A Primer on Intraoral Direct Digital Radiography Part I: Advantages and Disadvantages
Since the discovery of penetrating radiation by Roentgen in 1895, film-based imaging has been the predominant radiographic technology used in dentistry. The roots of modern computed radiography date back to 1975, when George Luckey developed the flexible storage phosphor plate.1 Direct digital radiography (DDR), a later development invented and championed by Dr. Frances Mouyen,2 has been gaining acceptance among dental and medical practitioners since it was first introduced in France in the mid-1980s. Photostimulable phosphor plates (PSP) and indirect digital radiography (secondary capture of conventional film by scanning) are two other forms of digital radiographic imaging available to practitioners.3,4 However, because of the workflow benefits associated with DDR, PSP and scanned conventional films are less useful technologies than direct digital detectors for endodontic, oral surgical, and implant procedures.
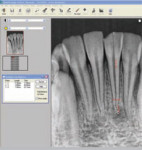
Advances in computer reliability, data storage, and image resolution have made DDR one of the most important advancements in healthcare (Figure 1). Despite DDR's advantages, many dental practitioners are reluctant to purchase these systems because of concerns about the transition from film-based imaging to DDR, and the notion that an office must be either completely digital or analog. For these practitioners, Farman and Scarfe suggest that adding digital radiography to a film-based system may be appropriate.5
The promise of digital imaging is aiding the practitioner in making better diagnostic decisions.6 Caries-detection software is a recently developed digital diagnostic tool that measures pixel brightness values and compares images to expected patterns. It is but one example of software that assists in the identification of difficult-to-detect early dental disease. While these software algorithms are fairly new, future developments in measuring bony changes, searching for periapical pathosis, automatic orthodontic measurements, and more hold great potential.7 What follows is a primer on the advantages and disadvantages of DDR. Part II of this article will review system components.
Advantages of Direct Digital Radiography
The value of digital radiography in dental and medical diagnosis is well known, especially during operative procedures where time-to-image is important. Key advantages of digital radiography are: reduction in radiation dose to the patient; patient education; image optimization and computer-aided feature extraction;8 workflow improvement; the avoidance of shipping, darkroom, or chemical processing errors; environmental waste reduction; improved electronic communications;9 image archiving; and projecting a technologically advanced practice image.
Reduction in Radiation Dose
Silver-halide film records the interaction of X-ray photons with electrons in the film emulsion. The photons are either attenuated (absorbed or scattered) or transmitted (along with some scatter), and reach the film emulsion to create a latent image. This image is then chemically processed to reveal the viewable radiograph.
Film images are characterized by continuous shades of gray between the extremes of black and white.10 However, film requires a relatively high dose of x-radiation to achieve the same result as a direct digital detector. According to van der Stelt, "the primary principles of radiation protection in diagnostic radiology are justification (the patient will experience more benefit than harm from the exposure) and the ‘as low as reasonably achievable' (ALARA) principle…"11 Despite the fact that radiation exposure can be reduced by using thyroid shields, the highest-speed films, and rectangular collimation, studies consistently demonstrate that radiation hygiene is not practiced by dentists to its fullest benefit. To this end, new guidelines issued in 2003 by the National Council on Radiation Protection (NCRP) in its Report No. 145 supersedes the previous report published in 1970.12
Many of the NCRP recommendations in the report (Table 1) are contrary to current common radiography practices in dentistry; if the states adopt the newest NCRP recommendations, as is commonly done, most dental offices would not be in compliance. Two terms used in the report have been specifically defined. The terms shall or shall not indicate that adherence to the recommendation would be in compliance to the standards of radiation safety. The terms should or should not indicate prudent practice and acknowledge that exceptions may be made in certain circumstances.
Although common dental projections rarely, if ever, deliver a measurable absorbed dose to the embryo or fetus, any radiologic procedure on a pregnant patient should be conducted so as to minimize the radiation dose to the pelvic region. This procedure should be conducted only if x-ray exposure is required for adequate diagnosis and treatment. If dental care is to be delayed until after delivery, then exposure should also be delayed. Also, usual and customary radiographic selection criteria should be applied for patients who are trying to get pregnant or are breast feeding or have received radiation therapy to the head and neck for medical purposes (the radiation dose from dental radiography is insignificant when compared to therapeutic dosing).13,14
In addition, there are also nine new recommendations for image processing of conventional film in the NCRP report. A strong argument can be made for dental practitioners to switch to a direct digital radiography system to avoid all the drastic changes necessary to be in compliance with the new recommendations.
