Treating Sensitivity and Gingivitis from Xerostomia
A new option to relieve and prevent complications from dry mouth
Xerostomia, or dry mouth, is a condition that can have serious implications for oral health and patient quality of life. The prevalence of dry mouth in the general population is difficult to accurately measure; prevalence rates from 0.9% to 64.8% have been reported.1 Its diagnosis is complicated by the fact that xerostomia is reported subjectively and can have various causes, including medication use, salivary gland dysfunction, and certain autoimmune diorders.2,3
Patients with dry mouth can present with a variety of symptoms, including difficulty speaking or swallowing, sore throat, and hoarseness.4 Dentists may also encounter gingivitis, sensitivity, and increased caries rates in patients with dry mouth,5 which can further complicate treatment protocols and cause patients more frustration, discomfort, and time/expense in the dental office.
Dental professionals can suggest that patients use a special gel or rinse designed to keep their mouths moist. If patients are also at risk for developing caries, dentists might also prescribe a toothpaste or mouth rinse that contains fluoride, apply a fluoride gel, or give the patient a fluoride rinse during their office visit.6 Other ways patients may find relief include:6
· chewing sugar-free gum or sucking on sugar-free hard candies to stimulate salivary flow.
· sucking on ice chips.
· sipping water with meals to aid in chewing and swallowing food.
· using alcohol-free mouth rinse.
· avoiding carbonated drinks (like soda), caffeine, tobacco, and alcohol.
· using a lanolin-based lip balm to soothe cracked or dry lips.
A challenge to manage symptomatically, xerosomia’s oral health implications can severely impact patients’ daily health and function and prove to be a source of frustration to dental health professionals.
Case Presentation
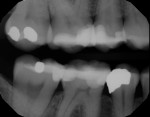
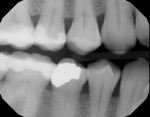
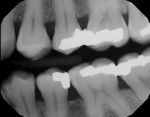
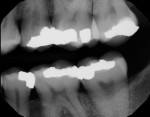
A 37-year-old woman presented with an autoimmune neurological disease (complex regional pain syndrome, previously known as reflex sympathetic dystrophy syndrome) that caused her to experience severe dry mouth discomfort and increasing sensitivity. Recent bitewing radiographs (Figures 1 through 4)show the result of her constant battle against caries, as most of her posterior teeth have been restored. The patient had 17 fillings in the past 5 years, with nine of these in the past year alone. The patient described her symptoms as an “extremely dry and very uncomfortable” mouth and “extremely sensitive” teeth that made it very difficult to drink anything cold.
Initial attempts to alleviate her symptoms included the use of both over-the-counter and prescription-strength products. These provided temporary, short-term relief; however, this long-time patient nevertheless experienced a worsening of her condition and symptoms over time.
Upon clinical examination, the patient’s mucosa was tight and dry. She reported that her lips were often dry and cracked, which caused her to constantly use a moisturizer. In addition, her tongue was often dry and felt rough, and she had trouble swallowing and difficulty speaking due to the lack of lubrication from the absence of saliva. She also complained that she was unable to flush debris from her mouth, which often caused her throat to tickle or feel hoarse.
In addition to these ongoing symptoms, the patient was beginning to experience severe gingivitis and increasing sensitivity. She was constantly returning for restorative work to fight an ever-increasing battle against caries.
Treatment
In the past 5 years, attempts at treating the patient’s condition with every available option had only at best relieved her dry mouth discomfort for a short period of time each day, had not been able to reduce her sensitivity or gingivitis, and did not manage or prevent caries as effectively as the author had hoped.
To protect against complications, it has been recommended that dental professionals encourage patients with dry mouth to use a dentifrice that provides as many of the following benefits as possible: strong caries protection, sensitivity reduction, demineralization resistance, and lubrication of mucosa.7 With this in mind, the author decided to give the patient a sample of Enamelon® Preventive Treatment Gel, a new product from Premier Dental Products (www.premusa.com), to discover if this stannous fluoride treatment gel delivering amorphous calcium phosphate (ACP) could help her. According to the manufacturer, Enamelon contains 970 ppm fluoride and is free of sodium laurel sulfate, gluten, and dyes.8 Although it is only available to patients through their dental offices, it is classified as an over-the-counter product.8
After a restorative appointment, the patient was given a 4-oz tube of Enamelon Preventive Treatment Gel and instructed to brush at least in the morning and evening with a dry toothbrush so the product would not be diluted. After 2 minutes of brushing, the patient was instructed to spit and not to rinse, eat, or drink for 30 minutes. The author advised the patient that this product is designed to help prevent caries and gingivitis, relieve sensitivity, and may even help to relieve the discomfort of her dry mouth. It was suggested that the patient replace her current treatment protocol, which provided only temporary relief despite using the product almost six times a day, with Enamelon for several days to test its efficacy in her case. Further, if she felt like it was not helping, she was to immediately return to the protocol that did provide some relief.
