Esthetic Crown Lengthening: An Alternate Technique for Surgical Communication
Greggory A. Kinzer, DDS, MSD
Esthetically driven treatment planning relies heavily on the position of the teeth and the position and architecture of the soft tissue.1-4 Often, an interdisciplinary treatment approach is needed to address the different treatment parameters and provide the most esthetic outcome. Many different treatment options for altering gingival levels have been documented in the literature.5-11 Regardless of the treatment modality selected, the correct diagnosis is paramount to the overall success of the treatment. One of the most frequently used treatment options for altering gingival levels is clinical crown lengthening. Unless the clinician restoring the teeth is also providing the surgical treatment, communication between the restorative dentist and the surgeon is imperative with regard to defining the desired tooth position and corresponding free gingival margin locations. This is ultimately accomplished as part of the treatment planning process by taking into consideration things such as the maxillary incisal edge position, tooth proportion, probing depths, and biologic width. Communicating the specific tooth position and free gingival margin location to the surgeon can be done in several ways. A diagnostic model with the appropriate diagnostic lines that define the location of the desired free gingival margin can be sent to the surgeon for reference. Using the measurements from the reference model and transferring them to the mouth during surgery is an effective form of communication. Another method of transferring the desired gingival alteration is to fabricate and use a surgical overlay guide.12 The surgical overlay guide provides the surgeon with all of the necessary information on tooth position and effectively communicates the intended surgical and restorative outcome to the patient before the surgical procedure. One of the challenges with either of these two techniques is maintaining a high level of esthetics throughout the course of treatment. While the desired tissue levels can be adequately communicated, the patient generally must wait a significant amount of time after the surgery for tissue healing and maturation before initiating provisional restorative therapy. It is during this time that the recession created by the excisional gingivectomy and osseous surgery can lack an esthetically pleasing appearance.
For patients with a high smile, two treatment options exist for maintaining esthetics throughout the entire treatment. One option is to use one of the aforementioned techniques to transfer information to the surgeon and "phase" the surgery. The first phase is to complete the osseous surgery component, thereby placing the bone in the correct position with regard to the future intended free gingival margin. However, rather than simultaneously moving the gingival tissues, the flap is coronally re-positioned to its original location. Then after the appropriate healing time, a gingivectomy can be completed to re-position the gingival tissue without violating the biologic width. At this same appointment, subsequent to the repositioning of the gingival tissue, the teeth can be prepared and provisionalized.
The purpose of this article is to discuss an alternate technique for transferring information on the definitive tooth placement and free gingival margin location to the surgeon that ensures that the highest level of esthetics will be maintained throughout the entire course of treatment. The proposed technique involves the restorative dentist repositioning the gingival margins to the desired level via a gingivectomy irrespective of the biologic width.5 Immediately after the gingivectomy, the teeth are prepared to the level of the new gingival margin and provisional restorations are placed. Once the tissue has healed, the next step in the treatment process is bone-level repositioning by the surgeon. At this time a flap is reflected to allow for the re-contouring of the osseous crest using the gingival margins of the provisional restoration as a reference. The required re-positioning of the bone relative to the provisional margin re-creates adequate space for the re-establishment of the biologic width. Upon healing and maturation of the tissues after the ostectomy, the preparations can be modified, final impressions can be taken, and the definitive restorations can be seated.
One issue that needs to be addressed is the effect of temporarily violating the biologic width. The gingivectomy procedure used in this technique typically will remove the gingival crevice, junctional epithelium, and part or all of the connective tissue attachment. Wound healing begins with epithelial proliferation and the establishment of a junctional epithelium, followed by connective tissue proliferation and the development or repair of a supracrestal fiber attachment. Studies that have examined periodontal wound healing have shown that these events occur within a 2- to 4-week period.13,14 The placement of restorations within this zone of periodontal attachment will impede the formation of dento-gingival fiber formation. This impediment will elicit an inflammatory reaction as the process of wound repair progresses. However, in this situation, violation of the biologic width is temporarily tolerated without undue gingival inflammation as the periodontal complex initially reorganizes. To avoid the development of gingival marginal erythema, it is important to sequence the treatment so that osseous resective periodontal surgery will follow ~2 to 4 weeks after the first restorative phase.
How long after the resective osseous surgery must one wait before initiating the final restorative procedures? Although periodontal flap wound healing may be complete at 4 to 6 weeks, soft tissue margin stability may not be achieved within this time frame. Studies evaluating gingival margin position after clinical crown lengthening procedures have shown both the development of recession and marginal "rebound."15,16 Factors that have an affect on the gingival margin position and stability are the periodontal biotype, amount of ostectomy, and flap adaptation. Although postsurgical suturing of the mucoperiosteal flap above the osseous crest will allow for a more rapid development of the dentogingival complex, it is prudent to wait longer before final restorations are placed. Generally, a 3-month healing period is allowed after the resective osseous surgery before initiating the final restorative procedures.