Digital intraoral imaging generally requires less radiation than film-based systems, a key public health benefit. According to the ADA Council on Scientific Affairs, digital imaging reduces radiation exposure by 50% to 90% (Table 2).15 Film scanning provides no reduction in radiation, because a conventional film image must first be produced.
Although digital radiography promises to reduce radiation for each image exposure, the real radiation that a patient receives in relation to the diagnostic information gained remains controversial. In studies by Versteeg et al, and Sommers, technique errors for digital detectors were higher than film-based systems.16,17 The most common difficulty, according to focus group studies, was found to be sensor positioning. These studies dramatically point out the need for careful and ongoing training of dental technicians in the art of taking radiographs with digital sensors, which is critical to take full advantage of the benefits of reduced radiation for each image exposed.
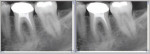
Placement errors aside, most CCD and CMOS-APS detectors have a similar range or exposure latitude to counteract under- or overexposure. Direct digital detectors take about 100 times more exposure to produce a black image than a light gray image, or a 100 to 1 ratio (Figure 2). In comparison, film has about a 1,000 to 1 ratio and PSPs have a range of 10,000 to 1.9 While the benefit of PSPs' wider range of exposure latitude may "save" an occasional over-exposed image, PSPs can lead to inadvertent excessive radiation exposure because over-exposure will less likely produce poor image quality as a warning.18 Strict adherence to preset exposure settings will continue to require diligence to reduce radiation exposure. Additional reduction in radiation to special needs patients (eg, patients with developmental disabilities or are severely mentally handicapped) may also be realized because of the advantages of digital detectors.19
Patient Education
Most people of college age and older are visual learners, and presentations that include both visual and auditory modalities are superior to visual or auditory modalities alone.20 Consider the educational value for the patient able to view a large, high-resolution radiograph in conjunction with the practitioner's diagnostic explanation. Once the patient understands their dental condition (eg, caries, periradicular pathosis), treatment acceptance becomes more assured.
Image Optimization and Computer-Aided Feature Extraction
The software bundled with most of the direct sensors will allow basic image optimization (Figure 3). Post-exposure image processing routines differ between manufacturers; where some produce a raw image in which automatic enhancement routines can be turned on and off, others produce images that are filtered automatically. Most software features the ability to adjust contrast, brightness, and perform gamma corrections and measurement functions. Creating an inverse image, density equalization, magnification, and image rotation are other fairly standard imaging tools. In a study by Hayakawa et al, the effects of equalization on image contrast and signal-to-noise ratio were evaluated using CDR (Schick Technologies Inc, Long Island City, NY) sensors.21 They found that the equalize function was an efficient method to increase contrast in underexposed images without adverse consequences to the signal-to-noise ratio. This tool does not compensate for overexposure, however, reducing the chances for overexposing the patient to ionizing radiation. Another enhancement, pseudo coloring, ascribes false colors based on the brightness of pixels and can help with patient visualization of images.22 Algorithms that can sharpen and enhance caries are also present in a number of systems, holding promise for even more future improvements.
Filtering Tools: Available in all commercial digital radiographic software, filtering tools help to measure area, mean, centroid, perimeter, etc; however, comparison between products is difficult because proprietary names do not reveal the underlying algorithms. Lehmann et al studied the functionality of 13 software programs and suggested more standardization of filtering tools to improve "exchange, enhancement, processing and analysis."23 He further suggested that public domain image processing and analysis software, like Scion Image (Scion Corporation, Frederick, MD), or similar software like that adopted for medicine by the National Institutes of Health, may provide the basis for more standardization.
Edge enhancement tools find areas where there is a change in contrast greater than the software manufacturer's preset gray levels, and enhances the contrast between those pixels and the pixels around them. In other words, these tools enhance the edges to add crispness to the image.
