Fiber Post Selection and Placement Criteria: A Review
There has been an increased demand for endodontic therapy in the last several decades. When a tooth requires endodontic treatment, consideration must be given to the restorability of the tooth. If the tooth requires crown lengthening or orthodontic extrusion to expose adequate tooth structure for the fabrication of the definitive restoration, the selection of extraction and implant placement has to be considered. The patients’ health, comfort, and thoughts on treatment need consideration. The quantity and quality of the bone, the soft tissue architecture in the area and the condition of the remaining dentition need to be addressed.1,2 Crown lengthening or orthodontic extrusion may create an esthetic problem, as the diameter of the exposed tooth is less and an unfavorable crown-to-root ratio might occur. In a study by Torabinejad et al, implant-supported single crowns and root canal treatment and restorations provided similar outcomes and better long-term survival compared to fixed partial dentures.3 Once the decision is made to implement endodontic treatment, a decision needs to be made as to the final restoration and necessity for a post.
Previously, it was believed that a post was necessary after endodontic treatment to strengthen the remaining root structure weakened by the access to the canal and canal preparation. However, it is now felt that a post preparation and the post itself weaken the tooth further and make the root more susceptible to fracture.4,5 The decision to place a post should only be based on the need for retention of coronal structure.6
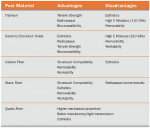
Once a post is deemed necessary for retention of the core, the type of post and appropriate luting material to achieve maximum longevity and support for the final restoration needs to be decided (Figure 1). Some authors have felt that the elastic modulus of fiber posts more closely resembles that of dentin compared to metal posts. This similarity may possibly result in greater stress reduction between the dentin and the post. This would result in less catastrophic failure such as root fracture.7 Cheung felt that by having the post and the dentin with similar physical properties bonded together, the post can strengthen and reinforce the root but still does not make the tooth stronger.8 The success of the endodontic treatment is predicated not only on good treatment but proper prosthetic reconstruction of the damaged tooth. Oral fluids and bacteria have to be prevented from gaining access to the periradicular areas by placement of adequate coronal restorations.8,9 The final treatment plan to create appropriate esthetics and function will help to determine the best post. It is imperative to determine if there is an ideal clinical situation for the variety of post systems currently available.10
Criteria for a post and determining its needs
Sedgley and Messer determined that vital dentin is harder than dentin from endodontically treated teeth but not enough to indicate that the teeth had become more brittle.11 Papa et al also felt there was not a major difference between vital and non-vital teeth as far as moisture content.12 The loss of tooth structure created by endodontic access (5% loss in structural stability) accompanied by a mesio-occluso-distal (MOD) cavity can result in an approximately 63% loss of stability.10 The indication for post placement depends on ascertaining the amount of destruction exhibited and whether the remaining tooth structure will support the selected restoration.13 The main factors that determine the prognosis of restored pulpless teeth have been the preservation of healthy dentin, the ferruling of crown margins on sound tooth structure, and the type of intermaxillary relation.14-17
Peroz et al described a classification of the amount of remaining tooth structure that depends on the amount of axial walls.9 Class I has all four axial walls remaining and only the access preparation involves removal of tooth structure. Class II has one cavity wall removed, which can consist of a mesio-occlusal or a disto-occlusal cavity. In Class III, a MOD cavity and two remaining cavity walls are present. Class IV has only one cavity wall remaining (either the buccal or lingual wall). In Class V, no cavity wall remains. This classification is useful in determining the need for a post.
