Cuspid Disclusion: Is It Not Academic?
Chris Stevens, DDS
The benefits of cuspid-protected lateral excursions have been debated for decades. Some clinicians and academicians felt cuspid rise was mandatory for case success while others pointed out that alternate disclusion schemes, such as group function, were just as reliable. Yet, without appropriate and objective measurement tools, the debate was based primarily on opinion. Today, however, easily applied, PC-enhanced recording means are available. With the proper application of these measurement tools, clinicians are now able to evaluate the need and benefits of occlusion and disclusion protocols.
This article will review the literature regarding disclusion schemes. A case report will then be presented in which the benefit of disclusion by cuspid protection can be demonstrated through the use of objective PC-enhanced instrumentation.
LITERATURE REVIEW
To study the various occlusion and disclusion schemes, some authors have used intraoral splints as a means of modifying the scheme. Grubwieser and colleagues1 studied two different anterior guidance patterns using splints. One splint provided an anterior canine guidance and the second splint provided bilaterally balanced occlusion. The study statistically concurred with previous data that all subjects whose muscle activities were observed with anterior guidance showed significantly lower values than subjects wearing the splint with bilateral balanced occlusion. Fitins and coworkers2 studied the effect of canine guidance of a full-arch, maxillary flat occlusal splint on the level of activation of the anterior and posterior, temporal, masseter, and suprahyoid muscles during maximal clenching in subjects without craniomandibular disorders. The results revealed that the level of activation of the jaw elevator muscles decreased significantly during maximal clenching on the cuspid ramp of the splint as compared to clenching on the splint. The decrease was most noteworthy in the ipsilateral masseter and the contralateral anterior and posterior temporal muscles. Williamson and colleagues3 made splints for subjects that gave both anterior guidance and posterior disclusion. Electromyography (EMG) was used to measure the splint effects. All subjects showed lessened muscle activity when anterior guidance took over on the splints. They went on to conclude that posterior group function elevated muscle activity levels during excursions.
Manns et al4 combined EMG and a full-coverage occlusal splint to compare two types of occlusal guidances: group function and canine guidance. The purpose was to determine which of the two occlusal schemes causes a greater reduction in muscle activity and thereby a decrease in muscle tension in eccentric mandibular positions. Left- and right-side integrated EMG recordings were made of the masseter and temporal muscles during static (clenching) and dynamic (lateral excursion and clenching) max-imal contractions. The results showed an EMG activity reduction of the elevator muscles with group function relative to their activity in centric occlusion. A more marked reduction was observed on the mediotrusive side, mainly in the temporal muscle. With canine guidance, the reduction in elevator muscle activity was much greater, more significant, and mainly in the temporal muscle of the mediotrusive side. The clinical implications of this study suggest the use of canine guidance in laterotrusion for therapy with full-coverage occlusal splints.
The effects of disclusion schemes have also been evaluated in patients with craniomandibular disorders and patients with parafunction. Miralles and colleagues5 studied electromyographic recordings made from the anterior temporal and masseter muscles during maximal voluntary clenching with complete dentures in the intercuspal position and in the laterotrusive jaw position with balanced occlusion and canine guidance. The lower activity in both muscles with canine guidance suggested that canine guidance may be a significant factor for preventing parafunctional activity in edentulous patients. Okano and coworkers6 found simulated canine-protected occlusion was associated with the lowest EMG activity, suggesting that this occlusal pattern has the capacity to reduce the level of parafunctional activity. Ott and colleagues7 looked at the electrical activity of the masseter and anterior temporal muscles during empty mastication before and after the canines were treated with build-ups in a patient group with muscular and temporomandibular joint (TMJ) problems and matched their observations against the results obtained in a control group. With cuspid build-ups allowing correct cuspid guidance, the patients with muscular and TMJ problems were symptom-free after just 3 days.
On the other hand, Rugh et al8 questioned the importance of canine disclusion in parafunctional subjects. They noted that the use of interocclusal orthopedic appliances is the most common method for managing nocturnal bruxism and associated craniomandibular symptoms and posterior disclusion, with canine or anterior guidance believed to be a key feature. The purpose of this study was to compare a canine versus molar guidance appliance in eight chronic bruxism patients. The appliances were used for 10 to 14 nights. The two appliances provided nearly equivalent effects on nocturnal bruxism in seven of eight subjects. Clinical examination and subjective pain ratings did not differ with the two guidance patterns. These results made them question the common assumption that canine guidance is a critical design feature for the management of nocturnal bruxism and associated craniomandibular symptoms.
