Systematic Rotary Instrumentation for Composite Restorations
Patient-friendly system offers conservative cavity preparation and also finishes and polishes nano-microhybrid composite restorative materials.
Dental histology reveals that pit-and-fissure caries often starts as a “pin point” lesion that expands in a triangular shape as it progresses toward the dentino-enamel junction (DEJ). Once the lesion penetrates the DEJ, the caries spreads laterally and pulpally at a much more rapid rate due to the relative “softness” of the dentin as compared to harder enamel. So, it stands to reason that, based on the histologic progression of tooth decay, initial penetration into the lesion should conserve as much of the healthy enamel as possible while allowing sufficient access to instrument the dentin and remove the softer carious dentin leaving healthy, mineralized dentin behind. This article will detail the use of a caries removal and preparation system that helps the dentist accomplish these goals, while limiting the use of anesthesia, thus increasing patient satisfaction among needle-phobic patients. Once the composite restoration is completed, a single instrument composite polishing system will be used to complete the procedure.
Incipient Lesions in Enamel Only
The Fissurotomy procedure (Fissurotomy®, SS White, Inc., www.sswhiteburs.com) allows the dentist to conservatively widen the primary grooves of a posterior tooth using specialized carbide burs designed to keep the preparation size to an absolute minimum, while creating ideal shape and form using divergent walls and rounded internal line angles to reduce the risk of fracturing for the composite to be placed. After caries removal, the preparation is restored using flowable composite material. In many cases, the preparation can be confined to only the affected area of the tooth. Therefore, “extension for prevention” is not required; only the diseased tooth structure and minimal surrounding hard tissue are removed, and the majority of surrounding healthy tooth structure is preserved. Because the composite resin micromechanically bonds to the underlying dentin and enamel, an insoluble seal of the margin is achieved. The chances of future microleakage and recurrent decay are greatly reduced using this minimally invasive approach, and the integrity of the tooth is preserved.
Caries Beyond the DEJ
After a carious lesion penetrates the DEJ, it will spread laterally and pulpally at a faster rate because of the softer nature of the dentin substrate as compared to harder enamel. Also, because of the presence of dentinal tubuli that are fluid-filled and communicate directly with the C-fiber nerve endings in the dental pulp, rotary excavation of carious dentin with conventional carbide burs has a propensity to cause discomfort to the patient unless local anesthesia is used.
The “Comfortable Cavity Prep” System
The Comfortable Cavity Prep System is a kit of “task specific” rotary instruments by SS White designed to give the dentist both a conservative way to access carious lesions in tooth structure and a way to remove carious dentin only, leaving behind structurally healthy dentin substrate. Access into enamel does not elicit a pain response because there is no nervous innervation of this tissue. The diminutive tip of the Fissurotomy bur allows for pinpoint access through the enamel to the carious lesion with little to no removal of healthy tooth structure. Once the DEJ is penetrated, SmartBur II, a polymer bur designed to discriminate between healthy and carious dentin and remove only decayed tooth structure, is used. According to the manufacturer, some of the other clinical benefits of SmartBur II include: 1. There is no trauma to the dentinal tubules, thereby in many cases, reducing, or eliminating the pain response and decreasing the need for local anesthetic; 2. The minimally invasive nature of the polymer-cutting instrument reduces the risk of pulp exposures when excavating deep carious lesions; and 3. Carious excavation using SmartBur II leaves a greater amount of healthy tooth structure remaining after preparation to help support and retain restorative materials.
A major clinical benefit of this system is the systematic approach to conservative cavity preparation that the unique instrumentation provides the dentist.
