A Discussion of the Safety and Efficacy of Four Tooth Bleaching Modalities
Ralph H. Leonard, DDS, MPH
Tooth bleaching remains of great interest to the public and the profession. The use of assorted products and techniques continues to escalate, whether in and from dental practices or purchased over-the-counter. The majority of bleaching solutions contain hydrogen peroxide or carbamide peroxide as the active ingredient delivered in various carrier designs.1,2 As dental professionals, we have an obligation to pursue scientific knowledge about what is available to treat our patients’ teeth so that we can differentiate between effective and safe bleaching methods and those that are marketed based on promotional speculation.
During the 17 years since nightguard vital bleaching was first described in the literature, many patients have enjoyed the benefits of treating their teeth through this method.2 Concurrently, other approaches to tooth bleaching have gained in popularity, including in-office bleaching; extended bleaching, primarily for tetracycline stained teeth; and over-the-counter products (eg, hydrogen peroxide based strips; paint-on bleaching solutions; abrasive dentifrices; etc).
This article discusses these four modalities for tooth bleaching. A brief review of the literature is summarized for each to address the efficacy and safety that they may or may not have demonstrated. The intent is to impress upon readers the need to thoroughly evaluate available treatment regimens so that patients can be properly advised of all of their options and what the implications of their use could be.
NIGHTGUARD VITAL BLEACHING
Since its introduction in 1989, nightguard vital bleaching has been proven to be a simple and predictable procedure to lighten discolored teeth.2,3 The efficacy of the technique has been shown to be 98% for nontetracycline stained teeth;4 and with extended treatment time (see below), tetracycline stained teeth can be expected to lighten in at least 86% of cases.3,5 What’s more, long-term retention of the shade change at a satisfactory level—without re-treatment—can be expected in at least 43% of cases at 10 years posttreatment;3,6 82% satisfactory shade retention was reported in another study at up to 47 months posttreatment.3,7
Side effects associated with nightguard vital bleaching are usually mild and transient, disappearing within days of treatment completion, with no long-term sequelae to the hard or soft tissues.3-7 The two most common side effects reported for nightguard vital bleaching are tooth sensitivity and gingival irritation.4,8
Long-term posttreatment, nightguard vital bleaching has been proven safe. At 10 or more years posttreatment, patients recalled for clinical evaluation demonstrated gingival index and tooth vitality findings that were considered to be within normal expectations (Figure 1; Figure 2View Figure; Figure 3).6 At that time, no cervical resorption or pulpal pathology was diagnosed.6
Nightguard vital whitening with 10% carbamide peroxide has also been shown to have no significant affect on surface or subsurface enamel microhardness.9,10 At 10 years post-treatment, scanning electron microscopy (SEM) observations did not reveal substantial differences between treated and nontreated tooth surfaces.6
Although some clinicians initially feared that tooth bleaching would result in increased incidence of the need for endodontic therapy, 10-year to 12-year posttreatment follow-up of patients who underwent nightguard vital bleaching indicates that this isn’t the case (Figure 4).6 Additionally, a study conducted on the 2-week use of 10% carbamide peroxide found that the slight histological changes that are sometimes observed after bleaching tend to resolve within 2 weeks posttreatment; they did not affect the overall health of the pulp tissue and are reversible.11
As noted previously, research has shown that nightguard vital whitening does not have a significantly negative effect on enamel structures. Further, it has also been shown that tooth bleaching with 10% carbamide peroxide, 35% hydrogen peroxide, or 20% carbamide peroxide with fluoride does not increase a patient’s susceptibility to caries.12
EXTENDED BLEACHING FOR TETRACYCLINE STAINS
Predicting the success of bleaching tetracycline-stained teeth is difficult. If the tetracycline stain is primarily incisal, the likelihood of successfully bleaching to achieve an esthetic result is better than if the stain appears along the gingival one-third of the tooth. However, tray bleaching has been used for extended treatment-time periods (ie, 6 months) to improve the appearance of teeth with tetracycline stains, with long-term color stability and efficacy (Figure 5; Figure 6; Figure 7).3,5
One longitudinal study in particular showed that at 90 months posttreatment, after 6 months of active nightguard vital bleaching with 10% carbamide peroxide, there was still shade stability.5 Additionally, patients participating in the study were overwhelmingly positive about the procedure in terms of shade retention, as well as a lack of posttreatment side-effects.5
Of patients with tetracycline stains who underwent 6 months of nightguard vital bleaching treatment and participated in the 7.5-year recall study, none reported having to have a crown or root canal that they believed was treatment-related.5 They also reported no tooth sensitivity. Visual assessment and thorough examinations did not reveal any fractured teeth, caries, or pulpal/enamel changes (Figure 5; Figure 6; Figure 7).