Numerous clinical studies have indicated that the lack of canine disclusion can damage the dentition. Mayhew and colleagues9 evaluated the relationship of occlusal stress factors, periodontal health status, and acidic dietary patterns to the presence of noncarious cervical lesions (NCCL). Forty-three subjects were admitted into the study and 178 teeth exhibiting NCCL were evaluated. They concluded that group function that may evolve with age and/or traumatic occlusion factors may be related to the etiology of NCCL.
Most authors do feel canine disclusion is preferable. Akoren et al10 completed a study to investigate two occlusal schemes, canine guidance and group function, in relation to masticatory muscle activity. Bilateral electromyographic recordings of masseter and anterior temporal muscles were obtained by surface electrodes during gum chewing and sliding laterally from centric relation while the teeth were in contact. Canine guidance reduced anterior temporal muscle activity during sliding. This suggested that in the presence of healthy and good supportive canine teeth, canine guidance occlusion will be preferable. Leiva and coworkers11 used integrated electromyography to determine the effects of laterotrusive occlusal schemes and body position on bilateral sternocleidomastoid activity. Subjects seated in the upright position had significantly lower activity with canine guidance than in group function.
CASE REPORT
The patient in this case was a healthy 53-year-old man who had been referred to the author’s practice by another patient who had had a smile enhancement. He was unhappy that he could not see his front teeth when he smiled and that his teeth varied widely in color (Figure 1 ; Figure 2; Figure 3; Figure 4). He requested that the author fix his six front teeth.
Dental History
The patient’s dental history involved traditional dentistry, several large amalgam restorations and porcelain-fused-to-metal crowns. He did have localized adult periodontitis and was under the care of a periodontist. When the author examined the periodontium, he discovered that slightly elevated bleeding indexes were confined to the lower left molars and, although other areas had residual pocketing, there was no bleeding. Because of this, he determined that the patient’s periodontium would support planned restorative care.
Comprehensive Evaluation
Because of existing occlusal disease, including occlusal wear, anterior chipping, and abfractions, the author was concerned about the health of the TMJ complex even though the patient reported no symptoms when asked to complete a symptomatic history fashioned after the Kinnie-Funt-Stack Visual Index. The author used bioelectric instrumentation from Bio-Research Associates, Inc (Milwaukee, WI), which has been proven reliable in assessing the TMJ complex,12-24 to evaluate the patient’s TMJ health. He also obtained corrected bilateral, multipositional, and parasagittal tomograms (Figure 5A and Figure 5B).
Case Planning
The first step in planning was to evaluate the 3-dimensional relationship of the mandible to the maxilla. This relationship would have to be altered to increase the length of the central incisors. The author used neuromuscular techniques to find the physiologic rest position and determine the vertical, anterior?posterior, and lateral position of the mandible. He used computer-enhanced jaw tracking to record isotonic closure through freeway from physiologic rest and noted closure along a physiologic trajectory. The patient’s centric occlusal position was on that trajectory with a freeway space of 1 mm. This position was recorded with an acrylic bite registration medium called blue Sapphire™ (Bosworth, Inc, Skokie, IL). The author measured incisal length by determining the patient’s phonetic f- and v-point.
The laboratory (Arrowhead Dental Laboratory, Sandy, UT) mounted the maxillary and mandibular casts with the occlusal registration on the Accu-Liner™ articulator (Accu-Liner Products, Woodinville, WA). They used the hamular notch?incisive papilla (HIP) plane, which is a very reliable horizontal reference plane of the skull that Dr. Harry Cooperman introduced to dentistry in 196025,26 to mount the maxillary cast. The laboratory used the occlusal registration to mount the mandibular cast relative to the maxillary cast, then removed the mandibular cast from the articulator and set the provided stage in place. They duplicated the central incisor length, as determined by the f- and v-point, on the central incisors of the cast and lowered the maxillary cast so that the intended incisal edge of the centrals contacted the stage of the articulator. Finally, the laboratory completed the maxillary wax-up to the ideal plane against the stage (Figure 6 and Figure 7).
Preparation
Once the wax-ups were completed, the laboratory made temporary stints and reduction guides and the case was ready for preparations. First, the author performed laser-assisted tissue recontouring to place gingival zeniths in the appropriate position for each tooth—both independently and in relation to one another.