Measurement: The three types of measurement generally available with digital imaging software are linear measurement"the distance between two points in millimeters (Figure 4); angle measurement"the angle between two lines; and area measurement"the area of the image or a segment of the image. Because magnification caused by projective distortion plays a significant role in all radiographic measurement accuracy, both film and digital systems are subject to error. However, a study by Eikenberg and Vandre comparing endodontic file-length images of human skulls taken with a custom jig suggested that "measurement error was significantly less for the digital images than the film-based images."24 The authors point out that in clinical situations, these measurement differences may not be clinically significant. Sophisticated calibration algorithms are under development, so accurate measurement of parallel images should be more feasible in the future.25
Digital Subtraction Radiography (DSR): The pixel values of two images of the same region, taken at different times, can be compared by subtracting the first image from the second and assessing the differences. Of course, careful alignment of the detector and beam are necessary to achieve the best results. In a recent study, Carvalho et al evaluated healing of chronic periapical lesions before and after endodontic treatment at 0, 2, 4, and 6 months using Adobe® Photoshop® CS (Adobe, San Jose, CA). The resulting DSR images clearly demonstrated that healing could be successfully evaluated using this methodology.26 New software is being developed to correct density and contrast, and modify the image geometry of a second image to match the first, obviating the need for bite blocks.27,28 DSR is more sensitive to early bone loss than film-based systems, and will probably see continued development in caries diagnosis.29
Workflow Improvement: A Work Multiplier
According to Diehl, digital radiography is one of the most beneficial advances of automation in dentistry (personal communication). Digital radiography is a work multiplier; it replaces human effort, making tasks the practitioner and staff members perform easier, more error-free, and in some cases, making new tasks possible.30 DDR images take less time to expose, duplicate, retake, and transmit, all with less radiation and environmental impact. With solid-state systems, any operative procedure, such as endodontic therapy and implant placement, can be performed in less time. Furthermore, the diagnostic yield of digital imaging systems will improve as enhancements are made to image acquisition, but also to our understanding of human vision and cognition. Image processing can improve diagnostic outcomes by defining diagnostic issues and designing tools to achieve specific goals.31 Also, visual information, such as digital radiography and visible light images (ie, intraoral photography, microscopy), is easier to access than film-based images, and improve office operations by increasing efficiency.
PSP plates take at least 8 seconds to process after the film is transported to the developing site and unwrapped, whereas CCD/CMOS-APS detectors are virtually instant, with "paint times" usually just a few seconds. Some workflow advantages are shown in the following comparisons.32
Endodontic treatment: With PSP or film, if the apex is not visualized on the initial radiograph, at least 30 seconds will be required to travel to the scanner or developer, unwrap, process, and view the initial image. A second image will require the same setup as the first image, with no assurance of improvement. Using a solid-state detector, the operator can just reposition the detector and/or reposition the tube-head to get a second image, all in less than 20 seconds. Improved reliability of the retake DDR image is also an important way to reduce radiation.
Film duplication: Duplicating a film-based image requires a dark box or dark room, a light source, and developing. Of course, each iteration of the duplicate image will suffer from reduced resolution because analog images are not reproducible without degradation. In contrast, solid-state detectors allow almost instant retrieval of any image, and after a few mouse clicks, an identical image can be e-mailed and/or placed on magnetic or optical media, with no loss of image quality.
Avoidance of Shipping, Darkroom, or Chemical-Processing Errors
Most film-based imaging systems can suffer from exposure, processing, or film handling errors. Exposure errors may include double exposures, backward-placed film, film distortion, solutions over- and under-heated, light leaks, wet or tacky films, solution contamination, streaking, black bend marks, radiation fogging, film deterioration resulting from heat in transit or storage, static electricity, and torn emulsion.33 For example, Nvsether and Hansen found that 7.7% of film-based images were rendered inadequate simply by insufficient washing.34 Another significant benefit of DDR is the elimination of infectious agent transmission via film packets to office staff or other patients.
Environmental Waste Reduction
Digital radiography eliminates the need for a darkroom and its attendant space requirements, along with the cost of stocking film and chemicals. A survey sponsored by the US Environmental Protection Agency, the California Dental Association, and others found that the average number of exposures was 70 for each dentist per week.35 About 3% were spoiled exposures and 0.5 ounce of developer and fixer was used on average for each exposure, significantly more than the 0.1 ounce per image recommended by many film processor vendors. The hazardous chemicals in developer and fixer are noted in Table 3.
