Dental Implants: Mastering Esthetics in the Smile Zone
Lee H. Silverstein, DDS, MS; Gregori M. Kurtzman, DDS; David Kurtzman, DDS; and Peter C. Shatz, DDS
The key to contemporary restorative dentistry is the fabrication of healthy, maintainable, esthetic, and functional prostheses. The true success of any restoration is reliant on the creation of an “illusion of reality,”1 regardless of the restorative modality used (eg, porcelain laminate veneers, crowns, and/or implant-supported prostheses).2 Developments and advances to the restorative armamentarium have significantly improved the clinician’s ability to deliver predictable and reliable treatments. Osseointegration is one of the essential components of implant therapy.3 It is universally accepted that implant dentistry is a restorative-driven treatment with a surgical component. 4
Mastering esthetics in the smile zone with the use of implant-supported restorations should involve:
- Proper diagnosis of smile design; gingival contours
- The existence of proper biologic width
- Proper decision making on site development
- Soft and hard tissue grafting to correct unesthetic or functionally compromised anatomic abnormalities
- The removal of excessive gingival and alveolar bone for the correction of “gummy” smiles.
All of these factors need to be considered during the treatment sequencing process and performed before placement of dental implants5 or the restoration of natural tooth-supported restorations.6-8
These aforementioned procedures are the blueprint to establishing a proper gingival smile line with correct biologic width. Crown lengthening is critical to the success of creating a smile that is harmoniously balanced with its surrounding facial features.9-12 Consequently, patients who clinically display too much gingiva and short teeth require a thorough diagnosis and treatment plan to provide a predictable esthetic outcome.13-15 This is especially imperative with the use of dental implant restorations according to these authors and advocated by Vincent Kokich, DDS.5 If a patient has altered passive eruption (APE) of the maxillary anterior teeth, either secondary to orthodontic treatment or without orthodontic therapy but with completed facial growth,16,17 then the surgeon must first correct the gingival levels with either a gingivectomy or esthetic crown-lengthening procedure before the placement of dental implants to ensure that the eventual gingival margins of the maxillary anterior teeth will be at their correct level relative to the adjacent anterior teeth, not only after restoration of the implant, but also over the long term.18
Biological width dictates that there be at least 3 mm between the most apical extension of the restorative margin and the alveolar bone crest.19 This allows sufficient room for the supracrestal collagen fibers that are part of the periodontal support mechanism, as well as providing a gingival crevice of 2 mm to 3 mm.20,21 If this guideline is followed, the restorative margin should be positioned approximately midway between the gingival tissue margin and the depth of the sulcus.22 Failure to allow sufficient space between the crown margin, be it on a natural tooth or an implant, and the alveolar crest height results in the finished restoration being positioned too deep in the periodontal tissues, which can result in increased inflammation and possible periodontal pocket formation.23
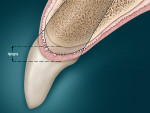
In a situation where no periodontal disease exists, the osseous structure roughly follows the scalloped parabolic contour of the cemento-enamel junction (CEJ), from facial to interproximal at an average distance of 2 mm to 3 mm.24,25 In addition, the average interproximal bone height is 3 mm coronal to the facial crest of bone (COB).26 Because the soft tissue topography is usually determined by the underlying hard tissue, this osseous “scallop” usually results in a gingival scallop of 3 mm.27 Examination of the periapical radiographs or periodontal vertical bite wings will allow the clinician to ascertain the position of the alveolar bone relative to the CEJ of the teeth28 to determine whether the COB is 2 mm to 3 mm apical to the CEJ, allowing for biologic width.29-31
However, in a clinical scenario where the COB is coronal to the CEJ, a condition results in APE.32-34 In this situation, the gingival margin will usually be located, on average, 3 mm coronal to the level of the COB, being more coronal on the body of the tooth and creating the appearance of a short clinical crown.35,36 These visual findings are coupled with the clinical information obtained by “bone sounding.” Bone sounding involves using a periodontal probe to locate the CEJ and determine whether it can be felt within the gingival sulcus or only when the probe penetrates through the base of the sulcus.37 Additionally, the periodontal probe is also used to feel for the COB. This value is expressed as a numerical distance in millimeters, revealing the distance between the COB and CEJ to ascertain whether there is sufficient biologic width.38Normally, the COB is 2 mm to 3 mm apical to the CEJ in a normal, non-diseased human periodontium.39
In addition to the gingival margin on the facial aspect of the teeth, in a non-diseased dentition the interproximal papilla between teeth with no bone loss due to periodontal disease is approximately 4.5 mm coronal to the interproximal COB. The mid-direct facial is about 1.5 mm more coronal to the COB. This additional 1.5 mm, with the 3-mm average osseous scallop from the CEJ, results in the tip of the papilla being an average of 4.5 mm coronal to the facial free gingival margin, where there is a “normal” periodontium, with no loss of bone or periodontal attachment due to periodontal disease.40
However, if the alveolar bone was situated in any other position other than normal, which is 2 mm to 3 mm apical from the CEJ, then these aforementioned values would not be the same and clinically relevant when used as a reference for the depth of a dental implant platform to allow for a proper emergence profile, according to the authors.