The author opted to prepare all 28 teeth in one visit, starting with teeth Nos. 3 through 7 and 10 through 14. The integrity of the occlusal registration was maintained by using the unprepared teeth to properly orient and reline the original blue Sapphire bite registration in the prepared areas with LuxaBite™ (Zenith Dental™, Englewood, NJ). Then the four remaining maxillary teeth were prepared. Shoulder margins for IPS Empress® (Ivoclar Vivadent®, Amherst, NY) restorations were left in all preparations. These would be cemented with composite resin cement.
The four mandibular molars were prepared to receive porcelain-fused-to-high-noble-gold crowns, which would be cemented with glass ionomer cement. Because of the margins of previously placed dentistry, there was concern for isolation needed for resin cementing on these teeth. All other mandibular teeth were prepared for IPS Empress and the arch prepared in the same manner as for the maxillary teeth, maintaining the bite registration through closed segmental reline.
The next step in the preparations was to obtain the color mapping, smile selection, and preparation (stump) shades with necessary photographs. The author made a stick bite to horizontal, which allowed the laboratory to compare the horizontal to the stage of the Accu-Liner articulator and remove the potential for canting in the final restorations.
Integrity™ (DENTSPLY/Caulk, Milford, DE) was loaded into the temporary Sil-Tech® (Ivoclar Vivadent) stints made from the wax-ups to fabricate provisionals. The stints, first the maxillary and then the mandibular, were loaded, vibrated to reduce bubbles, and seated against the preparations. The palate and tuberosities were used as positive stops for placing even pressure. The anterior portion of the stints was rubbed with a finger to thin excess and to make the stints easier to remove. They were removed 2 minutes after placement. A #15 scalpel and fine carbide burs were used to remove excess material. The provisionals were very attractive when they were finished (Figure 8).
The occlusion, esthetics of the provisionals, and home care were evaluated 3 days after preparation. At this time, any changes to the provisionals were noted and related to the laboratory so they could produce the final restorations to the patient’s satisfaction.
Cementation
When it was time for cementation/bonding, the maxillary provisionals were sectioned and removed after lingual anesthetization and the preparations were cleaned with Concepsis® scrub (Ultradent Products, Inc, South Jordan, UT), an ICB® (intracoronal brush, Ultradent), and then Concepsis liquid. The units were fitted, both independently and as a group, to determine proximal contact. After confirming each unit’s fit, the author placed the anterior segment and viewed its midline, length, and canting. He found it necessary to use try-in paste to observe the color.
The patient accepted the restorations, and then they were removed, rinsed thoroughly, and etched with 37% phosphoric acid. The author applied Silane primer (Kerr Corporation, Orange, CA) followed by the appropriate shade of Variolink® II bonding resin (Ivoclar Vivadent) to the restoration. They were then placed in a light-free environment in the Crown and Bridge Organizer (C & B Organizer, North Salt Lake, UT) which also logs their respective position in the arch.
To prevent saliva contamination, the rubber dam was placed in a trough format and the palate was sealed with bite registration material. The teeth were etched for 12 seconds, then washed and moisture-controlled. Ultracid®(Ultradent) was used as the wetting agent. The teeth were bonded using Opti-Bond® Solo Plus™ (Kerr) adhesive. The maxillary arch was seated first, then the mandibular, using the same method. Starting with the two central incisors, the units were placed and reasonable attempts were made to remove excess bonding resin without dislodging the restoration. The gingival area was tacked to maintain the position of the unit while the others were placed. The lateral and cuspid were placed, one side then the other, and tacked in place. The process of front-to-back placement was continued until all of the units were tacked using a 4-mm light guide for 5 seconds.
Using care not to dislodge the units, the author flossed interproximal areas to remove excess bonding resin. Multiple light units expedited final curing. Any remaining bonding resin was removed with a 12-bladed scalpel, fine finishing burs, and diamond-impregnated finishing strips. The rubber dam was then removed.
Once both arches were seated, the author performed preliminary occlusal adjustments. Adjustments were done only to remove obvious centric occlusion prematurities (Figure 9 and Figure 10), because the anesthesia reduced the patient’s occlusal awareness.
Final Adjustments
The patient returned to the office 48 hours later for residual bonding resin removal and initiation of occlusal balancing. Balancing was accomplished by using the T-Scan® II Occlusal Analysis System (TekScan, Inc., South Boston, MA). This system accurately records the timing of occlusal contacts and the forces generated by them.