Varvara et al felt the amount of residual dentin is important relative to failure load. However, it is the height of the remaining dentin and not the buccal thickness that affects the failure load. It is also thought that the height and location of the remaining tooth structure will affect the mechanical properties of the restored teeth.10
Dietschi et al reviewed the change in dentin composition, physical characteristics, fracture resistance, tooth stiffness, and restorative materials and techniques in an effort to delineate material selection and treatment of endodontically treated teeth.18 Endodontically treated teeth have a change in water content but this only modifies the Young modulus and proportional limit slightly; there is no decrease in compressive and tensile strength. Collagen cross-linking was the same in both vital and nonvital dentin.18
Sodium hypochlorite and ethylenediaminetetraacetic acid (chelator) and calcium hydroxide used for canal irrigation and disinfection modify the mineral content (chelator) or the organic substrate (sodium hypochlorite) of dentin. Chelators diminish calcium and may also affect noncollagenous proteins, resulting in softening. The proteolytic affect of sodium hypochlorite is possibly caused by fragmentation of long peptide chains (collagen).19 The use of disinfectants such as eugenol and formocresol result in increased dentin tensile strength as a result of protein coagulation and chelation with hydroxyapatite.20
Retention and cementation of fiber post
The use of fiber-reinforced composite-resin posts (FRC posts) has become popular in the last few years.21,22 The reason this has occurred is because the dentin-like modulus of elasticity of the FRC post allows better distribution of forces along the length of the root.10 The modulus of elasticity of composite resins (5.7 GPa to 25 GPa) and FRC posts (16 GPa to 40 GPa) provide elevated shock resistance, weakening of vibration, shock absorption, and augmented fatigue-resistance.23 The majority of the FRC posts contain a resin matrix with embedded glass or quartz fibers. Quartz fibers possess a higher tensile strength than glass fibers. The density, diameter, and adhesion of the fibers to the resin matrix vary in the different systems available and affect their strength.24 Resin is injected under pressure into preshaped molds containing prestressed fibers. The resin is usually an epoxy resin. The fibers in the FRC posts are designed to provide high tensile strength and the resin matrix is supposed to withstand compressive stresses and absorb stresses in the entire post system. Stresses can occur at the interface between the glass/silica fibers and resin matrix as the posts are loaded. This is because of their different elastic moduli. These stresses can result in voids, cracks, or micro bubbles and may weaken the post system. An increase in fiber/matrix and an increase in total interface area may lead to greater stiffness and a higher elastic modulus. However, increasing the stiffness of the FRC posts to a high value may result in root fractures (vertical or oblique) that require tooth extraction. Posts with an elastic modulus close to that of dentin are less prone to catastrophic fracture.25
Most posts are fabricated from E-glass fibers. R- and S-glass fibers have a smaller diameter and allow increased matrix spread to improve laminar tightness. The elastic modulus of D.T. LIGHT-POST® and D.T. LIGHT-POST Illusion (BISCO, Inc, Schaumburg, IL) is similar but its low thermal coefficient of expansion helps to maintain its structural integrity during thermal changes.
During the manufacturing process, the fibers are prestressed and soaked with resin and released after curing. This technique creates compression around the glass fibers resulting in reduced tensile stresses when the post is exposed to flexural forces. Seefeld et al also found a high degree of correlation between the fiber/matrix ratio and the flexural strength of these systems.25
Fiber posts are passively retained within the root canals. FRC posts are prevented from dislodgment by the luting agent adherence to the post and to the intraradicular dentin. There is also a need for adherence to the core material and the coronal dentin.26 Debonding has been a common cause of failure with FRC posts and usually occurs at the dentin interface. The pullout resistance of FRC posts decreases when the cement thickness is excessive.27