If implants are to replace missing teeth,then APE should be corrected before implant placement. In addition, if the patient has APE of the maxillary anterior segment, whether secondary to:
- orthodontic tooth movement;41
- a coronal gingival complex resulting from tissue hypertrophy secondary to plaque-induced inflammation;42
- medications such as calcium channel blocking agents, anticonvulsants, and immunosuppressant drugs;43
- deep decay causing short clinical crowns;44
- traumatic injury;44
- incisal attrition;45or
- tooth eruption and the patient has completed facial growth,46
The surgeon should first correct the aberrant gingival margins with an esthetic gingivectomy procedure, or the gingival margins and alveolar crest levels must be altered with an esthetic crown-lengthening procedure47 before the placement of the dental implant. These procedures can be accomplished at a separate surgical visit or at the time of dental implant placement but should be performed immediately before the preparation of the implant osteotomy, according to the authors and others.48,49 This will ensure that the eventual gingival margin over the dental implant will be at its correct level relative to the adjacent anterior teeth, according to the authors.
Clinical Guidelines
There are anatomic principles that act as parameters when practitioners perform esthetic gingival recontouring. A useful guide can be fabricated by the laboratory by modifying the mounted diagnostic casts so that the waxed modification reflects the ideal tooth anatomy desired in the final prosthesis, based on the guidelines previously published by Chiche and Pinault.50 These guidelines suggest that the average length for esthetically pleasing maxillary central incisors is 10 mm to 12 mm.51 These guidelines for the length of the central incisors, along with the recommended width-to-length ratio of 75% to 80%,52 should be kept in mind when recontouring the gingival tissues so as not to leave the teeth too long or too short.53
Once the central incisor proportions are achieved, practitioners should focus on the zenith or height of contour of the gingival margin on the centrals.54 The proper placement of the gingival zenith should be at the peak of the parabolic curvature of the gingival margin, which for the central incisors, cuspids, and bicuspids should specifically be located slightly distal to the middle of the long axis on these teeth. This gives the centrals, cuspids, and bicuspids the subtle distal root inclination that is paramount for the scaffold of a beautiful smile. The zenith for the lateral incisors is located at the midline of the long axis of the tooth. Furthermore, the height of the gingival crest for the lateral incisors should be 1 mm shorter than the gingival margins of the adjacent teeth. Additionally, the gingival tissues should be manipulated to have a resulting “knife-edge” gingival margin.55
Subsequent to the collection of the patient’s clinical data, which will reveal the presence of short clinical crowns and crestal bone levels approximating the CEJ, a diagnosis of APE can be made through the maxillary arch. The practitioner can then fabricate an esthetic guide that can be placed over the patient’s existing teeth to allow both the practitioner and patient to visualize what the smile will look like with the gingiva in a modified, more esthetic position.56
The repositioning of the gum line and crestal alveolar bone can be accomplished after the administration of local anesthetic. A periodontal probe is placed into the sulcus, attempting to locate the CEJ, but sometimes the CEJ cannot be discerned. In a case where the location of the CEJ is not clearly located, a periodontal probe should be passed through the periodontal attachment until the crest of alveolar bone is felt. Coupled with current periapical radiographs, the location of the crest of bone relative to the CEJ should be discernible.57
Periodontal, esthetic, and surgical crown-lengthening is then accomplished to correct the altered passive eruption. The laboratory-fabricated composite gingival esthetic guide can be used not only to position the alveolar crest 3 mm apical to the CEJ,58 but also to provide a blueprint for attaining horizontal gingival symmetry and height. The guide will also ensure proper interproximal scalloping based on the desired results. The newly established gingival margin will be determined by the patient’s lip line while smiling,59 the desired length of anterior teeth relative to the existing level of alveolar bone,60 and healthy interdental papillary tissue occupying the interdental spaces.61
Subsequent to scalloping the gingival tissues, an inverse beveled incision is made, connecting the sulci of the maxillary affected teeth. The surgical incision can transverse the base of the papillary tissue or it can follow the topography of the interdental papilla. For esthetic success at this critical phase of the crown-lengtheningprocess, it is important not to elevate the papilla, which usually will cause a loss of interproximal tissue height and may result in “black triangles.”
