Unilocular Ameloblastoma Simulating Periapical Lesion: The Importance of the Histopathologic Examination
Carlos Eduardo Xavier dos Santos Ribeiro da Silva, DDS; Artur Cerri, DDS;Francisco Octávio Pacca, DDS; Luc Louis Maurice Weckx, DDS; Ines Velez, DDS
The ameloblastoma is a benign, sometimes locally aggressive neoplasm that arises from the odontogenic epithelium of, primarily, the mandible. By means of histologic examination, it can be classified as uni- or multicystic. It is worth noting that the unicystic ameloblastoma behaves in a less aggressive manner than the multicystic type, and also shows a reduced potential for recurrence after treatment. Ameloblastoma occurs most often in younger patients (regardless of gender or ethnicity) in the posterior area of the mandible, and is commonly associated with an unerupted third molar.
In this article the authors will report on the case of a 25-year-old female Caucasian patient who presented with a radiolucent lesion in the area of an extracted molar. Surgical removal of the lesion was performed with the differential diagnosis of residual cyst vs chronic apical periodontitis caused by the adjacent premolar. Microscopic examination revealed acanthomatous ameloblastoma. The purpose of this article is to call attention to the importance of histopathologic examination of all tissue collected from the oral cavity, even though clinical and radiographic findings may divert attention to another form of pathology. The patient is presently under preventive surveillance, and shows signs of local bone regeneration.
THE AMELOBLASTOMA NEOPLASM
The ameloblastoma is a benign, locally aggressive neoplasm exclusively affecting the jawbones.1 Guzak first described it in 1826, and in 1879, Falkson performed a histological description.2 Ameloblastoma arises from odontogenic epithelium, but there are some doubts about the histogenesis. Different theories to explain the histogenesis of ameloblastomas postulate that these lesions may arise from the epithelial remnants of the enamel organ, proliferation of the epithelium that encases the odontogenic cysts, or even from the cells of the oral mucosa.3,4
The conventional ameloblastoma is a benign, locally invasive neoplasm with frequent recurrence after treatment. However, there are two related entities that are able to metastasize: the histologically benign ameloblastoma that exhibits malignant behavior, which is called malignant ameloblastoma, and the ameloblastoma with malignant microscopic manifestations, which is called ameloblastic carcinoma.5
The conventional ameloblastoma is an asymptomatic pathology with a slow evolution, occurring at any age. The most frequent multicystic variant occurs from the ages of 30 through the 70s, and the unicystic ameloblastoma is more common in the 20s.8 The occurrence of this lesion is independent of gender or ethnic origin. Approximately 80% of the cases affect the posterior area of the mandible and the ascending ramus.7 According to the World Health Organization, ameloblastomas are classified into the following types: conventional, unicystic, and peripheral. The histologic subtypes are desmoplastic, follicular, granular cell, plexiform, and acanthomatous.8,9 Radiographically, they manifest as osteolytic, well-defined, multilocular lesions showing bone septa that gives the ameloblastoma its “soap bubble” or “honeycomb” appearance. Early lesions are unilocular. The root resorption of the involved teeth occurs frequently.10,11
Curi et al12 advocate that when choosing therapy, the patient’s morbidity and quality of life must be taken into account because extensive resections provoke such problems as chewing difficulties, mutilation, facial deformity, and abnormal mandibular movements. The same authors observed the response in view of the surgical enucleation followed by cryosurgery in 46 cases of solid ameloblastomas. Surgical complications were evaluated by clinical and radiographic follow-up, and in 30.6% of the cases, there was a local recurrence.
In 1995, Feinberg and Steinberg,13 along with Neville,14 claimed that the recurrence ratio for solid ameloblastomas was between 15% to 25% whenever more radical measures were used.
Despite the fact that it is a benign neoplasm, oral surgeons have been discussing the therapy for the ameloblastoma because of its local common aggressive behavior. Extensive resections have been chosen for solid and multicystic ameloblastomas, whereas unicystic ameloblastomas were treated via enucleation. However, a certain tendency seems to exist among surgeons to adopt less aggressive procedures because the relapse ratios of the lesion are not very different when comparing conservative therapies (enucleation and cryosurgery) with radical ones (segmental resection with or without bone reconstruction).