The T-Scan II measures occlusal contact in real time and has the ability to disclose time and force data. Occlusal data is recorded by instructing the patient to occlude on an intraoral sensor that is connected to a computer. This time and force measurement capability allows the clinician to optimize occlusal contact patterns precisely, thereby attaining measurable verification of what has been theorized as ideal occlusal parameters in many classical occlusal principles.27-30
The data displayed on the monitor represents the maxillary arch. Data can be displayed in various formats including the 2-dimensional contour view and the 3-D columnar view. The 2-D view resembles articulation paper marks and the 3-D view makes force viewing easy when compared to the color-coded force legend. The force vs time graph allows the clinician to view time between initial tooth contact and last tooth contact, which is ideally less than 0.2 seconds.31
Follow-up
Six months postcementation, the patient returned for a recall visit. At that time he related a concern of bilateral temporal headaches. After taking and reviewing his updated history, the decision was made to evaluate his disclusion for any unwanted posterior contacts during the lateral excursion. This was accomplished using two separate technologies that have been recently synchronized. TekScan, Inc. and BioResearch, Inc. have developed a synchronized capability of recording and analyzing diagnostic data simultaneously. This simultaneous recording capability allows the operator to review and correlate occlusal movements to electromyographic data. Therefore, occlusal movements can be correlated to specific EMG changes that result from those movements.
Along with evaluation for potential unwanted posterior contact in anterior disclusion, the length of time to perform the disclusion was also analyzed. Disclusion time is defined as the duration of time that working and nonworking molars and premolars are in contact during a mandibular excursive movement that commences from the habitual closure position through to the contact of anterior guiding surfaces. Disclusion time was first described by Kerstein and Wright,32 who felt disclusion should be complete within 0.5 seconds of commencement.
During the right lateral excursion (Figure 11) it was evident that although the primary contact was on the right canine, there were contacts on the ipsilateral posterior teeth. These contacts, indicative of group function, were strong enough to move the summation of total contact force to an area just distal to the first premolar. Raw EMG images demonstrated elevated ipsilateral temporalis activity and numeric EMG analysis showed that 31 mv of temporalis muscular activity was required to perform this occlusal activity. The time for the lateral excursion to occur was just less than 0.4 seconds.
After adjustments to remove unwanted posterior contacts were made, a new synchronized recording was obtained (Figure 12). Note that all contact was confined to the right canine. EMG analysis showed a reduction of needed muscular activity to a level of 11 mv or about one third of the previously required level. The time for complete disclusion to occur was still less than 0.4 seconds.
During the left lateral excursion (Figure 13) it was again evident that pure canine disclusion was not occurring. Raw EMG images again demonstrated elevated ipsilateral temporalis activity and numeric EMG analysis showed that 30 mv of temporalis muscular activity was required to perform this occlusal activity. Also, it took just over 0.6 seconds for this function to occur.
After further adjustments to remove unwanted contacts were made, a new synchronized recording was obtained (Figure 14). The contact was removed from all posterior teeth. EMG analysis showed a reduction of needed muscular activity to a level of 8 mv or less than one third of the previously required level. Furthermore, the excursion required just over 0.4 seconds to occur.
Successive follow-up recall visits have since been done. This patient now remains in a totally asymptomatic state with appropriate occlusion and disclusion schemes. The use of objective recording tools was invaluable not only to recognize that a problem existed but to verify treatment was suitable and complete.
DISCUSSION
Anterior guidance, categorized as group function or canine guidance, is considered essential for esthetics, phonetics, and mastication. Thorton33 reviewed the historical development and philosophies of both occlusal schemes. At the time of the review, there was no scientific evidence to support one occlusal scheme over the other. However, it was felt that where anterior guidance must be reestablished or where it changes, there currently appeared to be more authorities who favor canine guidance over group function. Hobo34 reported, in evaluating anterior guidance and the condylar path, that posterior disclusion is crucial in controlling harmful lateral forces.
CONCLUSION
This patient presented with several occlusal signs of dysfunction as well as esthetic concerns but exhibited no symptoms. Through comprehensive evaluation a diagnosis, treatment plan, and prognosis were developed, all before initiation of restorative care. Nevertheless, the patient still required precise occlusal adjustment. Stable and efficient occlusion was not enough to ensure the patient’s comfort with the restorative care. Precise and time-based canine disclusion was also a critical component in the success of this patient’s care.