A full-thickness mucoperiosteal flap is then elevated with a periosteal elevator, and osseous resective techniques are performed with a surgical-length No. 8 round diamond bur and periodontal hand chisels to reshape the patient’s osseous bone margins. The surgical flap can then be positioned to the prearranged height determined by the esthetic surgical guide. The flaps are sutured using a 3/8 reverse cutting suture needle with a 4-0 thread size of polyglycolic acid (PGA), using a sling-suture technique. Suture removal is performed 10 days after surgery and the patient is instructed on the oral hygiene regimen to be used. This includes brushing with a soft-bristled toothbrush in a circular motion, and cleaning interdentally with either dental tape or floss.
After 10 weeks of postoperative healing, the cosmetic rehabilitation begins with the removal of the existing crowns. The teeth can be prepared with burs using the esthetic guide as the blueprint for tooth reduction. The restorations to be placed are ceramic crowns. These preparations are either placed at the free gingival margin or slightly subgingival on the facial aspect. Care should be taken not to violate the biologic width during the tooth preparation.62
Provisional restorations can be made by placing them in a vacuum-formed matrix made on the modified model, from which the esthetic surgical guide was fabricated, and then placed intraorally. After the appropriate time, approximately 60 to 90 seconds, the provisionals are removed and trimmed. The provisionals are bondedin place by spot-etching the preparations and using a luting material.
The occlusion should then be checked in the centric, protrusive, and lateral excursive positions63 and adjusted as needed. The patient should return to the office 10 days after insertion of the provisional restorations and provide input about what he/she likes and dislikes esthetically about the provisionals, and any changes that are desired. Subsequent to the recontouring of these provisional restorations to meet the patient’s expectations and gain the patient’s approval, impressions are taken and a putty matrix of the anterior segment is made to ensure the laboratory placed the incisal edges correctly.
Final impressions are obtained 6 to 8 weeks later64 by first placing a retraction cord, using a two-cord method with a woven cord, taking care not to injure the gingival tissues. Full-mouth impressions are taken with a vinyl polysiloxane facebow transfer, and open-bite centric relation records are obtained using registration material mounted in a semi-adjustable articulator. The case can be completed using full feldspathic porcelain crowns on teeth Nos. 6 through 11. Excess cement is removed with an explorer and periodontal scaler. The previously fabricated putty facial index should be placed to see if thereare any discrepancies, and any noted discrepancies should be modified.
