Optimal Results in the Esthetic Zone with CAD/CAM Implant Abutments: A Patient Example
George F. Priest
Optimal implant results in the esthetic zone can be predictably achieved using customized, patient-specific abutments. Encode™, a computer-aided design and computer-aided manufacturing (CAD/CAM) implant-restorative system developed by 3i (Palm Beach Gardens, FL), uses a unique healing abutment with codes embedded in the occlusal surface. After an impression has been made of the healing abutment in place, an optical scanner reads the codes from a resultant cast to determine implant size, location, hex position, and soft-tissue levels. A patient-specific final abutment is then designed and milled in titanium alloy. The abutment margins closely follow gingival levels and the form is idealized, contributing to a more optimal emergence profile and gingival architecture. A gold-colored, titanium-nitride coating is available as an optional esthetic feature which enhances ceramic crown shades and imparts warmer hues through gingival tissues.
The Advantages of CAD/CAM
The goals of implant dentistry have evolved beyond the mere provision of secure function to encompass the achievement of natural-appearing restorations. Newly available techniques and implant components are advancing the ability of restorative dentists to deliver predictable esthetic outcomes. One such innovation is the shift from conventional stock and cast-custom abutments to patient-specific abutments produced through CAD/CAM.
The fabrication of implant restorative components using conventional clinical and laboratory techniques has been problematic for a number of reasons. Many dentists are not comfortable making implant-level impressions. As a result, they may avoid offering implants as a treatment alternative. Or, they may use time-consuming traditional techniques for preparing stock abutments intraorally. Those who are at ease placing implants and making implant-level impressions may be troubled by the limitations of the lost-wax casting technology, which is subject to significant inaccuracies.1-3
CAD/CAM implant abutments offer the advantages of both stock and laboratory-processed custom abutments without their associated disadvantages. Like cast custom abutments, CAD/CAM abutments are created for each individual patient and therefore have the potential to provide optimal peri-implant soft-tissue support, a prerequisite for achieving ideal esthetics.4,5 CAD/CAM abutments require no manipulation after they are machined, resulting in a more precise fit than was previously achievable.6 Moreover, because the CAD software assists the technician in creating the abutment design, this precision can be produced with great consistency.
Encode healing abutments incorporate facets on their occlusal surfaces which serve as a code to identify the implant platform diameter, the height of the healing abutment, the hex position of the implant, and the diameter of the emergence profile.7 By making an impression of the healing abutment after tissue maturation, the restorative dentist is able to capture this vital information without having to resort to a more challenging implant-level impression.
An optical scanner reads and translates the codes embedded in the healing abutments. This data is transferred to the CAD software, the implant abutments are virtually designed, and the CAM milling apparatus produces the final titanium abutments. The completed abutments are returned to the local laboratory for completion of the definitive prosthesis.
A titanium-nitride gold coating was recently introduced as an optional feature for Encode final abutments. The gold coloring provides two distinct esthetic benefits. A ceramic crown seated on this abutment retains a more natural color (avoiding the gray tones that are often present when a silver colored alloy abutment is used). A gold-colored abutment also imparts a warm hue through the gingival tissues.
The following patient example illustrates a maxillary anterior reconstruction with ceramic crowns on natural teeth and a single implant with a titanium nitride-treated Encode abutment.
Case Presentation
A 60-year-old woman presented with a recently avulsed right maxillary central incisor. The tooth crown had been temporarily bonded to the adjacent teeth. Unesthetic veneer restorations in the anterior maxilla and loss of papillae around the missing incisor were evident upon examination (Figure 1). A high smile line made correction of the gingival profile a necessity for patient satisfaction. A treatment plan was developed, which called for replacement of the missing tooth with an implant and a customized patient-specific abutment followed by ceramic restorations on the maxillary anterior teeth and the single implant.
Using a surgical guide provided by the restorative dentist, the implant surgeon placed a 4-mm X 15-mm Osseotite® implant (3i) and grafted the site with autogenous bone covered by an Ossix™ resorbable membrane (3i). After implant uncovering, a temporary cylinder was secured to the abutment with a Gold-Tite™ screw (3i) and prepared (Figure 2). A bis-acrylic implant-level provisional crown was placed on the temporary cylinder and contoured to aid in the development of the peri-implant sulcus (Figure 3). Soft-tissue profiles and tooth proportions were then carefully assessed. Existing crowns were clinically short relative to the tooth width. However, prominent display of the patient’s teeth and existing vertical overlap precluded increasing tooth length in the coronal direction. Instead, the patient was referred to a periodontist who performed crown-lengthening (Figure 4, Figure 5 , and Figure 6) to reduce the display of the gingiva and achieve tooth dimensions that were proportional to the provisional restoration. After an additional 10 weeks, healing was complete (Figure 7).