DISCLAIMER
The author teaches for Arrowhead Dental Laboratory, TekScan, Inc, and BioResearch, Inc, but receives no monies from the sale of their products.
References
1. Grubwieser G, Flatz A, Grunert I, et al. Quantitative analysis of masseter and temporalis EMGs: a comparison of anterior guided versus balanced occlusal concepts in patients wearing complete dentures. J Oral Rehabil. 1999;26(9): 731-736.2. Fitins D, Sheikholeslam A. Effect of canine guidance of maxillary occlusal splint on level of activation of masticatory muscles. Swed Dent J. 1993;17(6):235-241.
3. Williamson EH, and Lundquist, DO. Anterior guidance: its effect on electromyographic activity of the temporal and masseter muscles. J Prosthet Dent. 1983; 49(6):816-823.
4. Manns A, Chan C, Miralles R. Influence of group function and canine guidance on electromyographic activity of elevator muscles. J Prosthet Dent. 1987;57(4):494-501.
5. Miralles R, Bull R, Manns A, et al. Influence of balanced occlusion and canine guidance on electromyographic activity of elevator muscles in complete denture wearers. J Prosthet Dent. 1989;61(4): 494-498.
6. Okano N, Baba K, Akishige S, et al. The influence of altered occlusal guidance on condylar displacement. J Oral Rehabil. 2002;29(11): 1091-1098.
7. Ott RW, Lechner KH. Cuspid protection and muscular reaction. Dtsch Zahnarztl Z. 1989;44(1):30-33.
8. Rugh JD, Graham GS, Smith JC, et al. Effects of canine versus molar occlusal splint guidance on nocturnal bruxism and craniomandibular symptomatology. J Craniomandib Disord. 1989;3(4):203-210.
9. Mayhew RB, Jessee SA, Martin RE. Association of occlusal, periodontal, and dietary factors with the presence of non-carious cervical dental lesions. Am J Dent. 1998;11(1):29-32.
10. Akoren AC, Karaagaclioglu L. Comparison of the electromyographic activity of individuals with canine guidance and group function occlusion. J Oral Rehabil. 1995;22(1):73-77.
11. Leiva M, Miralles R, Palazzi C, et al. Effect of laterotrusive occlusal scheme and body position on bilateral sternocleidomastoid EMG activity. Cranio. 2003;21(2):99-109.
12. Bessette RW. “A Clinical Study of Temporomandibular Joint Vibrations in TMJ Dysfunction Studies.” Presentation at the American Academy of Head, Neck, and Facial Pain, and TMJ Orthopedics. Kansas City, MO. August 15, 1992.
13. Brooks CP. Joint Vibration Analysis in 314 Patients Presenting with TM Dysfunction: Correlation with Clinical and Tomographic Data. Presentation at the 8th International Congress, International College of Craniomandibular Orthopedics. Banff, Alberta, Canada. October 1993.
14. Ishigaki I, Bessette RW, Maruyama T. Vibration of the temporomandibular joints with normal radiographic findings: Comparison between asymptomatic volunteers and symptomatic patients. J Craniomandib Prac. 1993: 11(2):88-94.
15. Ishigaki S, Bessette RW, Maruyama T. Vibration analysis of the temporomandibular joints with meniscal displacement with and without reduction. J Craniomandib Prac. 1993;11(3):192-201.
16. Ishigaki S, Bessette RW, Maruyama T. Vibration analysis of the temporomandibular joints with degenerative joint disease. J Craniomandib Prac. 1993;11(4): 276-283.
17. Ishigaki S, Bessette RW, Maruyama T. Diagnostic ability of the surface vibration analysis of the temporomandibular joint. International Association of Dental Research. Seattle, WA; March 1994.
18. Chong-Shan S. Proportionality of mean voltage of masseter muscle to maximum bite force applied for diagnosing temporomandibular joint disturbance syndrome. J Prosthet Dent. 1989:62: 682-684.
19. Clark GT, Beemsterboer PL, Solberg WK, Rugh JD. Nocturnal electromyographic evaluation of myofascial pain dysfunction in patients undergoing occlusal splint therapy. J Am Dent Assoc. 1981;99:607-611.
20. Dahlstrom L. Electromyographic studies of craniomandibular disorders: A review of the literature. J Oral Rehabil. 1989;16:1-20.