The end result should be a healthy periodontal response and symmetry of the smile, which illustrates a completed healthy esthetic functional prosthetic result. The central incisors should demonstrate midline symmetry, as well as the correct 75% to 80% width-to-length ratio. In addition, the incisal smile line should follow the curvature of the lower lip. The newly established periodontal smile line should show a reduction of the gummy smile and make the smile more esthetically appealing and harmonious with surrounding facial features.65
Gingival levels should be assessed relative to the projected incisal edge position. The projected incisal edge position should be assessed relative to the position of the gingival levels. A predictable mode of determining the proper gingival positions is to determine the desired tooth size relative to the projected incisal edge position. The practitioner should remember that the incisal edge should not be positioned using the relative position of the gingival margin to create the proper tooth size. This is because the gingival margin can move with eruption or recession.66 Therefore, the proper gingival margin positions should be determined by establishing the correct width-to-length ratio of the maxillary anterior teeth.67 This can be accomplished by determining the desired amount of gingival display and creating symmetry between the teeth throughout the maxillary arch.68
In other words, if the existing position of the gingival margins creates the presence of a short clinical crown relative to the projected incisal edge position, then the gingival margins should be moved apically. This can be accomplished by performing esthetic crown lengthening, esthetic gingivectomy, orthodontic intrusion, and/or prosthetic rehabilitation.69 The procedure that is chosen to reposition the gum line is dependent upon several clinical factors, such as the location of the CEJ relative to the COB, the crown-to-root ratio and the shape of the root(s), the amountof existing tooth structure, and the sulcus/pocket depth. It is also paramount when establishing the proper position of the maxillary anterior teeth for an optimal cosmetic outcome to assess the levels of the interdental papillary tissues and their position relative to the crown length of the maxillary incisors.
One published article70 demonstrated that if the interdental contact is shorter than the interproximal papilla, then this could be an indication that there is clinically significant incisor abrasion. This scenario may cause shorter crowns, which shortens the contact between the central incisors. However, if the interdental contact point is longer than the papilla, then the gingival margin contour would be flat and usually located coronal to the CEJ, analogous to the clinical presentation of APE.71 The correction of this condition would be accomplished by performing esthetic crown lengthening72 and or orthodontic therapy to either extrude73 or intrude74the affected teeth.
Conclusion
Figure 1; Figure 2; Figure 3; Figure 4; Figure 5; Figure 6; Figure 7; Figure 8; and Figure 9 illustrate the concepts presented in this article. Patients who clinically display too much gingiva and short teeth require a thorough diagnosis and treatment plan to provide a predictable esthetic outcome. This is especially imperative with the use of implant restorations because, according to these authors, if a patient has APE of the maxillary anterior teeth, either secondary to orthodontic treatment or without orthodontic therapy but has completed facial growth, then the surgeon must first correct the gingival levels with either a gingivectomy or esthetic crown-lengthening procedure before the placement of dental implants. This will ensure that the eventual gingival margins of the maxillary anterior teeth will be at their correct level relative to the adjacent anterior teeth, not only after restoration of the implant, but also for a favorable long-term implant and/or natural tooth restoration.75It is essential that there be at least 3 mm between the most apical extension of the restorative margin and the alveolar bone crest. This allows sufficient room for the supracrestal collagen fibers that are part of the periodontal support mechanism, as well as providing a gingival crevice of 2 mm to 3 mm.
Essentially, the guideline of 3 mm on the facial from the COB to the gingival margin and 4 mm to 5 mm from the interproximal COB to the tip of the papilla for proper implant placement to allow for proper restorative contours would be irrelevant and erroneous if the periodontium and its hard and soft tissues were not located where they should be in a normal situation, with no bone and or attachment loss. Also, if the gingival marginis not located at the CEJ and the underlying bone is not 2 mm to 3 mm apical to the CEJ and after its parabolic contours, then the value of 3 mm on the facial and 4 mm to 5 mm on the interproximal area guideline for proper implant placement should not be used.
References
1. Niessen L. Customers for life: marketing oral health care to older adults: J Calf Dent Assoc.1999;27(9):724-727.
2. Goldstein RE, Belinfante L, Nahai F. Change Your Smile.3rd ed. Chicago, IL: Quintessence; 1997.
3. Francishone CE, Vasconcelos CW, Branemark PI. Osseointegration and Esthetics in Single Tooth Rehabilitation. Sao Paulo, Brazil:Quintessence Publishing, 2000.
4. Salama MA, Salama H, Garber DA. Guidelines for esthetic restorative options and implant site enhancement: The utilization of orthodontic extrusion. Pract Proced Aesthet Dent. 2002;14(2):125-130.
5. Kokich VG: Maxillary lateral incisor implants: the orthodontic perspective. Inside Dentistry.2006;2(9);32-39.
6. Chiche G. A Six-Step Approach to Demystifying Esthetics. Lecture presented at: American Association of Esthetic Dentistry Meeting;August 8, 1996; Philadelphia, PA.