Analog film users must continue to purchase consumables"film and chemicals"and maintain sophisticated processors that generate waste byproducts in the form of silver and other chemical emissions. According to the Hawaii Pollution Prevention (P2) in Action newsletter, "Photo x-ray processing uses various chemicals and generates waste fixer containing silver that must be managed as hazardous waste or the silver reclaimed and recycled properly."36 The newsletter states that film packets generate lead waste and film processors use large amounts of water, creating further environment impact. X-ray developer and fixer contain hazardous chemicals which must not be poured into the sewer system.
Improved Electronic Communications
The advent of the Internet and computerized systems for the display and transmission of radiographic images has trans-formed medical and dental communications in ways that we could only dream of a few years ago. Radiologists can now remotely review CT, MRI, and other image formats via broadband connections with proprietary software that are allowing evaluations of radiographic images at any time, anywhere in the world, within a matter of minutes. HIPAA (Health Insurance Portability and Accountability Act) compliant offices can e-mail radiographs and protected health information to co-therapists for further consultation, if these entities satisfy the requirements of the HIPAA Security and state regulations. These improved electronic communications benefit patients by enhancing the transmission of radiographic and other materials, speeding decision making and avoiding duplication of diagnostic procedures, as well as increasing patient education options.
In dentistry, the interchange of diagnostic information between practitioners has been greatly improved by the industry's adoption of the Digital Imaging and Communication in Medicine (DICOM), standard. When JPEG images are sent between offices, a lot of the image data is lost, because the original JPEG standard uses a lossy compression codec. DICOM, on the other hand, supports the full exchange of original images along with patient demographics and anatomic information (eg, left or right side).
Image Archiving
Film-based images are prone to loss, and once the original film(s) are misplaced, scratched, undergo fixer degradation, or are otherwise damaged, there is no backup unless a duplicate film has been made. Although film-based images can easily be duplicated, each subsequent rendition of the image will be reduced in quality. Digital images, which are sensor-independent, can be reproduced in unlimited quantity because the data can be stored and reproduced without loss of any detail. Furthermore, digital images can be stored both on and off-site, and on many types of media, thereby helping to mitigate loss from theft, fire, or other causes.
All computer-based images are voracious consumers of hard drive space, and manufacturers have used a number of techniques to reduce image size. For example, Schick Technologies allows acquisition of each image with the advanced compression technology of the lossless mode of the JPEG 2000 codec. Practitioners can also compress selected groups of images between certain dates with up to four different compression schemes, allowing for lossless (no visible change in image clarity with approximately 50% reduction in file size) to lossy (significant reduction in file size with some degradation of image resolution) compression. Lossy compression is not recommended for dental grayscale images, and once the original images are compressed, they cannot be restored.
Occasionally radiographs need a tag so that the practitioner can return to them later to assemble teaching or patient education materials. Most software today allows markers to be placed so that a computer search can call up the images efficiently. These customized tags can be useful in organizing cases that require special follow-up to evaluate postoperative healing. In addition, most imaging software enables the practitioner to create notes and diagrammatic annotation of important image features (Figure 5).
Paradoxically, the ease of reproduction of digital images allows for the alteration of radiographs without a trace.37 Of course, this has also always been possible with duplicated analog film images, but the issue has not been commonly addressed. The ease of producing an altered image is controversial, but most digital vendors have created safeguards that greatly minimize the possibility of this occurring. Archiving radiographic images in a secure site in DICOM format using removable media such as optical disc storage media format, tape, or Internet backup is one of the current solutions to this issue. Magnetic or optical media can be stored off-site by a third-party archivist for extra protection and legal proof of image integrity.
Another important security consideration is the database engine that is used to store the files on the practice's server. Among the most robust systems are SQL-based models which allow for client-server configuration with industry standard software protocols. Images that are stored and retrieved cannot be deleted, or patient identification changed, without opening a separate administration utility that logs changes. Schick Technologies, Inc, for example, places a small letter symbol on any image that has been exported or imported (Figure 6), but always maintains the original image for retrieval. Ultimately, images can be analyzed by experts for image characteristics that will reveal alteration.
Projecting a Technologically Advanced Practice Image
One of the best ways to establish market leadership is to use state-of-the-art-technology to create value that patients can see and understand. Every patient treatment communication should reflect your technological competence. Digital radiographs and photographic images along with cogent narratives of treatment will reflect your commitment to the latest technology and help to operationalize your brand. Performing a state-of-the-art procedure and then communicating the results by sending a film-based image and a few handwritten notes misses the opportunity to maximize your image as technologically sophisticated. Research continues to link business success and professional achievement with developing long-term appeal and credibility. Adopting proven technologies is one of the most visible and reliable ways to create a positive impression with patients, referrers, and staff.