21. Gervais R, Fitzsimmons GW, Thomas NR. Masseter and temporalis electromyographic activity in asymptomatic, subclinical, and temporomandibular joint dysfunction patients. J Craniomandib Prac. 1989;7:52-57.
22. Bell WE. Clinical management of temporomandibular disorders. Yearbook Medical Publishers, Chicago/London; 1986.
23. Bessette RW. Role of mandibular tracking in temporomandibular joint surgery. Oral and Maxillofacial Surgery Clinics of North America. 1989;1: 205-220.
24. Michler L, Bakke M, Moller E. Graphic assessment of natural mandibular movements. J Craniomandib Disorders Fac & Oral Pain. 1987;1:97-114.
25. Cooperman HN. Willard SB. Studies of the Louchheim Collection of Skulls. New York: American Museum of Natural History, 1960.
26. Cooperman HN. The H.I.P. Plane of Occlusion in Oral Diagnosis. Dental Survey Nov. 1975;60-62.
27. Kerstein RB. Current applications of computerized occlusal analysis in dental medicine. Gen Dent. 2001;49(5):521-530.
28. Dawson PE. Diagnosis and Treatment of Occlusal Problems. 2nd ed. St. Louis: CV Mosby Co.;1989.
29. Schuyler CH. Fundamental principles in the correction of occlusal disharmony, natural and artificial. J Am Dent Assoc. 1935;66: 1193-1202.
30. Glickman L. Clinical Periodontology. 4th ed. Philadelphia: W.B. Saunders Co.;1972.
31. Kerstein RB, Grundset K. Obtaining bilateral simultaneous occlusal contacts and a straight line path of closure with computer analyzed and guided occlusal adjustments. Quintessence Int. 2001;32(1): 7-18.
32. Kerstein RB, Wright NR. Electomyographic and computer analyses of patients suffering from chronic myofascial pain-dysfunction syndrome: before and after treatment with immediate complete anterior guidance development. J Prosthet Dent. 1991;66(5):677-686.
33. Thornton LJ. Anterior guidance: group function/canine guidance. A literature review. J Prosthet Dent. 1990;64(4): 479-482.
34. Hobo S. Twin-tables technique for occlusal rehabilitation: Part I: Mechanism of anterior guidance. J Prosthet Dent. 1991;66 (3):299-303.
 |  | |
| Figure 1 Preoperative view, unretracted smile. Note the reverse smile curve. Reprinted courtesy of Dentistry Today. | Figure 2 Preoperative view, retracted smile. Reprinted courtesy of Dentistry Today. | |
 |  | |
| Figure 3 Preoperative view, maxillary arch. Reprinted courtesy of Dentistry Today. | Figure 4 Preoperative view, mandibular arch. Reprinted courtesy of Dentistry Today. | |
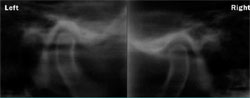 | ||
| Figure 5A and 5B Left and right tomographic temporomandibular joint views in the closed position. Reprinted courtesy of Dentistry Today. | ||
 |  | |
| Figure 6 Maxillary wax-up on stage of Accu- Liner articulator. Note level occlusal plane. Reprinted courtesy of Dentistry Today. | Figure 7 Completed wax-up on Accu-Liner articulator. Reprinted courtesy of Dentistry Today. | |
 |  | |
| Figure 8 Provisionals in place. Reprinted courtesy of Dentistry Today. | Figure 9 Unretracted postcementation view of the smile. Reprinted courtesy of Dentistry Today. | |
 | ||
| Figure 10 Retracted postcementation view of the smile. Reprinted courtesy of Dentistry Today. | ||
| Figure 11 Synchronized data of the right lateral excursion before any adjustment. Note that the contacts are group function. This pattern requires 31 mv of temporalis activity to perform the lateral excursion. | Figure 12 Synchronized data of the right lateral excursion after adjustment. Note that the contact is indicative of canine disclusion. This pattern only requires 11 mv of temporalis activity to perform. | |
| Figure 13 Synchronized data of the left lateral excursion before any adjustment. Note that the contacts are again representative of group function. This pattern requires 30 mv of temporalis activity to perform the lateral excursion. | Figure 14 Synchronized data of the left lateral excursion after adjustment. Note that the contact is indicative of canine disclusion. This pattern only requires 8 mv of temporalis activity to perform. | |
| About the Author | ||
 Chris Stevens, DDS Chris Stevens, DDS Private Practice Sun Prairie, Wisconsin | ||




