shape was simultaneously refined, improving the esthetics (Figure 70). In this way, the complex form of natural teeth was copied piece by piece and transferred to the artificial crowns. Also, resulting from this was the final length of the anterior teeth and the contour of the incisal edge—from symmetrical virgin teeth to asymmetrical teeth marked by real life. The reason for this can be found in the lower jaw.
To prevent the crowns from falling from the model during the grinding process, they can be secured with Tac Gel (Dental Ventures of America, Inc. www.dentalventures.com). Prepared in this manner, the previously indicated excursion movements could be carried out and displayed with appropriately colored occlusion foil (green = laterotrusion, red = protrusion) (Figure 71, Figure 72 and Figure 73).
Final Finishing
Before the degree of gloss was set, the proximal contact points, and also primarily the strength of the contact, had to be checked with the help of shim stock strips on the control model (Figure 74). Then the surfaces of the crowns (Figure 75) were fused in a so-called modified gloss-firing procedure at around 880°C (approximately 20°C below the temperature of the dentin firing). With regards to the results of the modified gloss-firing process shown in Figure 76, no glass frit was used; however, some paint was used to accentuate certain areas. This helped achieve an equally fused surface, upon which all previously developed features survived. The final degree of gloss was set through mechanical polishing using an initial mixture of fluid polish and a little water and then a mixture of fluid polish, pumice powder, and water. This resulted in a creamy “polish ointment,” with which the degree of gloss can be adjusted extremely well. The direction of polish is extremely important here: first from side to side, then from top to bottom. The latest generation of layered porcelains are fine-grained so that they are thicker after firing. Therefore, the goal of polishing—at least with most porcelain systems—is no longer to thicken the surface, but rather to adjust the degree of gloss on each individual set (Figure 77, Figure 78 and Figure 79). The level of transmitted light of the six anterior crowns illustrates their warm and bone-like character (Figure 80).
And with reflected light on the sectioned model, the zirconium-dioxide-based crowns also looked very natural (Figure 81). At the end, the finished crowns were once again photographed on the reflector so that the light qualities of the translucent zirconium dioxide and ZIROX veneering porcelain (Wieland Dental) were able to be better emphasized (Figure 82 and Figure 83). The bone-like, toothy color comes about from the fact that the veneering porcelain can shine in the zirconium-dioxide framework, giving the impression that they are pressed porcelain crowns.
Final Seating
After fitting the six maxillary anterior teeth, Dr. Drescher let the patient look at his new teeth in the mirror. Of course, the final outcome was a big difference, as the patient went from having old, very short teeth to having longer, considerably whiter crowns. Initially the patient’s reaction was critical (Figure 84), but as he played around with some facial expressions (Figure 85), he became happy with his new smile (Figure 86).
Figure 87 shows a close-up of the crowns directly after being fitted. When the patient came to a check-up visit a few weeks later, it became apparent that the gingiva had been regenerated (Figure 88, Figure 89 and Figure 90). If the case results are compared with the natural teeth in the lower jaw, it becomes clear that, with the help of the new combination of materials, the profession has taken a huge step toward the goal of coming as close as possible to natural teeth. The patient had wanted a lighter tooth color (modified A2) that contrasts sharply with the A3.5 color of the mandibular teeth.
Conclusion
If the authors compare what they produced with natural teeth, it becomes clear that dental practitioners will never win the battle against nature. However, with a team-oriented treatment concept and modern materials, the dental profession is approaching the goal of producing artificial teeth that appear natural.
References
1. Kois JC. The restorative-periodontal interface: biological parameters. Periodontol 2000. 1996;11(1):29-38.
2. Haase U, Thiel H. Der Werkstoff Zirkondioxid unter der Lupe. Dent Dialog. 2007;9:76-86.
3. Stawarczyk B, Sailer I, Zahno X, et al. Metallfreie, zirkoniumdioxidbasierte Rekon- struktionen – Bearbeitungsschritte zum Erfolg. Dent Dialog. 2009;1:84-102.
4. WIELAND Dental + Technik. ZENO Materialien, 530080d.02.05/09
5. Broseghini C. Die Bio-Schichtung: Dentin- schichtweise bei ZrO2-Versorgungen zum natürlichen Ergebnis. Dent Dialog. 2009;8:60-6.
6. Kohler W. Schichten mit Signum matrix – mehr als nur ein Komposit. Dent Dialog. 2007;8:90-101.
7. Nolte A. Schlichte Frontzahnästhetik – erste Etappe einer Wegbeschreibung. Dent Dialog. 2003;1:8-27.
8. Girinis H. Abnehmbare, implantatgetragene Suprakonstruktion im Oberkiefer – Teil 3. Dent Dialog. 2008;5:108-15.
About the Authors
Haristos Girinis, MDT
Girinis Dental Design
Nagold, Germany
Ernst Peter Drescher, DMD
Private Practice
Stuttgart, Germany