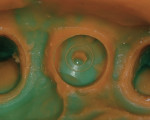
The restorative dentist prepared the remaining incisors and canines for ceramic crowns. The provisional implant restoration was removed, and an Encode healing abutment was placed (Figure 8 and Figure 9).An impression was then made using Fresh™ heavy- and light-bodied polyvinylsiloxane impression material (Exacta Dental Products, Clinton Township, MI). In making the impression, it was not necessary to pack a retraction cord around the abutment, in part because of the width of the sulcus shaped by the provisional restoration. This impression captured the codes embedded in the abutment (Figure 10). The restorative dentist also made a mandibular impression and an interocclusal record. The impressions and record were sent to the dentist’s local dental laboratory.
The laboratory poured the impression of the abutment with yellow die stone, then mounted the master and opposing cast on a semi-adjustable articulator. These casts were sent to 3i Implant Innovations, where the master cast was optically scanned, and the data were used to produce a computer model of the articulated casts. A 3i technician then designed a virtual abutment with a subgingival margin that conformed precisely to the patient’s soft-tissue contours (Figure 11). The model of the abutment was used to set a tool path to drive a milling machine that fabricated the final abutment from a solid blockof titanium alloy. This abutment was then coated with gold-colored titanium nitride to optimize the final appearance of the gingiva and the ceramic crown (Figure 12). 3i then returned the final abutment to the local laboratory.
Upon receipt of the final abutment from the laboratory, the restorative dentist secured it to the implant. A second impression was made of the prepared teeth and the final abutment (Figure 13), which allowed the ceramist to fabricate ceramic crowns on the abutment and prepared teeth concurrently (Figure 14, Figure 15, and Figure 16).
The local laboratory sent the crowns, final abutment, and a Gold-Tite abutment screw to the restorative dentist, who seated the final abutment on the implant, tightened the Gold-Tite screw to 35Ncm, and sealed the access opening (Figure 17). Complete seating of the abutment and ceramic crown was verified with a digital radiograph (Figure 18). Occlusion was refined, and the remaining ceramic crowns were seated and conventionally cemented (Figure 19).
Discussion
The primary challenge in this oral reconstruction was to create esthetic continuity between the natural teeth and the implant restoration. Implant placement in a well-developed site was the first step toward achieving normal soft- and hard-tissue results. Crown lengthening by the periodontist was essential to providing even gingival levels, reducing the gummy smile, and establishing ideal tooth proportions. A patient-specific CAD/CAM abutment provided ideal abutment form that optimally supported the peri-implant soft tissue. Finally, the titanium-nitride coating of the abutment allowed for continuity of color between the natural teeth and implant and imparted a warm gingival hue apical to the implant restoration.
Conclusion
The use of patient-specific computer-generated abutments offers several benefits. This technology significantly simplifies the impression-making process for the restorative dentist. It also eliminates the inaccuracies of casting technology, an important consideration in implant dentistry because the precision of components may affect implant longevity, prosthetic success, ease of restoration, and esthetic outcome. The use of CAD/ CAM technology also frees laboratory technicians from labor-intensive casting procedures, allowing them to instead concentrate on higher-level activities related to crown form and color. CAD/CAM patient-specific abutments have expanded the applicability of implants in the esthetic zone by contributing to ideal marginal abutment form and maximal peri-implant support. The additional benefits of titanium-nitride abutment coatings are superior shades of ceramic crowns and natural hues through the marginal tissues.
Disclosure
Dr. Priest is a 3i mentor, lecturer, and consultant for Implant Innovations, Inc. He also is a consultant and speaker for Exacta Products Inc. He did not receive financial remuneration for this article.
References
1. Gelbard S, Aoskar Y, Zalkind M, et al. Effect of impression materials and techniques on the marginal fit of metal casting. J Prosthet Dent. 1994;71(1): 1-6.
2. Vigolo P, Majzoub Z, Cordioli G. Measurement of the dimensions and abutment rotational freedom of gold-machined 3i UCLA-type abutments in the as-received condition, after casting with a noble metal alloy and porcelain firing. J Prosthet Dent. 2000; 84(5):548-553.
3. Hurson S. Laboratory techniques to prevent screw loosening on dental implants. J Dent Technol. 1996;13(3):30-37.
4. Papazian S, Morgano SM. A laboratory procedure to facilitate the development of an emergence profile with a custom implant abutment. J Prosthet Dent. 1998;79(2): 232-234.
5. Touati B. Biologically driven prosthetic options in implant dentistry. Pract Proced Aesthet Dent. 2004;16(7):517-520.
6. Byrne D, Houston F, Cleary R, et al. The fit of cast and premachined implant abutments. J Prosthet Dent. 1998:80:184-192.
7. Priest GF. Virtual-designed and computer-milled implant abutments. J Oral Maxillofac Surgery. 2005;63(suppl 2):22-32.
About the Author
George F. Priest, DMD
Private Practice (Prosthodontics)
Atlanta, Georgia