This esthetic crown-lengthening technique affords many benefits. First, it places the control of positioning the gingival margins in the hands of the restorative dentist, while still allowing for any fine-tuning of the tissue levels by the surgeon at a later date. One caveat exists when applying this technique; an ample amount of gingival tissue must initially be present, such that 2 mm to 3 mm of keratinized tissue remains after the gingivectomy. Second, the overall esthetics of the teeth and smile are improved from the very first appointment. The patient does not have unesthetic root exposed at any time during the restorative treatment. Lastly, it is one of the most ideal ways to provide information to the surgeon. Not only has the gingival architecture previously been created, but the reference points for repositioning the osseous crest are present as well.
CASE STUDY
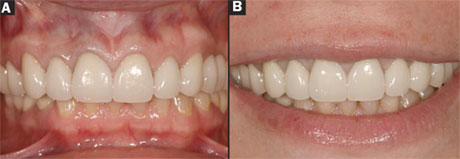
A 35-year-old woman was referred for comprehensive evaluation and treatment by her endodontist (Figure 1A and Figure 1B). Her dental history included a reconstruction of the upper arch with full-coverage splinted metal-ceramic restorations. The restorations were completed in Russia and ranged from 5 to 10 years old. Clinical evaluation revealed that all of the maxillary restorations from teeth Nos. 3 through 9 were failing as a result of significant marginal openings with subsequent microleakage and caries. In addition, numerous teeth on the maxillary arch had failing root canals that would require endodontic re-treatment. One of the patient's treatment goals was to improve the overall health and esthetics of her dentition. An examination was completed and the appropriate diagnostic information was gathered, including periodontal and occlusal evaluations. Study models were obtained and mounted with a facebow and centric relation bite records.
TREATMENT PLANNING
The treatment planning process was initiated by evaluating the current tooth position of the maxillary incisal and occlusal planes. One of the treatment objectives was to have a level occlusal plane at the completion of treatment. Because of the absence of teeth Nos. 30 and 31 and the severe occlusal wear on teeth Nos. 28 and 29, the current occlusal plane was hanging down on the upper right (Figure 2). To level the maxillary posterior occlusal plane, the right posterior crowns would need to be raised to match the position of the left posterior crowns. Raising the occlusal plane of the right side would have the added benefit of allowing enough interocclusal distance to restore the lower right posterior with two single-tooth implants in the Nos. 30 and 31 sites. Evaluation of the maxillary incisor display with the lips in repose revealed ~1.5 mm of central incisor display (Figure 3). Given what is known from the literature regarding tooth display at rest and the fact that the current flatness of the maxillary incisal edges on teeth Nos. 7 through 9 gave the patient a more "aged" appearance, it was decided that the incisal edges of teeth Nos. 8 and 9 would be lengthened.17
Once the position of the maxillary occlusal plane had been decided, the next area to be evaluated was the position of the free gingival margins. To evaluate the position of the soft tissues, the teeth were evaluated with regard to tooth proportion and symmetry. In the maxillary anterior, good tooth proportion was present on teeth Nos. 10 and 11; these teeth were used as a guide to help determine the desired gingival margin locations of the remaining anterior teeth. The goal was to achieve the classic "high-low-high" gingival margin symmetry of the canine, lateral, and central incisor. In the posterior, excessive gingival display was present on the upper right during a full smile as a result of a combination of lip asymmetry and the over-eruption of the upper right posterior teeth. The desired free gingival margin location in the posterior was relatively easy to determine given that the desired occlusal plane location had been determined and the corresponding tooth sizes from the upper left were present.
Once the position of the incisal/occlusal plane and free gingival margin locations were determined, the next question addressed was deciding the type of treatment to be used (Figure 4). The two treatment options that were discussed with the patient were orthodontics or osseous surgery. Given the root length, root taper, and the patient's desires, osseous surgery followed by restorative dentistry was chosen to establish the correct occlusal plane and free gingival margin locations.