The bonding capacities of FRC are influenced by a variety of factors. The various designs and composition of the various post systems have a direct bearing on their retention and the resulting microleakage that may occur as a result of reduced bonding capability. High wall-to-wall contraction shrinkage may occur because thin resin films generate high shrinkage stress during polymerization. The composite flow is hindered by the confinement of the material bonded to the tooth in the pre-gel phase, and, as a result, contraction manifests itself as stress at the adhesive interface. The C-factor typically varies from 1 to 5 in intracoronal restorations; it exceeded 200 in the cementation of endodontic posts to root canal dentin. To evenly distribute the stress generated by functional load, minimize the contraction stress, and ensure a good bond between dentin and post, the composite cement should have a low conversion rate and, consequently, a low modulus of elasticity while maintaining a good mechanical resistance.28
The bonding quality to dentin is also a factor. There is decreased microleakage in teeth restored with bonded fiber-reinforced posts compared to teeth with posts that are not bonded.29 However, leakage along the post is still a problem. Bonfante et al found that the amount of uninterrupted interface between dentin and cement depended upon the resin cement used and the time of water storage. No gaps were seen at the cement-post interface, suggesting that bonds to dentin are weaker. Bonds were stronger at the cervical portion than at the apical portion. Water molecules diffuse into the resin matrix resulting in hydrolytic degradation and swelling of the composite.30
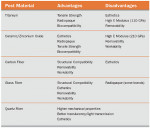
If the composite is only cured by light (Figure 2), insufficient light intensity will affect the degree of conversion at the apex and middle third. This reduced degree of conversion will result in the composite being adversely affected by moisture. It is harder to control moisture and placement of adhesive in the apical portion. The smear layer, sealer, and gutta-percha not cleaned off the walls can be found in the canal after acid-etching. They also concluded that the swelling of the composite from water sorption and resulting friction retain the post in the canal despite poor bond strengths.30
A variety of luting agents and the corresponding adhesives can be used to bond fiber posts into root canals. These adhesives can be of the self-etch or total-etch varieties. Giannini et al compared the influence of tubule density and areas of solid dentin using a self-etch system (Clearfil® Liner Bond 2V, Kuraray America, Inc, New York, NY) and an acetone-based system in a total-etch technique. They found the self-etching system was less sensitive to dentin depth and tubular depth compared to the acetone-based system.31 In a study by Zicari et al, the curing mode did not effect the push-out bond strength but dual-cure cements demonstrated poor sealing ability.32 Self-etching systems and total-etch systems sealed the root system much better than the self-adhesive cements. Etch-and-rinse alcohol-based adhesives are supposed to be applied to moist dentin but this is almost impossible to control in the canal. Cements that contain the self-etch 10-MDP (Clearfil® Esthetic Cement, Kuraray America) react with the hydroxyapatite in the hybrid layer to form a low-soluble MDP-calcium salt to improve long-term stability. Self-curing cements also seem to be the most effective in preventing microleakage, possibly because of better flow as a result of the slower self-polymerization reaction. Because the bond strength to root canal dentin is less than coronal dentin, it is important to maximize adhesive procedures.32
Ideally, the post diameter should be less than one third the diameter of the root at the cementoenamel junction and 1 mm or more of dentin should remain around the post. Post removal, internal resorption, or current coronal flaring to gain access to the apical aspect may result in reduced dentin thickness at the coronal portion. The reduced thickness of the coronal walls may decrease the effect of the ferrule. The restorative procedures required for endodontically treated teeth are dependent upon the amount of coronal dentin remaining.33
A 2-mm cervical ferrule increases fracture resistance with any luting material, but resin is superior. In addition, there will not be a close apposition between the post and the dentinal walls at the coronal portion of the canal and the luting agent has to fill in this space. The increased amount of luting material may result in the resin pulling away from the dentin as a result of polymerization shrinkage.29
A variety of resin cements with their associated bonding systems have been suggested for use with FRC posts. Resin cements are either traditional bis-GMA-based resin systems or adhesive resin cements having functional monomers, for example, 10-MDP or 4-Meta.22 The luting agents can also be divided into self-etching adhesives and etch-and-rinse systems. Recently, self-adhesive resins such as RelyX™ Unicem (3M ESPE, St Paul, MN) have been introduced. ContactCure® (Centrix, Shelton CT) and Multilink® (Ivoclar Vivadent, Amherst, NY) both contain self-etching primers. Multilink also contains a silane and a metal primer.