Disadvantages of Direct Digital Radiography
The main disadvantages of direct digital radiography are the thickness and rigidity of the digital detector, infection control, hardware and software maintenance, and the higher initial cost of the system. While increased placement errors have been documented by several studies discussed earlier,16,17 most placement errors can be significantly reduced by training and familiarity with the system.
Infection control is another area that requires special care, because dental dam clamps and positioning devices can cause tears in the plastic barriers, resulting in contamination of the sensor and/or its wire, if any. Some manufacturers (Planmeca USA, Roselle, IL) are producing hermetically sealed and fully submersible sensors that offer improved disinfection. No sensors are available today that allow heat or autoclave sterilization.
Today, hardware and software are reasonably stable and require infrequent maintenance. Many manufacturers now offer online software updates that keep pace with changing operating systems and customer replaceable cable-to-sensor connections that improve in-office serviceability (Schick Technologies).
DDR systems require a large initial investment to acquire sensors, software, and up-to-date computer workstations and monitors. All manufacturers, however, can show that new systems will eventually yield a positive return on investment owing to workflow efficiencies, elimination of darkroom supplies and developer purchases, and floor-space rental costs.
Conclusion
Patients expect a high-tech approach to treatment. In fact, the National Health Information Infrastructure (NHII), a federally sponsored, voluntary national electronic information network for healthcare, proposes to implement a set of technologies, standards, applications, and laws that support interoperable computer-based patient records for most Americans by 2014.38 How will your practice measure up? With the expanding use of technology in every aspect of life, patients expect their healthcare encounters to include the newest technologies. There are many ways an office can project a technologically advanced practice image. Examples include: use of the Internet for patient intake; receipt of pre-treatment radiographs and information; digital radiography; electronic medical record (EMR); microscopes with imaging capability; instant communication of treatment reports by e-mail; online pharmacology information at chairside; and music and entertainment options during treatment. The list goes on and on, but the importance of differentiating your practice cannot be overestimated.
References
1. Mango SA. Transitioning to digital radiography"How NDE organizations are making sense of new technology. Brit J Nondestr Test. 48(1):52-53.
2. Mouyen M, Benz C, Sonnabend E, et al. Presentations and physical evaluation of RadioVisioGraphy. Oral Surg Oral Med Oral Pathol. 1989;68(2):238-242.
3. Vandre RH, Webber RL. Future trends in dental radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80(4):471-478.
4. Farman AG. Fundamentals of image acquisition and processing in the digital era. Orthod Craniofac Res. 2003;6(suppl 1):17-22.
5. Farman Ag, Scarfe, WC. Digital dental radiography is not an "all or nothing" decision. Contemp Esthet Restor Pract. 2006;10(3):12-15.
6. White SC, Yoon DC, Tetradis S. Digital radiography in dentistry: What it should do for you. J Calif Dent Assoc. 1999;27:942-952.
7. Gakenheimer DC. The efficacy of a computerized caries detector in intraoral digital radiography. J Am Dent Assoc. 2002;133(7):883-890.
8. Van der Stelt PF. Principles of digital imaging. Dent Clin North Am. 2000;44(2):237-248.
9. Versteeg CH, Sanderink GC, van der Stelt PF: Efficacy of digital intra-oral radiography in clinical dentistry. J Dent. 1997;25(3-4): 215-224.
10. Razmus TF. An overview of oral and maxillofacial imaging. In: Razmus TF, Williamson GF, eds. Current Oral and Maxillofacial Imaging. Philadelphia, PA: WB Saunders; 1996:6-7.
11. Van der Stelt. Filmless imaging: The uses of digital radiography in dental practice. J Am Dent Assoc. 2005;136(10):1379-1387.
12. National Council on Radiation Protection and Measurements (NCRP), Radiation protection in dentistry. Report #145, Bethesda, MD, 2003. Available at: www.ncrponline.org/Publications/145press.html. Accessed March 18, 2008.
13. Matteson SR, Joseph LP, Bottomley W, et al. The report of the panel to develop radiographic selection criteria for dental patients. Gen Dent. 1991;39: 264-270.