OVER-THE-COUNTER PRODUCTS
A variety of over-the-counter (OTC) products are available. Studies have demonstrated that some of them work,13,14 while others—because of their novelty and/or proprietary nature—we know nothing about in terms of their efficacy and safety because they have not undergone rigorous and objective clinical testing.1 The efficacy of any bleaching product is determined by its active ingredient, concentration, and treatment time. Because these products are used in an unsupervised manner, the exact nature of their efficacy and safe use is hard to establish and monitor.
Understandably, problems may arise with the use of OTC tooth bleaching products as a result of how they work, how long they take to work, the ingredients they contain, and their misuse by patients. In some instances, it may be more cost-effective, efficient, and safe for the patient to undergo in-office bleaching or dentist-monitored bleaching than pursue OTC alternatives.
Hydrogen Peroxide Strips
When hydrogen peroxide bleaching strips were introduced, studies were conducted to demonstrate their effectiveness in improving color, as well as to evaluate posttreatment color retention.13,14 They were found to be effective (Figure 8 and Figure 9) and well-tolerated (ie, minor tooth sensitivity and oral irritation); most initial color changes remained stable at 6 months posttreatment.13,14
Further, the strips were found to be safe in terms of their effects on subsurface microhardness and ultrastructure of tooth enamel and coronal dentin.9,15 When human tooth enamel specimens were cycled through a daily regimen including salivary immersions and treatments with commercial tooth bleaching gels and strips containing hydrogen peroxide or carbamide peroxide, the peroxide bleaching compositions had no affects or no significant affects on surface or subsurface microhardness of enamel or dentin.9,15
However, other OTC bleaching products can negatively affect the enamel surface microhardness, and potential adverse effects can occur when these products are used inappropriately.8 The risks associated with using higher-concentration at-home OTC bleaching products without a dentist’s supervision are yet to be determined.8
Paint-on Bleaching Solutions
Among the newest OTC bleaching products available to consumers are paint-on bleaching solutions. To date, limited data is available in the literature regarding the efficacy and safety of these bleaching solutions.10
Research indicates that some formulations provide improved whitening compared to others.16-18 The amount of shade change of paint-on solutions when compared to a tray-based system is less and, at this time, longevity of shade change is unknown. Additionally, the guidelines by which the color change was assessed may or may not have understandable clinical relevance in terms of shade changes.
Of particular importance to dentists and their patients, however, are the safety issues surrounding the use of paint-on solutions. The results of an in vitro study showed that consumer-available, paint-on bleaching solutions adversely affected enamel microhardness at some time during the study, compared to a control and 10% carbamide peroxide dentist-prescribed, home-applied bleaching product.10
In-Office Bleaching
In-office bleaching has been performed successfully in the dental office for many years. Its recently increased popularly can be attributed to many factors, not the least of which is patients’ desires to achieve a more esthetic, whiter smile in the fastest way possible. To this end, various high concentrations of carbamide peroxide and hydrogen peroxide solutions can be applied in the dental office to achieve tooth bleaching.
It may take multiple in-office bleaching appointments—and/or a combination of in-office bleaching and take-home nightguard vital bleaching—to achieve the patient’s desired results. In one study, it was found that from one to four in-office bleaching procedures were necessary to achieve patient satisfaction with the color change.19 The average color change per appointment was 2.1 to 3.7 units using a 16-scale Vita Classic shade guide; and color relapse was more noticeable 2 weeks post-treatment compared to the 6-month follow-up.19 Therefore, a caveat of evaluating the success of in-office bleaching is that final color change results should be evaluated at least 5 days to 7 days after bleaching to allow for color stabilization and regression.
As far as safety issues are concerned, in-office tooth bleaching with the highest concentration of hydrogen peroxide (ie, 35%) and the maximum likely exposure has been shown in tests to produce no evidence of deleterious effects on enamel or dentin.20 Additionally, other tests have demonstrated that in-office power bleaching produces minimal enamel surface changes and does not affect enamel hardness.21
Given the efficacy and safety associated with traditional methods of in-office tooth bleaching, prudent clinicians should question the necessity of applying various light sources to the bleaching agent in order to achieve faster and/or better treatment results. This is particularly important considering that—to date—data is lacking in the scientific literature that documents the long-term safety or efficacy of light-activated bleaching procedures. Further, what has been published in the literature does at times seem conflicting and confusing.