7. Morley J: Altering gingival level: the restorative connections part I: biologic variables. J Am Dent Assoc.2001;132(1):39-45.
8. Glassman S. Cosmetic treatment of the gummy smile. Contemporary Esthetics and Restorative Practice.2001;5(1):58-61.
9. Rufenacht C. Fundamentals of Esthetics.Carol Stream, IL: Quintessence, 1990.
10. Morley J. A multidisciplinary approach to complex esthetic restoration with diagnostic planning. Pract Periodontics Aesthet Dent. 2000;12(6):575-577.
11. Silverstein LH, Shatz PC, Baker K. Subgingival technology to enhance the therapeutic outcome during surgical and restorative phases of smile reconstruction. Contemporary Esthetics and Restorative Practice. 2002;6(7):40-47.
12. Levine RA, Randel H. Multidisciplinary Approach to Solving Cosmetic Dilemmas in the Esthetic Zone. Contemporary Esthetics and Restorative Practice. 2001;5(6):62-67.
13. Chiche G, Kokich V, Caudill R. Diagnosis and Treatment Planning of Esthetic Problems. In: Pinault A, Chiche G, eds. Esthetics of Anterior Fixed Prosthodontics, Chicago, Quintessence, 1994.
14. Studer S, Zellweger U, Scharer P. The aesthetic guidelines of the mucogingival complex for fixed prosthodontics. Pract Periodontics Aesthet Dent.1996;8(4):333-341.
15. Kois JC. Altering gingival level: The restorative connections. Part I: Biological variables. J Esthet Dent.1994;6(1):3-9.
16. Kokich VG. Managing Orthodontic–Restorative Treatment for the Adolescent Patient. In: McNamara JA Jr, ed. Orthodontics and Dentofacial Orthopedics.2001; Ann Arbor, Michigan: Needham Press; 395-422.
17. Kokich V. Esthetics and anterior tooth position:an orthodontic perspective, Part III: Mediolateral relationships. J Esthet Dent.1993;5(5):200-207.
18. Rufenacht C. Structural Esthetic Rules. In: Fundamentals Of Esthetics. 1992; Chicago,IL: Quintessence Publishing; 67, 134.
19. Carranza FA, Newman MG. Clinical Periodontology. 8th ed. 1996; Philadelphia, Pa: WBSaunders Company; 720-722.
20. Gargiulo AW, Wentz FM, Orban B. Dimensions and relations of the dentogingival junction in humans. J Periodontol. 1961;32:261-267.
21. Kois JC. The restorative-periodontal interface: biological parameters. Periodontal 2000. 1996;11:29-38.
22. Goldstein RE. Esthetics in Dentistry. 1976; Philadelphia, PA: Lippincott; 425-455.
23. Smukler H, Chaibi M. Periodontal and dental considerations in clinical crown extension. A rational basis for treatment. Int J Periodontics Restorative Dent. 1997;17(5):464-477.
24. Hirshfeld I. A study of skulls in the American Museum of Natural History in relation to periodontal disease. J Dent Res. 1923;5:241-275.
25. Weinman JP, Sicher H. Bone and Bones. Fundamentals of Bone Biology. 2nd ed. 1955; St Louis, Mo: CV Mosby.
26. Hermann JS, Cochran DL, Nummikoski PV, et al. Crestal bone changes around titanium implants. A radiographic evaluation of unloaded nonsubmerged and submerged implants in the canine model. J Periodontol.1997;68(11):1117-1130.
27. Saadoun AP, Le Gall MG, Touati B. Current trends in implantology: Part II—treatment planning, esthetic considerations, and tissue regeneration. Pract Proced Aesthet Dent. 2004;16(10):707-714.
28. Levine RA, McGuire M. Diagnosis and treatment of the gummy smile. Compend Contin Educ Dent. 1997;18(8):757-764.
29. Garber DA, Salama MA. The aesthetic smile: diagnosis and treatment. Periodontol 2000. 1996;11:18-28.
30. Landsberg CJ, Sarne O. Management of excessive gingival display following adult orthodontic treatment: A case report. Pract Proced Aesthet Dent. 2006;18(2):89-96.