Influence of post and cores on light transmission through all-ceramic crowns
Usually all-ceramic restorations display optical behavior that mimics natural teeth. The optics of the ceramics is modified by its structure, the luting material, and any post and cores that may need to be placed. Some ceramic systems are semi-translucent (IPS Empress®, Ivoclar Vivadent) and others are semi-opaque (In-Ceram®, Vident, Brea, CA). A traditional metal post (gold or titanium) results in poor esthetics because of the lack of light transmission. The metal can be masked by opaque porcelain or opaque resin but the results are poor. This is because of the lack of light transmission at the coronal portion of the tooth and also to the periodontal tissues. Metallic posts also create a light blue/gray appearance at the gingival margin, possibly as a result of shadows. Ceramic, zirconium, and polyester with zirconium fibers (Snowlight®, Carbotech, Lewis Center, OH) allow more natural light transmission. In a study by Michalakis et al, a post made of zirconium fibers embedded in a polyester matrix allowed light transmission similar to a zirconia post.34 However, zirconium posts have a high degree of rigidity, are difficult to remove, are harder to bond, and are brittle.
A Sampling of Systems
RelyX™ Fiber Post (3M ESPE) is made of glass fibers embedded in a cured epoxy-resin matrix containing zirconia filler, which aids in the radiopacity of the post. The post contains 60% to 70% (by weight) glass fibers. The fibers are oriented longitudinally in the post and are dispersed homogeneously within the cross section of the post. The adhesion of the epoxy-resin to the glass fibers is a key point for excellent fatigue properties of the post.
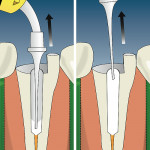
The composition of the RelyX Fiber Post provides an elastic modulus similar to dentin, allowing functional stresses to be dissipated rather than concentrated in the root. Therefore, the likelihood or potential for root fractures is reduced. The outer surface of RelyX Fiber Post has a microporous surface which aids in good mechanical retention of RelyX Unicem cement, which aids in the adhesive strength between the post and the cement. RelyX Fiber Post does not require pre-treatment when cemented with RelyX Unicem cement (Figure 3).
Dentatus Luscent™ Anchors (Dentatus USA Ltd, New York, NY) transmit polymerizing light within the confines of canals and provide a one-stop core anchor foundation with all restorative materials. They reflect natural hues for esthetic restorations and provide visible radiolucency in canals and through the core materials. They are available in three diameters to fit very slim and large canals. Dentatus Twin Luscent™ Anchors have a cone-shaped end that can be placed in deeper and narrower canals without excess removal of dentin or the canal wall. The parallel end can be alternately placed into long, wider canals of teeth. The parallel canals can be refined with drills and used in parallel-canal post techniques. A longitudinal vent groove eliminates trapped air bubbles for complete filling of the canal. Additionally, the vent groove creates an anti-rotational resistance in the surrounding polymerized resin material.
ParaPost® Fiber Lux/Taper Lux (Coltene Whaledent, Cuyahoga Falls, OH) is available in both parallel (Figure 4) and tapered Translucent Fiber Post Systems. The tapered post is recommended for teeth prepared with the crown-down technique and rotary endodontics. The post assumes the shape of the canal—wider coronally and narrowing apically. Less tooth structure has to be removed apically in preparation for the post, making this treatment a more conservative option. The rounded head is designed to reduce stress and lock in core material. It is light-transmitting for faster cementation and has a higher concentration of fibers for increased strength, with good radiopacity and removability.
GT®Fiber Posts (DENTSPLY Tulsa, Tulsa, OK) are composed from glass fiber and epoxy resin. They are sized to the Profile® GT-shaped canal and color-coordinated to match the GT family of products, and are parallel-sided and translucent for light transmission while curing.
FRC Postec® Plus (Ivoclar Vivadent) has been further developed from FRC Postec, which has been in successful clinical use for 5 years. It uses the combination of an innovative glass fiber material and a specially developed composite matrix to impart a natural translucency. FRC Postec Plus offers a high radiopacity similar to that of metal posts, but their design, consisting of glass fibers embedded in a composite matrix, produces a post with a modulus of elasticity similar to that of dentin, unlike metal or ceramic posts. In combination with Multilink and MultiCore, FRC Postec Plus produces effective, reproducible results because of a clear application protocol. The retention of adhesively cemented posts is three to four times higher than that of conventionally cemented posts in the root canal.