As reported by Tavares et al, the use of a light increased the tooth whitening effect of the hydrogen peroxide gel when compared to the gel alone during a single visit appointment.22 The statistically significant effect from baseline noted immediately after treatment was maintained at the 6-month post-treatment appointment. Side effects reported by participant of the study were similar to other studies.22
In some cases, tooth color and temperature changes have been significantly affected by an interaction of the bleaching agent and light variables (eg, halogen curing light, infrared light, argon laser, CO2 laser).23 The application of lights significantly improved the bleaching efficacy of some bleach materials, but it caused significant temperature increases in the outer and inner tooth surfaces.23 In another instance, the use of an ultraviolet light was shown to improve the bleaching effect of a peroxide gel that contained a photo activator by 26% compared to treating with the gel alone.24
However, other researchers have examined the effects of different light sources on in-office hydrogen peroxide treatment solutions and have determined that the lights did not bleach teeth more than the bleaching gels alone.25 Rather, the laboratory tests indicated that the proprietary chemicals mixed into each bleaching gel before use acted as catalysts and were probably responsible for more rapid lightening; neither the heat produced by the accessory lights, nor the light output itself, were responsible for the catalytic activity.25 Other scientists also have found no benefit to the use of light compared to a chemically activated tooth bleaching system after a 2-week recall.26
As mentioned earlier, the literature suggests that caution must be exercised in terms of what type of light activation is used and for how long in order to avoid potentially detrimental effects to the tooth and the pulp.23 In a study that examined—among other things—the temperature rise in the pulp chamber when a tooth was exposed to bleaching gel and a variety of light-curing units, it was found that the use of intense lights does elevate bleach temperature and also results in increased intrapulpal temperatures.27 The researchers suggested that this may further impact patient sensitivity and pulpal health as a result of the whitening treatment.27
CONCLUSION
Tooth bleaching procedures that are dentist-monitored, such as nightguard vital bleaching, have been proven safe and effective for the long term. Color stability has been demonstrated over time and minimal-to-no side effects have been reported. It also has been proven safe and effective for extended bleaching of tetracycline stained teeth for up to 6 months. In-office bleaching using either hydrogen or carbamide peroxide according to tested and proven techniques can be confidently recommended and used for treating patients’ teeth. Overall, risks to patients and their dentition are minimized when bleaching procedures and their related products are supplied and supervised by dentists; professionals can diagnose any problems or special needs and plan the bleaching treatment appropriately.28
References
1. Kugel G. Over-the-counter tooth-whitening systems. Compend Contin Educ Dent. 2003;24(4A): 376-82.2. Haywood VB, Heymann HO. Nightguard vital bleaching. Quintessence Int. 1989;20(3):173-176.
3. Leonard RH Jr. Long-term treatment results with nightguard vital bleaching. Compend Contin Educ Dent. 2003;24(4A):364-374.
4. Haywood VB, Leonard RH, Nelson CF, et al. Effectiveness, side effects and long-term status of nightguard vital bleaching. J Am Dent Assoc. 1994;125(9):1219-1226.
5. Leonard RH Jr, Haywood VB, Caplan DJ, et al. Nightguard vital bleaching of tetracycline-stained teeth: 90 months post treatment. J Esthet Restor Dent. 2003;15(3): 142-152.
6. Ritter AV, Leonard RH Jr, St Georges AJ, et al. Safety and stability of nightguard vital bleaching: 9 to 12 years post-treatment. J Esthet Restor Dent. 2002;14(5):275-285.
7. Leonard RH Jr, Bentley C, Eagle JC, et al. Nightguard vital bleaching: a long-term study on efficacy, shade retention, side effects, and patients’ perceptions. J Esthet Restor Dent. 2001;13(6): 357-369.
8. Li Y. The safety of peroxide-containing at-home tooth whiteners. Compend Contin Educ Dent. 2003;24(4A):384-389.
9. Teixeira EC, Ritter AV, Thompson JY, et al. Effect of tray-based and trayless tooth whitening systems on microhardness of enamel surface and subsurface. Am J Dent. 2004;17(6):433-436.
10. Leonard RH, Teixeira EC, Garland, GE, et al. Effect on enamel microhardness of two consumer-available bleaching solutions when compared with a dentist-prescribed, home-applied bleaching solution and a control. J Esthet Restor Dent. 2005;17(6): 343-350.
11. Fugaro JO, Nordahl I, Fugaro OJ, et al. Pulp reaction to vital bleaching. Oper Dent. 2004;29(4):363-368.
12. Al-Qunaian TA. The effect of whitening agents on caries susceptibility of human enamel. Oper Dent. 2005;30(2):265-270.
