Implications of Implementing the ALARA Principle and NCRP Guidelines: How They Affect Your X-ray Procedures
David N. Wright, DMD
The ALARA Principle (which stands for As Low as Reasonably Achievable) is an integral component of the new National Council on Radiation Protection and Measurements (NCRP) Guidelines for Radiation Protection. The suggestions for implementation provided in this article will help you to do the following: Comply with a major part of the new Guidelines that deal directly with radiation exposure issues to staff and patients; provide a safer practice environment for you and your staff/patients by significantly reducing radiation exposure; and give you more “readable” x-rays in the process.
The NCRP issued a new set of guidelines, Radiation Protection in Dentistry,1 in 2003, supplanting the previous Guidelines that were issued in 1970, stating that dentists are obligated to follow the ALARA Principle and are required to implement it in their practices.
Providing even more incentive to follow these Guidelines, recent studies on the development of cancer from long-term, cumulative low doses of ionizing radiation also strongly suggest that dentists seriously review their radiographic procedures and make every attempt to lower even further the radiation exposure to staff and patients.
IMPLEMENTATION RECOMMENDATIONS
Because dentists have a moral as well as what could soon be a legal obligation to keep radiation exposure to their patients and staff as low as reasonably achievable, and to thereby conform to the new NCRP radiation guidelines, it is recommended that the following steps be taken as soon as possible:
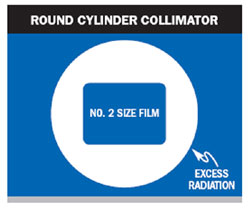
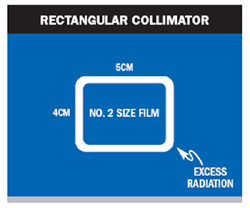
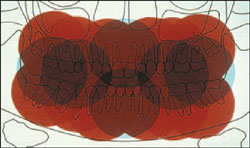
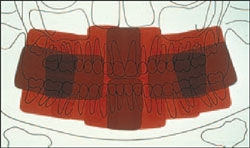
- Replace all round x-ray collimators (cones) with rectangular collimators. This is required under the new Guidelines to “reduce the effective dose to the patient by a factor of four to five, without adverse influence on image quality.”1p19,38 The new Guidelines concerning collimators are very strict: “Rectangular collimation of the x-ray beam shall be routinely used for periapical radiography. Each dimension of the beam, measured in the plane of the image receptor, should not exceed the dimension of the image receptor by more than two percent of the source-to-image receptor distance. Similar collimation should be used, when feasible, for interproximal radiography. Anatomy or the inability of occasional specific patients to cooperate, including some children, may make rectangular collimation and beam-receptor alignment awkward or impossible for some projections. The requirement may be relaxed in these rare cases.”1p21 Figures 1, Figure 2, Figure 3, Figure 4 show the difference in radiation patterns experienced by your patients from the 2 cones.
- To use the fastest image receptors available, eg, using “F” speed film, which would reduce the dose by 20% compared to “E” speed film.1p21,22
- To shield patients with a leaded apron, unless all requirements in the NCRP Report 145 are met. It is now required that all children wear a thyroid shield. Adults should be provided with a thyroid shield “when it will not interfere with the examination.”1p26,27
- To require that personal dosimeters be worn and monitored by all known pregnant employees who work around x-ray equipment when it is being used. Personal dosimeters are commercially available from a number of sources.1p31,32
- To require that shielding design be incorporated in all new dental office construction, and to require certification by pertinent existing state regulatory departments. Two statements are worth quoting: “Shielding design for new offices shall provide protective barriers for the operator. The barriers shall be constructed so operators can maintain visual contact and communication with patients throughout the procedures...in the absence of a barrier in an existing facility the operator shall remain at least 2 M from the tube head during exposure. If the 2 M distance cannot be maintained, then a barrier shall be provided.”1p27-29
- Although not required, going to digital imaging is also a very viable way to follow the ALARA principle, as patient/staff exposure is reduced.1p88
Steps 2 through 6 are self-explanatory and easily understood. Referring to the sources cited for further information may be helpful. Step 1, regarding collimators, requires further discussion.
Many dental schools teach their students how to use rectangular collimation, and they cite the reduction of radiation as the major reason for using these collimators. The major issue that students face using these collimators, however, is frequent “cone-cutting” because of the reduced size of the x-ray beam. Film positioning devices are essential to reduce the incidence of cone-cutting. These, along with rectangular collimators, are available through distributors. Proper use of these devices “produces more accurate images in terms of minimizing inaccurate relationships of one structure to another, foreshortening, elongation, distortion and the overlap of structures such as the contact points” (Figure 5).1p21,22 In addition, rectangular collimation provides for increased contrast and clarity of x-rays. Reduction of scatter radiation reduces unwanted and non diagnostic scattered photons of radiation to the image, and this in turn reduces the degradation in the inherent image quality, thereby increasing the contrast. “This added bonus of rectangular collimation applies equally to both film and all types of digital sensors.”1p21,22
A new, unique product, manufactured by Interactive Diagnostic Imaging, makes the task of taking good x-rays with a rectangular collimator almost fool-proof. Called the Tru-Align Positioning System, it consists of a rectangular collimator that will retrofit most existing x-ray heads currently in use. Attached to the end of the rectangular cone is a unique magnetized ring that, when it is aligned properly, precisely fits the magnetized outer end of the included image receptor/film holder. When the beam is perfectly aligned with the digital image receptor or film, the magnets connect and signal the true alignment, and the x-ray can now be taken, without concern for cone-cutting (Figure 6).
CONCLUSION
The new Guidelines for Radiation Protection are quite imposing to implement all at once. In the author’s experience, it is much easier to tackle them one at a time, starting with the easiest and most beneficial ones first. Replacing circular cones with rectangular cones is a very effective and simple way to reduce radiation exposure of patients and staff, and it also helps to produce more readable x-rays. However, at least one circular cone should be saved for the “rare patient” who will require its use.
DISCLOSURE
Dr. Wright currently serves on the National Clinical Advisory Council for Kuraray Corporation.
REFERENCE
1. National Council on Radiation Protection and Measurements. Radiation protection in dentistry. Report No. 145. NRCP Publications, Bethesda, Md. 2003. Available at https://www.ncrponline.org/pubs.html.
 |
 |
||||
| Figure 1 Round collimator target image showing large zone of excess radiation. | Figure 2 Rectangular collimator target image showing small zone of excess radiation. | ||||
 |
 |
||||
| Figure 3 Overlapping radiation fields with circular collimation, maximum 4 fields. | Figure 4 Overlapping radiation fields with rectangular collimation, maximum 6+ fields. | ||||
 |
 |
||||
| Figure 5 Current film positioning devices. | Figure 6 The TruAlign System showing the rectangular collimator and magnetized film/sensor positioning device. | ||||
|
|||||