31. Coslet JG, Vanarsdall R, Weisgold A. Diagnosis and classification of delayed passive eruption of the dentogingival junction in the adult. Alpha Omegan. 1997;70(3):24-28.
32. Pulliam RP, Melker D. Altered passive eruption: diagnosis and treatment. Contemporary Esthetics and Restorative Practice.2002;6(4):20-30.
33. Robbins JW. Esthetic gingival recontouring-cavet emptor. Contemporary Esthetics and Restorative Practice.2002;6(4):66-674.
34. Allen EP. Surgical crown lengthening for function and esthetics. Dent Clin North Am.1993;37(2):163-179.
35. Dolt AH 3rd, Robbins JW. Altered passive eruption: an etiology of short clinical crowns. Quintessence Int. 1997;28(6):363-372.
36. Townsend CL: Resective surgery: an esthetic application. Quintessence Int. 1993;24(8):535-542.
37. Rosenberg ES, Cho SC, Garber DA. Crown lengthening revisited. Compend Contin Educ Dent. 1999;20(6):527-534.
38. Periodontal Probing—What Does It Mean? In: Garnick JJ, Silverstein LH. Clark’s Clinical Dentistry.Vol. 3. 1993; Philadelphia, Pa: JB Lippincott; 115.
39. Ten Cate AR: The Development of the Periodontium. In: Melcher AH, Bowen WH, eds. Biology of the Periodontium. 1969; New York,NY: Academic Press, Inc.
40. Spear FA: The esthetic management of multiple missing anterior teeth. Inside Dentistry.2007;3(1):72-76.
41. Kokich VG, Kokich VO. Interrelationship of Orthodontics with Periodontics and Restorative Dentistry. In: Nanda R, ed. Biomechanics and Esthetic Strategies in Clinical Orthodontics. 2005; St Louis, Mo: WB Saunders; 348-373.
42. Silverstein LH, Garnick JJ, Stein SH, et al. Medication-induced gingival enlargement: a clinical review. Gen Dent. 1997;45(4)371-378.
43. Silverstein LH, Koch JP, Lefkove MD, et al. Nifedipine-induced gingival enlargement around dental implants: a clinical report. J Oral Implantol.1995;21(2):116-120.
44. Goldstein RE: Esthetics In Dentistry.2006; Hamilton Ontario, Canada: BC Decker.
45. Magne P, Magne M, Belser U. Natural and restorative oral esthetics. Part I: Rationale and basic strategies for successful esthetic rehabilitations. J Esthet Dent. 1993;5(4):161-173.
46. Amstad-Jossi M, Schroeder HE. Age-related alterations of periodontal structures around the cemento-enamel junction and the gingival connective tissue composition in germ free rats. J Periodont Res.1978;13(1):76.
47. Clinicians’ Guide To Peri-Implantology. In: Silverstein LH, Meffert RM, Jeffcoat M, et al. Clark’s Clinical Dentistry. Vol. 5. 1998; St Louis, Mo: Mosby Year Book.
48. Francischone CE, Oltramari PV, Vasconcelos LW, et al. Treatment for predictable multidisciplinary implantology, orthodontics, and restorative dentistry. Pract Proced Aesthet Dent.2003;15(4):321-326.
49. Levine RA, Katz D. Developing a team approach to complex esthetics: treatment considerations. Pract Proced Aesthet Dent. 2003;15(4):301-306.
50. Chiche G, Pinault A. Esthetics of Anterior Fixed Prosthodontics.1994; Carol Stream, Ill: Quintessence Publishing.
51. Singer BA. Principles of esthetics. Curr Opin Cosmet Dent.1994;6-12.
52. Sterrett JD, Oliver T, Robinson F, et al. Width/length ratios of normal clinical crowns of the maxillary anterior dentition in man. J Clin Periodontol.1999;26(3):153-157.
53. Spear FM, Kokich VG, Mathews DP. Interdisciplinary management of anterior dental esthetics. J Am Dent Assoc. 2006;137(2): 160-169.
54. Ahmad I. Geometric considerations in anterior dental esthetics: restorative principles. Pract Periodontics Aesthet Dent. 1998;10(7):813-822.