TREATMENT
Before initiating any clinical treatment, a diagnostic wax-up was prepared. Given that the new free gingival margin location would be created at the time of initial tooth preparation and the placement of provisionals, the anticipated gingival surgery would need to be completed on the models before the diagnostic wax-up. A red pencil was first used to draw the desired free gingival margin locations on teeth Nos. 3 through 9 (Figure 5A ). This was done on two separate models, one to be used as a "go-by" when the excisional gingivectomies were performed clinically and one to be used for the diagnostic wax-up. A cleoid-discoid was used to remove the desired stone up to the red pencil line before completing the wax-up (Figure 5B ). Upon completion, the diagnostic wax-up was duplicated and a provisional "shell" was fabricated (Protemp™ 3 Garant™, 3M ESPE, St. Paul, MN).18
Clinically, the first step in the process following local anesthesia was to perform the excisional gingivectomies. Performing the gingivectomies before removing the existing restorations is recommended. This is done so that the restorations can be used as a part of the reference process. Using calipers, the diagnostic model with the red line that had not been waxed was used to transfer the desired location of the new free gingival margins to the mouth. Electrosurgery was used to perform the gingivectomies (Figure 6A ). Once the new free gingival margin location was created, the existing restorations were removed (Figure 6B ). Caries control was performed and the teeth were prepared up to the level of the newly created free gingival margin. Upon completion of the initial preparations the provisional shell was tried-in and relined. Once set, the provisional restoration was removed from the mouth, finished, and polished. The provisional was sectioned into three segments and tried back in the mouth to verify marginal fit, occlusion, and esthetics. After the appropriate changes it was cemented with temporary cement (Fynal®, Dentsply Caulk, Milford, DE) (Figure 7 ). A provisional check performed at 2 weeks (before re-establishing the proper biologic width with osseous surgery) revealed good gingival symmetry and the appearance of a healthy periodontal complex (Figure 8 ).
The patient was seen for osseous surgery ~16 days after the initial placement of the provisionals. To perform the required osseous surgery, a full-thickness flap is reflected while leaving the papillae (Figure 9A Figure 4). The patient's own biologic width was determined by "sounding" and "probing" adjacent teeth that did not have a gingivectomy performed. Using this information, osseous surgery was performed to re-establish the necessary room for the patient's biologic width (Figure 9B ). In the maxillary anterior (teeth Nos. 6 through 9), only facial bone was removed. In the maxillary posterior (teeth Nos. 3 through 5), the papillae were reflected and bone was removed circumferentially to allow for an increase in the preparation height needed for resistance and retention form. In addition to the osseous surgery performed in the maxillary arch, implants were placed in the Nos. 30 and 31 sites as well as crown lengthening on teeth Nos. 28 and 29.
During the 3 months allowed for implant integration, tissue healing, and maturation, the teeth that required endodontic re-treatment were addressed and subsequent foundation restorations were placed. Because of the lack of an opposing tooth, tooth No. 2 was left unrestored and only received plasty of the occlusal surface. The position of tooth No. 2 was to be maintained with the use of a full-coverage maxillary occlusal splint to be worn at night. The final impressions were taken and full-coverage metal-ceramic crowns were fabricated following the length, contour, and arrangement set forth by the provisional restorations. The definitive restorations were tried in and the fit, occlusion, and esthetics were evaluated and adjusted as necessary. The restorations were cemented with a resin-modified glass-ionomer cement (RelyX™ Luting Cement, 3M ESPE). The final result reveals a level occlusal plane with beautiful tissue symmetry and tooth proportion (Figure 10A and Figure 10B).
CONCLUSION
Predictable esthetic crown lengthening often requires an interdisciplinary treatment approach to address the different treatment parameters and provide the most esthetic outcome. Therefore, communication between the restorative dentist and the surgeon is essential. This article discussed an alternate treatment technique that is indicated for cases requiring crown lengthening in the esthetic zone. The proposed technique not only transfers the information on the definitive tooth position and free gingival margin location to the surgeon, but also affords the highest level of esthetics throughout the course of treatment.
References
1. Chiche GJ, Pinault A. Esthetics of Anterior Fixed Prosthodontics. Quintessence Publishing; 1994.2. Rufenache CR. Fundamentals of Esthetics. Quintessence Publishing; 1990.
3. Garber DA, Salama MA. The aesthetic smile: diagnosis and treatment. Periodontol 2000. 1996;11:18-28.
4. Spear FM, Kokich VG, Mathews DP. Interdisciplinary management of anterior dental esthetics. J Am Dent Assoc. 2006;137(2):160-169.
5. Lee EA. Aesthetic Crown Lengthening: Classification, biologic rationale and treatment planning considerations. Pract Proced Aesthet Dent. 2004;16(10):769-778.
6. Proffit WR. The soft tissue paradigm in orthodontic diagnosis and treatment planning: a new view for a new century. J Esthet Dent. 2000;12(1): 46-49.
7. Becker W, Ochsenbein C, Becker B. Crown lengthening: the periodontal-restorative connection. Compend Cont Educ Dent. 1998;19(3):239-254.
8. Allen EP. Surgical crown lengthening for function and esthetics. Dent Clin North Am.1993;37(2):163-179.
9. Kay HB. Esthetic considerations in the definitive periodontal prosthetic management of the maxillary anterior segment. Int J Periodont Rest Dent. 1982;2(3):44-59.