Clinical Case: Deep Carious Lesion
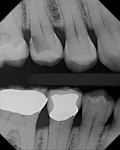
A patient presented with a rather extensive radiographic carious lesion on the distal aspect of tooth No. 4 (Figure 1). Clearly visible was the carious penetration below the proximal contact area into the distal surface of the tooth, with the larger apex of the “triangle” at the surface narrowing to a pinpoint as the lesion followed the enamel rods toward the DEJ. The caries then spread laterally along the DEJ and pulpally toward the center of the tooth. Another area of caries penetration was seen in the central groove of the occlusal surface as a “small, pinpoint” area that would either “stick” or not “stick” with an explorer tip (Figure 2). The carious penetration in the central groove was “opened up” using a Fissurotomy bur (Figure 3) to gain conservative access to the active lesion below (Figure 4). As the lesion was opened up, it was noted that the caries had spread in the buccolingual direction as well. A diode laser was used to remove the interproximal tissue and gain better access to the gingival margin of the cavity for matrix placement. Once the convenience and access forms of the cavity were completed, the excavation of the carious lesion with SmartBur II could begin (Figure 5). The appropriate size diameter SmartBur II was chosen, and the excavation was completed with slow-speed instrumentation. The major advantage of using the polymer bur is that it can easily remove decayed dentin but it cannot cut healthy dentin, which is always removed when using round carbide burs for this procedure. Because of the close proximity to the dental pulp, a bioactive cavity liner was placed on the cavity floor (Figure 6). Once the liner was light-cured, a self-etching dentin bonding resin was applied to the enamel and dentin per manufacturer’s instructions and light-cured. Next, the first increment of composite material was placed into the cavity preparation and light-cured. This increment filled the proximal box and pulpal floor of the cavity to a point just apical to the proximal contact area (Figure 7). The final increments were then placed, light-cured, and finished. Figure 8 shows the completed composite restoration on tooth No. 4 after instrumentation with the Comfortable Cavity Prep System.
A Simplified, Systematic Approach to Finishing
Once a composite restoration is placed, it must be trimmed/finished and polished so that the surface is smooth like natural tooth structure and the margins of the tooth/restoration are confluent and imperceptible to the tine of an explorer. Many composite finishing systems require two or three successive diamond or carbide instruments to refine or prepare the composite surface for the final luster, which is placed with rubber abrasives.
Trimming and finishing burs (SS White) are manufactured in both 12- and 20-blade configurations. These posterior composite burs are designed for two-step contouring and pre-polishing all posterior composite restorations. The 12-blade burs are engineered to finish and contour composite restorations directly after placement. Anatomical features such as grooves, pits, and fissures can be easily placed into the composite restoration with this set of finishing burs. They create a seamless transition from composite to natural tooth at the margins of the restoration. The 20-blade configuration is used to pre-polish the surface of the composite by removing any striations or scratches and blending the cavosurface margin to a natural seamless form. These burs are non-invasive and create an ultra-smooth surface on all composite materials, which is ideal for final polishing. These burs are used in a high-speed handpiece with water spray to optimize the finished surface.
Once the trimming/finishing step is completed, the occlusal contacts on the restoration are checked with articulating paper and are further adjusted with the appropriate 20-blade trimming/finishing bur as needed. Once the occlusion has been properly adjusted, the final luster or polish can be imparted to the restoration. Again, for many polishing systems, two or three grits of rubber abrasives are required to finish the process and end with a high luster on the surface of the restoration. Jazz® Supreme Single Step Composite Polishers (SS White) are designed to use low speed and low pressure with water to create a beautiful luster on the surface of composite restorations. The water creates a slurry with the diamond particles and the silicone in the polisher to impart a high surface gloss on the composite material. According to the manufacturer, some of the benefits of the Jazz Supreme system are: (1.) The combined technology of diamond particles and silicone impregnated in the rubber abrasive help create the highest possible surface luster; (2.) A single-step system saves the operator time and helps create an optimal shine much faster; (3.) The shanks of the instruments are made of stainless steel and are surface refined witsh gold flashing, making these instruments ideal for multiple use; and (4.) The Jazz Supreme Polishers are compatible with all esthetic composite materials, eliminating the need for multiple polishing systems.
Disclosure
Dr. Lowe has received honoraria from SS White.
About the Author
Robert A. Lowe, DDS
Private Practice
Charlotte, North Carolina