The UniCore™ Post and Drill System (Ultradent Products, Inc, South Jordan, UT) features a heat-dissipating, diamond-coated collar that eliminates excessive heat production caused by the friction of drill-to-tooth contact (Figure 55). The patented heat-generating tip softens the matrix of fiber posts, greatly simplifying their removal for retreatment and also greatly enhances the removal of stubborn rigid carriers like Thermafil® (DENTSPLY Tulsa), as well as gliding down canals filled with traditional gutta-percha or synthetic Resilon® (Pentron Clinical Technologies, LLC, Wallingford, CT) cones.
Specially designed flutes only cut the sides of the canal, never the bottom, so no zipping or stripping of the post chamber walls occurs. The UniCore Drill flutes quickly and efficiently remove material up and out of the post chamber. The drills and posts are color-coded according to size, making identification of matching posts and drills simple.
The FibreKleer® Post from Pentron Clinical Technologies is available in three body designs: parallel with a retentive head, tapered, and serrated. The transparency of the glass fibers allows light transmission through the post and makes FibreKleer Posts the ideal choice for use under all-ceramic restorations. FibreKleer posts have a flexural strength of 1,423 MPa for durability in high-stress areas and a flexural modulus engineered to minimize root fractures. They possess high radiopacity for easy detection on radiographs, are pre-silanated for convenience and enhanced adhesion of resin cements, and are easily retrieved using conventional burs and drill bits.
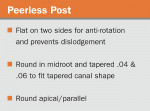
PeerlessPost™ (Sybron Endo, Orange, CA) features coronal and apical 1-mm adjustable sections (Figure 6) and comes in .04 and .06 tapered varieties. Composed of continuous, pre-stressed, high-quality fibers, they are customizable for every canal shape and length. With a low elastic modulus and high tensile and flexural strength, PeerlessPost absorbs and dissipates stress to prevent root fracture. They are bonded, not cemented; their retentive surface prevents rotation and dislodgement. Tooth-colored, radiopaque, and with three sections per post, they are easy to adapt, with minimal dentin removal.
The everStick®Post (Stick Tech Ltd, Turku, Finland) is a flexible, resin-impregnated glass fiber post that can be precision-shaped to the root canal and the core structure. Because it can be anatomically contoured, it is tissue saving. The unique interpenetrating polymer network (IPN) structure allows bonding of the everStick fibers with composites, adhesives, and composite cements. The IPN network also makes it possible to reactivate fiber surfaces for repair and allows for reinforcement of the pulp chamber area (the chamber can be tightly filled with fibers).
D.T. LIGHT-POST Illusion (BISCO) is an anatomical, two-taper design. Esthetic and light-transmitting, it has a flexural strength exceeding that of most metal posts with a modulus of elasticity close to dentin. Radiopaque for visibility on radiographs, it also features patented color-on-command technology. When the post is placed intraorally, the intrinsic color disappears. When retreatment is required the post will reappear on command by spraying water (Figure 7).
Rebilda Post (Voco Gmbh, Cuxhaven, Germany) has a modulus of elasticity of 24 GPa (90°), a transverse strength at 90° of 1,240 MPa, and a transverse strength at 45° of 1,904 MPa. It has a translucency of 27.2%, radiopacity of 350% Al, and a water absorption capacity of 10.6 µg/mm3.
LuxaPost® (Zenith Dental, Englewood, NJ) is a transparent glass-fiber reinforced composite post with a flexural modulus that reacts to pressure and stress much like natural dentin used in conjunction with LuxaBond® total-etch (Zenith Dental). The dual-curing adhesive system is compatible with all commercially available self-curing and dual-curing materials. No light is needed for LuxaBond. LuxaCore® Z-Dual can be used as the luting medium and core material. The manufacturer states the material has a 20 µm film thickness and 380 MPa compressive strength.