14. Gibbs SJ. ADA Council on Dental Materials, Instruments and Equipment: Biological effects of radiation from dental radiographs. J Am Dent Assoc. 1982;105:275-281.
15. ADA Council on Scientific Affairs. An update on radiographic practices: information and recommendations. J Am Dent Assoc. 2001;132:234-238.
16. Versteeg CH, Sanderink GC, van Ginkel FC, van der Stelt PF. An evaluation of periapical radiography with a charge-coupled device. Dentomaxillofac Radiol. 1998;27(2):97-101.
17. Sommers TM, Mauriello SM, Ludlow JB, et al. Pre-clinical performance comparing film and CCD-based systems. J Dent Hyg. 2002;76:26-33.
18. Berkhout WE, Beuger DA, Sanderink GC, van der Stelt PF. The dynamic range of digital radiographic systems: dose reduction or risk of overexposure? Dentomaxillofac Radiol. 2004;33(1): 1-5.
19. Farman AG, Horsley B, Warr E, et al. Outcomes of digital X-ray mini-panel examinations for patients having mental retardation and developmental disability. Dentomaxillofac Radiol. 2003;32(1):15-20.
20 Fleder RM, Silverman LK. Learning and teaching styles in engineering education. Engr Education. 1988;78(7):674-681.
21. Hayakawa Y, Farman AG, Scarfe WC, Kuroyanagi K. Processing to achieve high-contrast images with computed dental radiography. Dentomaxillofac Radiol. 1996;25(4):211-214.
22. Lehmann TM, Kaser A, Repges R. A simple parametric equation for pseudocoloring grey scale images keeping their original brightness progression. Image and Vision Computing. 1997;15:251.
23. Lehmann TM, Troeltsch E, Spitzer K. Image processing and enhancement provided by commercial dental software programs. Dentomaxillofac Radiol. 2002;31:264-272.
24. Eikenberg S, Vandre R. Comparison of digital dental x-ray systems with self-developing film and manual processing for endodontic file length comparison. J Endod. 2000;26(2): 65-67.
25. Burger CL, Mork TO, Hutter JW, Nicoll B: Direct digital radiography versus conventional radiography for estimation of canal length in curved canals. J Endod. 1999;25 (4): 260-263.
26. Carvalho FB, Gonçalves M, Tanomaru-Filho M. Evaluation of chronic periapical lesions by digital subtraction radiography by using Adobe Photoshop CS: A technical report. J Endod. 2007;33(4): 493-497.
27. Yoon DC. A new method for the automated alignment of dental radiographs for digital subtraction radiography. Dentomaxillofac Radiol. 2000;29(1):11-19.
28. Guneri P, Gogus S, Tugsel Z, Boyacioglu H. Efficacy of a new software in eliminating the angulation errors in digital subtraction radiography. Dentomaxillofac Radiol. 2007;36(8):484-489.
29. Nummikoski PV, Martinez TS, et al. Digital subtraction radiography in artificial recurrent caries detection. Dentomaxillofac Radiol. 1992;21(2): 59-64.
30. Levin, M. Digital imaging: A work multiplier. Endodontic Therapy. 2005;5(4):31.
31. Mol A: Image processing tools for dental applications. Dent Clin North Am. 2000;44(2):299-318.
32. Parks ET, Williamson,GF. Digital radiography: An overview. J Contemp Dent Prac. 2002;3(4):23-39.
33. National Electric Manufacturers Association (NEMA): PS 3.1-2004. Digital Imaging and Communications in Medicine (DICOM) Part 1: Introduction and overview. Available at: www.medical.nema.org/dicom/2004/04_01PU.PDF. Accessed February 15, 2008.
34. Nvsether S, Hansen, BF. Errors on dental bitewing radiographs. Community Dent Oral. 1983;11(5):286-288.
35. Western Regional Pollution Prevention Network. Reducing dental x-ray chemical use. Available at: www.wrppn.org/dental/pages/pdf/Photo_Fact_03-pc.pdf. Accessed February 15, 2008.
36. Pollution prevention (P2) in action. Dentistry. Hawaii State Department of Health. 2007;1(1):1-2.
37. Visser H, Kruger W: Can dentists recognize manipulated digital radiographs? Dentomaxillofac Radiol. 1997;26(1): 67-69.
38. The National Health Information Infrastructure. Available at: www.aspe.hhs.gov/sp/NHII/. Accessed January 12, 2008.