Recall Appointment
Two weeks later, the patient returned for her follow-up appointment and said that the level of sensitivity and dry mouth discomfort she had been experiencing was cut in half from its previous rating of “severe.” Additionally, she reported the relief from dry mouth discomfort she experienced using Enamelon was more “permanent” than her previous protocol, even though she only used it two times a day.
The follow-up intraoral examination revealed that the mucosa did not appear to be as dry (Figure 5) and more saliva was present in the oral cavity. The patient reported that her mouth felt “more slippery,” making it easier for her to talk and swallow. She also noted that she would recommend the product to others suffering from the same condition and symptoms.
Although this is an anecdotal reporting of one experience using this new product, this patient experienced excellent initial clinical results and symptomatic relief. Considering the long history of this case and the amount of suffering she has endured, both patient and doctor were satisfied with the promising treatment offered by Enamelon Preventive Treatment Gel.
Discussion
The science behind Enamelon explains how it helps relieve the dry mouth discomfort and sensitivity that was experienced in this case. Fluoride ions in saliva are not as effective without the presence of sufficient calcium and phosphate ions.9 Enamelon offers remineralization benefits in part because its formulation includes the technology to deliver ACP. In addition, the product features mucoadhesive copolymers and Ultramulsion®, a patented, saliva-soluble, long-lasting coating that may lubricate and soothe the soft tissues of the mouth and may provide improved therapeutic performance by enhancing substantivity.8 The combination of these components allows for the formation of loosely bound calcium fluoride reservoirs that serve to promote remineralization and inhibit demineralization.8 Indeed, Enamelon has been shown in in vitro studies to provide almost 2.5 times greater fluoride uptake10 and 3 times greater resistance to demineralization11 than prescription strength, 5000-ppm fluoride toothpastes.
Conclusion
One major challenge in dentistry is to decide which treatment may be best for each patient. For patients who report similar problems with sensitivity, gingivitis, high caries rates, and dry mouth discomfort, Enamelon is a new option that could prove as effective as in the case example here. The author has since recommended it to other patients with similarly positive results. The safety of this 970-ppm fluoride gel and the in vitro data showing that it outperforms prescription products with five times the amount of fluoride makes it an excellent option for many patients.
For more information, contact:
Premier Dental
888-670-6100
www.premusa.com
References
1. Orellana MF, Lagravère MO, Boychuk DG, et al. Prevalence of xerostomia in population-based samples: a systematic review. J Public Health Dent. 2006;66(2):152-158.
2. Guggenheim J, Moore PA. Xerostomia: etiology, recognition and treatment. J Am Dent Assoc. 2003;134(4):61-69.
3. Navazesh M. How can oral health care providers determine if patients have a dry mouth? J Am Dent Assoc. 2003;134:613-618.
4. Dry mouth. American Dental Association website. www.ada.org/en/Home-MouthHealthy/az-topics/d/dry-mouth. Accessed April 20, 2015.
5. Xerostomia. The Oral Cancer Foundation website. www.oralcancerfoundation.org/complications/xerostomia.php. Accessed April 20, 2015.
6. American Dental Association (ADA) Division of Science. Managing dry mouth. J Am Dent Assoc. 2015;146(2):A40. doi: dx.doi.org/10.1016/j.adaj.2014.11.019.
7. Croll TP, DiMarino J. A review of contemporary dentifrices. Academy of Dental Therapeutics and Stomatology website. www.ineedce.com. Accessed April 20, 2015.
8. Enamelon: the new standard of caring [product brochure]. Premier website. www.premusa.com/dsp/Enamelon_Brochure_R6.pdf. Accessed April 20, 2015.
9. Schemehorn BR, Orban JC, Wood GD, et al. Remineralization by fluoride enhanced with calcium and phosphate ingredients. J Clin Dent. 1999;10(1 spec. no.):13-16.
10. Schemehorn BR, DiMarino JC, Movahed N. Comparison of the incipient lesion enamel fluoride uptake from various prescription and OTC fluoride toothpastes and gels. J Clin Dent. 2014;25(3):57-64.
11. Schemehorn BR, DiMarino JC, Movahed N. Comparison of the enamel solubility reduction from various prescription and OTC fluoride toothpastes and gels. J Clin Dent. 2014;25:61-64.