In 2002, Nakamura et al15 described a conservative therapy for cystic ameloblastomas by means of marsupialization and posterior enucleation that turned out to be quite efficient and showed few relapses. Radiotherapy, as an auxiliary therapy for ameloblastoma, was recommended in the past and then discarded because, besides the risk of bone necrosis and malignant transformation caused by x-rays, the lesion is resistant to radiotherapy.16
CASE PRESENTATION
A 25-year-old female Caucasian patient was referred to the oral surgery department of the Universidade de Santo Amaro in São Paulo, Brazil, by the orthodontics department for evaluation of a radiolucent lesion in the area of the missing right inferior first molar. During the anamnesis the patient did not report any relevant information regarding medical history, family antecedents, or dental history, and she did not mention the use of any medication. Facial symmetry and normal texture of the skin were observed during examination of the face. When examining the head and neck, one inflammatory lymph node, in the right submandibular area, was identified. The remaining lymph nodes were within normal limits.
During the intraoral examination, the patient exhibited expansion of the mandible as well as normal color of the smooth, brilliant, and well-hydrated mucous membrane. Palpation revealed crepitice of the buccal bone wall, reflecting its thin composition. Radiographically, it presented as a radiolucent, unilocular lesion well defined by a radiopaque halo. The diameter measured approximately 2 cm, extending from the root of the mandibular right second molar to the root of the second premolar (Figure 1). The lesion also caused a displacement of the right alveolar canal towards the cortical inferior border of the mandible. No symptoms were reported but the lesion was aspirated to rule out intraosseous hemangioma, and the presence of a clear brownish liquid seemed to confirm the clinical and radiographic diagnosis of a cyst.
Because radiographically the lesion revealed the involvement of the root of the second premolar, vitality testing was performed, with negative results to heat and cold. Therefore, before surgery, root canal treatment with a long filling was requested on this nonvital tooth. The long filling was demanded to facilitate the detection of the root tip during the surgical procedure.
Standard procedures for surgery preparation were carried out with 0.12% chlorexidine. By means of a pterygomandibular technique, the patient was anesthetized on the right side with bupivacaine. An incision was made from the distal portion of the third inferior molar to the mesial region of the canine, followed by blunt gingival retraction. Much care was taken to preserve the integrity of the nerve. After release of the muco-periostal flap it was possible to see the thin, expanded, cortical plate, which was removed with a scalpel. The cavity was full of fluid, with a fibrous envelope around its borders. The enucleation was carried out very carefully and in one piece to ensure complete removal. The remaining bone tissue showed normal color and consistency without any clinical signs of pathosis. After replacement of the flap, it was secured using 4-0 silk sutures and the patient received the routine postsurgical instructions, along with prescriptions for antibiotics and anti-inflammatory drugs. The removed tissue was maintained in 10% formaldehyde and sent to the pathology laboratory.
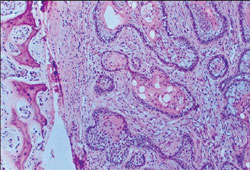
The histopathologic diagnosis was acanthomatous ameloblastoma with a cystic component. Because the clinical and radiographic diagnosis was not in agreement with the obtained results, the material was forwarded to another pathology laboratory, which confirmed the previous result (Figure 2).
X-ray observation of the patient to monitor the possibility of a relapse of the lesion was chosen because the lesion had a well-defined capsule and complete removal was possible. Presently, she is under follow-up for 12 months, with no sign of recurrence. Bone regeneration in the affected area is now seen (Figure 3).
DISCUSSION
The diagnosis in this case was possible only because the microscopic study was performed. It reinforces the importance of histologic examination of all tissues removed from the patient, regardless of the clinical diagnosis.
Because the ameloblastoma is known for its great potential of relapse and sometimes aggressive behavior, it is fundamental for the oral surgeon to maintain a regular and careful follow-up of a patient for several years.
CONCLUSION
Microscopic examination of all tissue removed from the oral cavity is of particular importance. The clinical and radiographic findings in this case suggested the presence of a periapical or residual cyst, but in fact it was a more aggressive lesion, ameloblastoma.