10. Rosenberg ES, Garber DA, Evain CI. Tooth lengthening procedures. Compendium. 1980;1(3):161-173.
11. Lowe RA. Clinical use of the Er,Cr:YSGG laser for osseous crown lengthening: redefining the standard of care. Pract Proced Aesthet Dent. 2006;18(4): S2-S9.
12. Spear FM. Construction and use of a surgical guide for anterior periodontal surgery. Contemporary Esthetics and Restorative Practice. 1999;4: 12-24.
13. Caffesse RG, Ramfjord SP, Nasjleti CE. Reverse bevel periodontal flaps in monkeys. J Periodontol. 1968;39(4): 219-235.
14. Engler WO, Ramfjord SP, Hiniker JJ. Healing following simple gingivectomy. A tritiated thymidine radioautographic study. I. Epithelialization. J Periodontol. 1966;37(4):298-308.
15. Brägger U, Lauchenauer D, Lang NP. Surgical lengthening of the clinical crown. J Clin Periodontol. 1992;19(1): 58-63.
16. Pontoriero R, Carnevale G. Surgical crown lengthening: a 12-month clinical wound healing study. J Periodontol. 2001;72(7):841-848.
17. Vig R, Brundo G. The kinetics of anterior tooth display. J Prosthet Dent. 1978;39:502-504.
18. Kinzer GA. The "eggshell" provisional technique. Advanced Esthetics and Interdisciplinary Dentistry. 2007;3(2): 26-31.
This article was reprinted from Advanced Esthetics and Interdisciplinary Dentistry. 2008;4(1):24-32.
 | ||
| Figure 1A and Figure 1B A 35-year-old woman presented with a complete maxillary reconstruction that had been seated 5 to 10 years previously. Multiple restorations were defective as a result of marginal microleakage, caries, and failing root canals. The patient?s treatment goals were to improve the overall health and esthetics of her dentition. | ||
 |  | |
| Figure 2 Esthetic evaluation revealed an uneven occlusal plane that was hanging down on the patient?s right side as a result of the absence of teeth Nos. 30 and 31 and the severe occlusal wear on teeth Nos. 28 and 29. Because of the compensatory eruption of the right side, significant gingival asymmetry was also present. | Figure 3 Evaluation of the maxillary incisor display with the lips at rest revealed ~1.5 mm of central incisor display. The ?flatness? of the maxillary incisal edges (teeth Nos. 7 through 10) gave the patient a more ?aged? appearance. Lengthening the incisal edges of the central incisors was planned. | |
 |  | |
| Figure 4 The esthetic treatment plan schematically drawn in blue over the patient?s smile projected lengthening the maxillary incisors and raising the posteriors on the upper right to help level the occlusal plane. To obtain gingival symmetry, the free gingival margins on teeth Nos. 3 through 9 needed to be moved apically. | Figure 5A Before the diagnostic wax-up, a red pencil was used to draw the desired free gingival margin locations on teeth Nos. 3 through 9. | |
 |  | |
| Figure 5B Model surgery was performed to apically move the free gingival margin location to the level of the red line. Once completed, a diagnostic wax-up was performed. | Figure 6A Before removing the current restorations, electrosurgery was used to perform the gingivectomies. A diagnostic model of the proposed gingival margin locations was used as a reference for the gingivectomies. | |
 |  | |
| Figure 6B Removal of the old restorations revealed marginal microleakage and cement washout. Caries control was performed and the teeth were re-prepared up to the level of the newly created free gingival margins. | Figure 7 The provisional restoration immediately after cementing the provisionals at the initial gingivectomy and preparing appointment revealed a level occlusal plane and gingival symmetry. | |
 |  | |
| Figure 8 A provisional check performed at 2 weeks revealed good gingival symmetry and the appearance of a healthy periodontal complex regardless of the biologic width impingement. At this point the patient was seen by the surgeon for the corrective osseous surgery. | Figure 9A To perform the required osseous surgery, a full-thickness flap was reflected leaving the papillae. Note the location of the provisional margin in relation to the osseous crest. (Note: these photos are from a different patient.) | |
 | ||
| Figure 9B Using the gingival margin location of the provisionals as a reference, osseous surgery was performed to re-establish the necessary room for the patient?s biologic width. | ||
 | ||
| Figure 10A and Figure 10B The definitive metal-ceramic restorations at a 2-year recall. The final result revealed a level occlusal plane with beautiful tissue symmetry and tooth proportion. | ||
| ABOUT THE AUTHOR | ||
 Greggory A. Kinzer, DDS, MSD Greggory A. Kinzer, DDS, MSDAffiliate Assistant Professor Department of Prosthodontics School of Dentistry University of Washington Seattle,Washington Private Practice Seattle, Washington | ||