Flexi-Post® Fiber and Flexi-Flange® Fiber from Essential Dental Systems (Hackensack, NJ), have serrated heads that permit greater retention of core material. The second tier of the shank increases the intimacy of fit between the post and the natural point at which the canal widens. The Flexi-Post Fiber Vent releases internal hydrostatic pressure upon cementation. Flexi-Posts are made of an epoxy-reinforced S-glass fiber. Their threaded design is reported by the manufacturer to have greater retention than passive fiber posts without the need for a bonding agent. The manufacturer also reports that during tap insertion and thread-pattern creation, the patented Split-Shank Tap allows the stresses of insertion to be absorbed by the tap, not the root, virtually eliminating the major cause of root fracture. Vertical blades remove dentinal debris, enhancing ease of post placement.
Conclusion
No post-and-core system is ideal for all clinical situations. The ideal post should have the same shape as the endodontic preparation, and should be non-corrosive, readily adjusted, and able to be removed without difficulty. Radiopacity, minimal removal of tooth structure, and a modulus of elasticity similar to dentin are other important features, as are retentiveness in the canal and to the core.35 The post must provide all of the mechanical requirements needed to restore the tooth. The interaction of the modulus of elasticity and mechanical properties of the post with the luting material and core material are critical in the longevity of the restoration.
Disclosure
The author has received material support from the companies mentioned in this article.
References
1. Abou-Rass M, Donovan TE. The restoration of endodontically treated teeth. J Calif Dent Assoc. 1993;21(12):61-67.
2. Torabinejad M, Goodacre CJ. Endodontic or implant therapy. J Am Dent Assoc. 2006;137(7):973-977.
3. Torabinejad M, Andeson P, Bader J, et al. Outcomes of root canal treatment and restoration, implant-supported single crowns, fixed partial dentures, and extraction without replacement: a systematic review. J Prosthet Dent. 2007;98(5):285-311.
4. Guzy GE, Nicholls JI. In vitro comparison of intact endodontically treated teeth with and without endo-post reinforcement. J Prosthet Dent. 1979;42(1):39-34.
5. Trope M, Maltz DO, Tronstad L. Resistance to fracture of restored endodontically restored teeth. J Endod Dent Traumatol. 1985;1(3):108-111.
6. Sorensen JA, Martinoff JT. Intracoronal reinforcement and coronal coverage: a study of endodontically treated teeth. J Prosthet Dent. 1984;51(6):780-784.
7. Qing H, Zhu ZM, Chao YL, Zhang WQ. In vitro evaluation of the fracture resistance of anterior endodontically treated teeth restored with glass fiber and zircon posts. J Prosthet Dent. 2007;97(2):93-98.
8. Cheung W. A review of the management of endodontically treated teeth: post, core and the final restoration. J Am Dent Assoc. 2005;136(5): 611-619.
9. Peroz I, Blankenstein F, Lange K-P, Naumann M. Restoring endodontically treated teeth with post and cores: a review. Quintessence Int. 2005;36(9): 737-746.
10. Varvara G, Perinetti G, Dilorio D, et al. In vitro evaluation of fracture resistance and failure mode of internally restored endodontically treated maxillary incisors with different heights of residual dentin. J Prosthet Dent. 2007;98(5):365-372.
11. Sedgley CM, Messer HH. Are endodontically treated teeth more brittle? J Endod. 1992;18(7):332-335.
12. Papa J, Cain C, Messer HH. Moisture content of vital vs endodontically treated teeth. Endod Dent Traumatol. 1994;10(2):91-93.
13. Pilo R, Tamse A. Residual dentin thickness in mandibular premolars prepared with Gates Glidden and ParaPost drills. J Prosthet Dent. 2000;83(6):617-623.
14. Assif D, Gorfil C. Biomechanical considerations in restoring endodontically treated teeth. J Prosthet Dent. 1994;71(6):565-567.