The ameloblastoma exhibits a variable prognosis that depends on a number of clinical and histological aspects. Extreme caution must be shown when dealing with lesions that require extensive surgeries. Periapical lesions are sometimes expansive and extremely large conditions that may mimic aggressive and destructive lesions.
References
1. Kramer IRH, Pindborg JJ, Shear M. Histological typing of odontogenic tumors. International Histological Classification of Tumours. 2nd ed. Heidelberg: Springer-Verlag; 1992: 11-14.
2. Shafer WG, Hine MK, Levy BM. Tratado de patologia bucal. 4th ed. Rio de Janeiro: Interacmericana; 1985:255-263.
3. Iordanidis S, Makos C, Dimitrakopoulos J, et al. Ameloblastoma of the maxilla. Case report. Aust Dent J. 1999;44(1):51-55.
4. Kawai T, Kishino M, Hiranuma H, et al. A unique case of desmoplastic ameloblastoma of the mandible: a report of a case and brief review of the English language literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87(2):258-263.
5. Maia Campos G. Ameloblastoma, a behavioral and histologic paradox (a philosophical approach). Braz Dent J. 1990;1(1): 5-15.
6. Kim SG, Jang HS. Ameloblastoma: a clinical, radiographic, and histopathologic analysis of 71 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91(6):649-653.
7. Gardner DG. Some current concepts on the pathology of ameloblastomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82(6):660-669.
8. World Health Organization (WHO); 1992. Available at: https://www.who.int/en/. Accessed February 1, 2007.
9. Isacsson G, Andersson L, Forsslund H, et al. Diagnosis and treatment of the unicystic ameloblastoma. Int J Oral Maxillofac Surg. 1986;15(6):759-764.
10. Regezi JA, Sciubba JJ. Oral Pathology: Clinical-Pathologic Correlations. Philadelphia: Saunders; 1989:554.
11. Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol. 1995;31B(2): 86-99.
12. Curi MM, Dib LL, Pinto DS. Management of solid ameloblastoma of the jaws with liquid nitrogen spray cryosurgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84(4):339-344.
13. Feinberg SE, Steinberg B. Surgical management of ameloblastoma. Current status of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81(4): 383-388.
14. Neville BW, Damm DD, Allen CM, et al. Oral & Maxillofacial Pathology. 2nd ed. Philadelphia: WB Saunders; 2002.
15. Nakamura N, Higuchi Y, Tashiro H, et al. Marsupialization of cystic ameloblastoma: a clinical and histopathologic study of the growth characteristics before and after marsupialization. J Oral Maxillofac Surg. 1995;53(7): 748-754, discussion 755-756.
16. Santos JN, Pinto LP, de Figueredo CR, et al. Odontogenic tumors: analysis of 127 cases. Pesqui Odontol Bras. 2001;15(4): 308-313.
 |
 |
|
| Figure 1 Panoramic radiograph showing a well-defined unilocular radiolucent lesion in the right mandible. | Figure 2 View of an acanthomatous ameloblastoma at 40X magnification. Note the epithelial islands of follicular type ameloblastoma with squamous metaplasia. | |
 |
||
| Figure 3 Note the bone regeneration at the 12-month follow-up. | ||
| About the Authors | ||
|
Carlos Eduardo Xavier dos Santos Ribeiro da Silva, DDS Professor Department of Otorhinolaryngology and Head and Neck Surgery Universidade de Santo Amaro Universidade Federal de São Paulo São Paulo, Brazil |
||
|
Artur Cerri, DDS Professor Universidade de Santo Amaro São Paulo, Brazil |
||
|
Francisco Octávio Pacca, DDS Professor Universidade de Santo Amaro São Paulo, Brazil |
||
|
Luc Louis Maurice Weckx, DDS Chief Department of Otorhinolaryngology and Head and Neck Surgery Universidade Federal de São Paulo São Paulo, Brazil |
||
|
Ines Velez, DDS Associate Professor and Director Oral and Maxillofacial Pathology Service Nova Southeastern University College of Dental Medicine Fort Lauderdale, Florida |
||



