Using a Laser Fluorescence Device for Caries Diagnosis
Are clinicians seeing the “total picture” of patients’ caries status?
Technology has moved dentistry into an exciting time. Practices all over the country are fabricating crowns using laser scanning and computer design. Lasers are being used to control inflammation and pain in the mouth and to help stabilize chronic periodontal infections. New materials, tools, and equipment have made restorative dentistry more efficient, esthetic, minimally invasive, and enjoyable to practice.
However, on the diagnostic side of the equation, the profession as a whole has lacked the forward thinking that the restorative side has enjoyed. Unlike periodontal disease, which is experiencing a renaissance in diagnostics with bacterial testing and the use of high magnification, caries diagnosis has remained visual and tactile, and therefore highly subjective. Caries management is the dental professional’s most important duty.1
The scientific literature is clear that cutting cavity preparations in teeth of a certain width and depth weaken the tooth.2 Thus, it is imperative that catching decay early and sealing the teeth to prevent future acid attack is vital to preserving the vitality and biomechanical properties of sound tooth structure. Early and accurate detection of decay is essential to achieving this goal.3 Traditional methods of caries detection are well entrenched in dental school curriculums. Explorers, visual inspection, and radiographs are the main methods for assessing the potential caries in a tooth.
The use of the explorer as the primary diagnostic tool for caries diagnosis is as reflexive as the periodontal probe. However, the use of an explorer for caries detection is neither objective nor accurate. Studies have shown 30% to 50% effectiveness for even the sharpest of explorers.4
Visual inspection of the tooth is an integral part of traditional caries diagnosis. It is clear, however, that the criteria for visual inspection is not consistent throughout the profession and it relies heavily on the lighting, magnification, and the subjective judgment of the clinician.
The International Caries Assessment and Detection System was created to standardize the diagnosis and treatment of dental decay. Unfortunately, while the developers should be applauded for their intentions, their decision tree is not easily followed and integrated into private practices.
Because of fluoridation and improvements in oral home care, some of the criteria that have been used for the longest time no longer apply. It is rare to see softened enamel around a stained fissure, and with the advent of remineralization dentifrices and rinses, even decalcification is harder and harder to detect.5 It is well understood that radiographs are no better in diagnosing occlusal caries.6 The biggest problem, then, is the issue of “subclinical” decay.
Caries expression is not always cavitated or severely decalcified in the enamel. The base of a pit or fissure, which is usually the most susceptible to acid attack, often exhibits caries without any visual occlusal evidence other than stain. This subclinical caries is often seen as innocuous pits and fissures in which, when the dentinoenamel junction (DEJ) is exposed, the acid attack is far worse than expected (Figure 1, Figure 2 and Figure 3). Clinicians relying on the traditional method of caries detection see these stained fissures and either re-evaluate at the following recall or ignore them altogether (Figure 4).
As important in caries diagnosis is patient education. Patients are routinely surprised when their dentist “finds” one or multiple “cavities.” Often the response is one of shock because they have no symptoms. Caries can progress even into the pulp chamber without any symptoms. However, patients incorrectly believe that pain is always associated with dental caries.7
That surprise can often turn to distrust, when the practitioner finds multiple caries in a patient that has no caries history or no dental complaints. Patients will leave one office and go to another for a second opinion and that dentist finds much less or none at all. Often that dentist will discredit the first practitioner, accusing him or her of overtreatment or insincere motives. This can lead to the patient not doing anything and forgoing treatment altogether because they hold dentistry in such low regard.
It has been nearly 300 years since the dental explorer was introduced. Certainly, there must be more modern methods of caries detection that deal with the deficiencies of traditional caries diagnosis.
Laser Fluorescence as an Adjunctive Diagnostic Aid
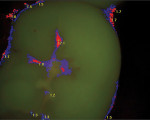
With the application of laser energy of a specific wavelength, bacterial byproducts called porphyrins will fluoresce red. The intensity of the fluorescence can then be measured as a direct correlation to the occurrence and magnitude of the caries activity. Thus, the more acid attack the tooth undergoes, the higher the number on the scale of the capture device.
The Spectra Caries Detection Device (Air Techniques, airtechniques.com) has dealt with many of the stated issues with early laser fluorescence devices and made a device that is portable, efficient, and provides significant patient impact and excellent documentation of the tooth’s caries status. It consists of a wand that seamlessly integrates with most digital imaging software via a TWAIN interface. This “plug-and-play” property allows the operator to quickly disconnect the unit from one computer and connect it to another operatory computer.
The color pattern reminds practitioners of weather patterns on radar that one would see on the evening news. This “Doppler” effect provides the patient and the practitioner a visual aid that frames dental decay in familiar terms. The dentist can then show the patient the tooth and, immediately, the patient can understand what is going on, why it is going on, and discussions of possible treatment plans can proceed. Patients rarely question the results because it is an objective test; the doctor’s thoughts and biases are taken out of the equation (Figure 5, Figure 6 and Figure 7).
Conclusion
The Spectra brings caries detection closer to being a more objective diagnostic science. More decay is diagnosed and less tooth structure is lost as a result of the progression of an infection that can be easily halted. Patients no longer question the dentist’s motivation in wanting to “find work” to do on them as the diagnosis is taken out of the dentist’s hands and into a framework that the patient can understand and appreciate.
References
1. Fusayama T. A Pain-Free Adhesive Restorative System by Minimal Reduction and Total Etching. Tokyo: Ishiyaku EuroAmerica, Inc: 1993:2.
2. Larson TD, Douglas WH, Geistfeld RE. Effect of prepared cavities on the strength of teeth. Oper Dent. 1981;6(1):2-5.
3. Milicich G, Rainey JT. Clinical presentations of stress distribution in teeth and the significance in operative dentistry. Prac Periodont Aesthet Dent. 2000;12(7):695-700.
4. Loesche WJ, Svanberg ML, Pape HR. Intra-oral transmission of mutans streptococcus by a dental explorer. J Dent Res. 1979;58(8):1765-1770.
5. Hamilton JC. Should a dental explorer be used to probe suspected carious lesions? J Am Dent Assoc. 2005;136(11):1526-1530.
6. Eds Fejerskov O, Kidd E, eds. Dental Caries. The Disease and its Clinical Management. 2nd ed. Oxford: Blackwell Munksgaard; 2008.
7. Christensen R. Air abrasion caries removal, 5 year status report. Clinical Research Associates Newsletter. 1999;23(12):2-3.
About the Author
Howard Golan, DDS
Private Practice
New Hyde Park, New York