15. Libman WJ, Nicholls JI. Load fatigue of teeth restored with cast posts and cores and complete crowns. Int J Prosthodont. 1995;8(2): 155-161.
16. Barkhordar RA, Radke R, Abbas J. Effect of metal collars on resistance of endodontically treated teeth to root fracture. J Prosthet Dent. 1989;61(6):676-678.
17. Glantz PO, Nilner K. Root canal posts—some prosthodontic aspects. Endod Dent Traumatol. 1986;2(6): 231-236.
18. Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature. Part I. Composition and micro-and macrostructure alterations. Quintessence Int. 2007:38(9):733-743.
19. Grigoratos D, Knowles J, Ng Y-L, Gulabivala K. Effect of exposing dentine to sodium hypo-chlorite and calcium. J Int Endod. 2001;34(2): 113-119.
20. Nakano F, Takahashi H, Nishimura F. Reinforcement mechanism of dentin mechanical properties by intracanal medicaments. Dent Mater J. 1999;18(3):304-313.
21. Perdigão J, Gomes G, Augusto V. The effect of dowel space on the bond strength of fiber posts. J Prosthodont. 2007;16(3):154-164.
22. Bitter K, Luckel HM, Priehen K, et al. Bond strengths of resin cements to fiber-reinforced composite posts. Am J Dent. 2006;19(3): 138-142.
23. Kececi AD, Ureyen Kaya B, Adanir N. Micro push-out bond strengths of four fiber-reinforced composite post systems and 2 luting materials. Oral Surg Oral Med Pathol Radiol Endod. 2008;105(1):121-128.
24. Grandini S, Goracci C, Monticelli F, et al: Fatigue resistance and structural characteristics of fiber posts: three-point bending test and SEM evaluation. Dent Mater. 2005;21(2):75-82.
25. Seefeld F, Wenz H-J, Ludwig K, Kern M. Resistance to fracture and structural characteristics of different fiber reinforced post systems. Dent Mater. 2007;23(3):265-271.
26. Goracci C, Grandinin S, Bossu M, et al. J Dent. 2007:35(11):827-835.
27. D’Arcangelo C, Cinelli M, De Angelis F, D’Amario M. The effect of resin cement film thickness on the pullout strength of a fiber reinforced post system. J Prosthet Dent. 2007;98(3):193-198.
28. Giachetti L, Scaminaci Russo D, Bertini F, Giuliani V. Translucent fiber post cementation using a light-curing adhesive/composite system: SEM analysis and pull-out test. J Dent. 2004;32(8):629-663.
29. Erkut S, Gilsahi K, Caglar A, et al. Op Dent. 2008;33:96-105.
30. Bonfante EA, Pegoraro LF, de Góes MF, Carvalho RM. SEM observation of the bond integrity of fiber-reinforced composite posts cemented into root canals. Dent Mater. 2008;24(4):483-491.
31. Giannini M, Carvalho R, Martins LRM, et al. The influence of tubule density and area of solid dentin on bond strength of two adhesive systems to dentin. J Adhesive Dent.2001;3(4):315-324.
32. Zicari F, Couthino E, Munck JD, et al. Bonding effectiveness and sealing ability of fiber-post bonding. Dent Mater. 2008; Jan 2; [Epub ahead of print].
33. Mezzomo E, Massa F, Libera SD. Fracture resistance of teeth restored with two different post-and-core designs cemented with two different cements: an in vitro study. Part I. Quintessence Int. 2003;34(4):301-306.
34. Michalakis KX, Hirayama H, Sfolkos J, Skolfos K. Light transmission of posts and cores used for the anterior esthetic region. Int J Periodontics Restorative Dent. 2004;24(5):462-469.
35. Peters J, Zyman G, Kogan E, et al. Retention of three endodontic post systems. Am J Dent. 2007;20(3):198-200.
About the author
Richard Trushkowsky, DDS
Associate Professor
Associate Director of International Aesthetics
New York University College of Dentistry
New York, New York
Private Practice
Staten Island, New York