55. Chalifoux PR. Checklist to esthetic dentistry. Pract Periodontics Aesthet Dent. 1990;2(1):9-12.
56. Spear F. Construction and use of a surgical guide for anterior periodontal surgery. Contemporary Esthetics and Restorative Practice. 1999;12-20.
57. Garnick JJ, Silverstein LH. Periodontal probing: probe tip diameter. J Periodontol. 2000;71(1):96-103.
58. Singer BA. Fundamentals of Esthetics. In: Dale BG, Aschheim CW, eds. Esthetic Dentistry. A Clinical Approach to Techniques and Materials. 1993; Philadelphia, Pa: Mosby; 5-13.
59. Van der Geld PA, van Waas MA. The smile line: a literature search. Ned Tijdschr Tandheelkd. 2003;110(9):350-354.
60. Kois JC. Predictable single-tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2004;25(11):895-898.
61. Kan JY, Rung Charassaeng K, Umezu K, et al. Dimensions of peri-implant mucosa: an evaluation of maxillary anterior single implants in humans. J Periodontol. 2003;74(4):557-562.
62. Silness J. Periodontal conditions in patients treated with dental bridges. 3. The relationship between the location of the crown margin and the periodontal condition. J Periodontal Res. 1970;5(3):225.
63. Wolffe GN, van der Weijden FA, Spanauf AJ, et al. Lengthening clinical crowns—a solution for specific periodontal, restorative, and esthetic problems. Quintessence Int.1994;25(2):81-88.
64. Hornbrook DJ. Cementation of all ceramic veneers using the “tack & wave” technique. Contemporary Esthetics and Restorative Practice. 2002;6(4):36-48.
65. Rufenacht CR. Principles of Esthetic Integration. 2000; Germany: Quintessence Publishing; 73-97.
66. Gottlieb B, Orban B. Active and passive eruption of the teeth. J Dent Res.1933;3:214.
67. Gillen RJ, Schwartz RS, Hilton TJ, et al. Analysis of selected normative tooth proportions. Int J Prosthodont. 1994;7(5):410-417.
68. Becker W, Ochsenbein C, Becker BE. Crown lengthening: the periodontal-restorative connection. Compend Contin Educ Dent. 1998;19(3):234-242.
69. Kokich V. Esthetics and anterior tooth position: an orthodontic perspective. Part I: Crown length. J Esthet Dent. 1993;5(1):19-23.
70. Kokich VG, Kokich VO. Orthodontic Therapy for the Periodontal-Restorative Patient. In: Rose LF, Mealey B, Genco R, Cohen D, eds. Periodontics: Medicine, Surgery, and Implants. 2nd ed. 2004; St. Louis, Mo: Mosby;718-744.
71. Spear FM. Maintenance of the interdental papilla following anterior tooth removal. Prac Periodontics Aesthet Dent. 1999;11(1):21-28.
72. Kokich VG, Spear F. Guidelines for treating the orthodontic-restorative patient. Orthod Dento Facial Orthop. 1997;3:3-20.
73. Koyuturk AE, Malkoc S. Orthodontic extrusion of subgingivally fractured incisor before restoration. A case report: 3-years follow-up. Dent Traumatol. 2005;21(3):174-178.
74. Salama H, Salama M, Kelly J. The orthodontic-periodontal connection in implant site development. Pract Periodontics Aesthet Dent. 1996;8(9):923-932.
75. Silverstein LH, Kurtzman D, Cohen R, et al. Adjunctive Orchestrated Orthodontic Therapy: an emerging trend in cosmetic dentistry. Alpha Omegan. 2001;94(4):27-33.
About the Authors
Lee H. Silverstein, DDS, MS
Associate Clinical Professor of Periodontics
Medical College of Georgia
Augusta, Georgia
Private Practice,
Marietta, Georgia
Gregori M. Kurtzman, DDS
Private Practice
Silver Spring, Maryland
David Kurtzman, DDS
General Private Practice
Hospital-Based Practice Treating Special
Needs Patients
Marietta, Georgia
Peter C. Shatz, DDS
Assistant Clinical Professor of Periodontics
Medical College of Georgia
Augusta, Georgia
Private Practice,
Marietta, Georgia