13. Gerlach RW, Barker ML. Professional vital bleaching using a thin and concentrated peroxide gel on whitening strips: An integrated clinical summary. J Contemp Dent Pract. 2004;5:1-13.
14. Gerlach RW, Gibb RD, Sagel PA. Initial color change and color retention with a hydrogen peroxide bleaching strip. Am J Dent. 2002;15(1): 3-7.
15. White DJ, Kozak KM, Zoladz JR, et al. Effects of Crest Whitestrips bleaching on subsurface microhardness and ultrastructure of tooth enamel and coronal dentin. Am J Dent. 2004;17(1):5-11.
16. Barlow A, Gerlach RW, Date RF, et al. Clinical response of two brush-applied peroxide whitening systems. J Clin Dent. 2003;14(3):59-63.
17. Li Y, Lee SS, Cartwright S, et al. Comparative tooth whitening efficacy of 18% carbamide peroxide liquid whitening gel using three different regimens. J Clin Dent. 2004;15(1):11-16.
18. Elais A, Santo Domingo W, Petrone M, et al. Tooth whitening efficacy: Colgate Simply White and Crest Night Effects. IADR/AADR. 2004; Abstract #2131.
19. de Silva Gottardi M, Brackett MG, Haywood VB. Number of in-office light-activated bleaching treatments needed to achieve patient satisfaction. Quintessence Int. 2006;37(2):115-120.
20. Sulieman M, Addy M, Macdonald E, et al. A safety study in vitro for the effects of an in-office bleaching system on the integrity of enamel and dentine. J Dent. 2004;32(7):581-590.
21. Garland GE, Leonard RH, Ritter AV, et al. Enamel surface and hardness changes during power bleaching. AADR. 2003; Abstract #0917.
22. Tavares M, Stultz J, Newman M, et al. Light augments tooth whitening with peroxide. J Am Dent Assoc. 2003;134(2):167-175.
23. Luk K, Tam L, Hubert M. Effect of light energy on peroxide tooth bleaching. J Am Dent Assoc. 2004;135(2):194-201.
24. Ziemba SL, Felix H, MacDonald J, et al. Clinical evaluation of a novel dental whitening lamp and light-catalyzed peroxide gel. J Clin Dent. 2005;16(4):123-127.
25. Hein DK, Ploeger BJ, Hartup JK, et al. In-office vital tooth bleaching—what do lights add? Compend Contin Educ Dent. 2003;24(4A): 340-352.
26. Kugel G, Papathanasiou A, Williams AJ 3rd, et al. Clinical evaluation of chemical and light-activated tooth whitening systems. Compend Contin Educ Dent. 2006;27(1):54-62.
27. Baik JW, Rueggeberg FA, Liewehr FR. Effect of light-enhanced bleaching on in vitro surface and intrapulpal temperature rise. J Esthet Restor Dent. 2001;13(6):370-378.
28. Haywood VB. Historical development of whiteners: clinical safety and efficacy. Dent Update. 1997;24(3):98-104.
 |  | |
| Figure 1 Preoperative view of a male patient who presented for tooth whitening; a nonvital but asymptomatic discolored tooth was present. | Figure 2 View of the same patient's teeth at three years postbleaching. | |
 | 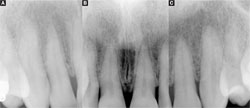 | |
| Figure 3 View of the same patient's teeth at 12 years postbleaching. Note the appearance of the healthy gums; no tooth fractures or other adverse affects were noted. | Figure 4 A radiograph taken at 16 years postbleaching demonstrates that, long-term, no abnormalities are present from an endodontic standpoint as a result of the whitening treatment. | |
 |  | |
| Figure 5 Prebleaching view of a patient with tetracycline-stained teeth. | Figure 6 Postbleaching image of the patient in Figure 5 showing the efficacy of extended bleaching. | |
 |  | |
| Figure 7 View of the same patient at 7.5 years postbleaching, demonstrating the longevity of the whitening effects on tetracycline-stained teeth and color stability. | Figure 8 Pretreatment view of patient who elected to whiten their teeth using the over-thecounter strip/hydrogen peroxide method. | |
 | ||
| Figure 9 Postbleaching view showing that the OTC product did improve the tooth color. | ||
| About the Author | ||
 Ralph H. Leonard, DDS, MPH Ralph H. Leonard, DDS, MPHDepartment of Diagnostic Sciences and General Dentistry University of North Carolina School of Dentistry Chapel Hill, North Carolina | ||



