The Team: The Restorative Dentist–Periodontist Partnership
In this era of rapidly changing healthcare options, there has never been a more critical time for dentists to embrace a team approach to care. Every day, more than 8,000 people in the United States turn 65, and in the coming years, the population age 65 years and older will double from 35 million to over 70 million. Life-span has increased dramatically since 1900, when the average life expectancy in the United States was slightly over 48 years, and the leading causes of death were pneumonia, tuberculosis, and dysentery. In contrast, life expectancy today is over 77 years,1 and infection has been eliminated as a major cause of death. As life expectancy increases, chronic diseases of aging are replacing acute diseases of infection. Most of these diseases have a strong association with inflammation, a condition to which an individual may be genetically predisposed.2 In a report released this year, it was estimated that up to one-third of all cancers may be related to chronic systemic inflammation.3 No longer a country whose population dies at a relatively young age, the United States is now populated by people who, in increasing numbers, experience more chronic diseases for which they are taking more medications than ever before. In addition, many of those in the now-aging generation not only seek to live longer lives, they strive to maintain high-quality, active lives that are not restricted by function or esthetics.4
However, 30% of Americans are either diabetic or prediabetic, and most of these people will die of a cardiovascular event.5 A review of the medical histories of diabetic patients reveals that most, if not all, are on lipid-reducing and cardiac medications. These individuals show measurable increases in circulating inflammatory mediators such as C- reactive protein and tumor necrosis factor, exhibiting a proinflammatory state. It is well-documented that there is a significant relationship between obesity, circulating tumor necrosis factor, diabetes, and periodontal diseases.6 Data on patients with heart disease indicate that many who exhibit a cardiovascular event have normal or below normal cholesterol levels and lipid levels; they do not exhibit the classic cardiovascular risk factors.7 As they age, these patients may be genetically predisposed to the production of inflammatory mediators, which are indicators of disease risk8 (Figure 1). These inflammatory mediators can be produced from a number of body systems, including the periodontium.9,10 Patients who have high concentrations of these inflammatory mediators also exhibit a proinflammatory state.
Because periodontal diseases have an inflammatory response associated with the bacterial accumulation of plaque, plaque has been equated with disease.11 Previously, there were only two explanations for demonstrated disease progression: either the patient failed to perform plaque control adequately; or the dental team failed to perform subgingival debridement adequately. This was the simple explanation, but it was not complete. The correlation between plaque and disease is quite strong in gingivitis, but it begins to break down with periodontitis. Not all gingivitis progresses to periodontitis, and the severity of periodontitis is not dependent upon the amount of plaque.12,13 It is now known that a subset of the population—people with a genotype that favors the production of the inflammatory mediator interleuken—are more likely to develop severe periodontitis when faced with a bacterial challenge than those who do not carry this gene.14 These individuals exhibit the same proinflammatory potential that is found in those with other chronic diseases of agingFigure 2).
An examination of patients with high bone loss scores associated with moderate-to-severe periodontitis reveals that this population has a significantly increased risk of suffering a cardiovascular event.15 The presence of circulating inflammatory mediators—which are found in patients with periodontal or cardiovascular disease—are an indication of disease risk. This is the essence of the perio-systemic link, which focuses not only on the presence of disease, but the risk of future disease and its impact on the rest of the body.16,17 While there are not yet any interventional studies showing causality with regard to periodontal diseases and other chronic inflammatory diseases of aging, it may be said that overall excellent health cannot coexist with periodontal disease. Periodontal health should be considered an essential part of overall health and well-being. These correlations are apparent as well to those outside of dentistry. The American Journal of Cardiology has collaborated with the American Academy of Periodontology (AAP) in exploring this issue, and the American Diabetes Association, as well as the World Health Organization, have both expressed interest in working with the AAP to further define the role of inflammation in periodontal disease and its relationship to systemic health. The significance of this major dental disease is certain to command much more public attention in the near future.
A major focus in both medicine and dentistry is control of inflammatory burden and managing patient risk. However, patient expectations have changed: Those with soft and hard tissue loss are no long satisfied with having their disease controlled; they want to be restored to predisease levels.18 Advances in periodontal regeneration have changed the rules of the game in periodontal treatment planning (Figure 3 and Figure 4). The addition of growth factors and biologic mediators applied at surgery—either alone, or in combination with bone grafts—have provided the ability to restore large amounts of periodontal ligament, bone, and cementum, and to predictably restore the health, function, and esthetics of patients. Periodontists are able to save more teeth than ever before.19-22
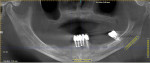
Even furcation involvements, when addressed appropriately, can offer long-term success23 (Figure 5 and Figure 6). The concept of tissue regeneration has expanded to soft tissue and coverage of exposed root surfaces, which as patients age, becomes increasingly difficult to manage from a strictly restorative perspective (Figure 7 and Figure 8). Also, as this population—whose demands on restorative outcomes is quite high—ages, periodontists and restorative dentists need to find ways to work together to provide a framework of healthy, functional hard and soft tissue to support the best outcomes (Figure 9 and Figure 10). These concepts of regeneration have been adapted to framing implants and their restorations, which look more like teeth and less like prosthetic replacements (Figure 11). As advancements in tissue regeneration continue to emerge, those individuals for whom periodontal therapy is not possible can once again function in a manner consistent with long-term health and well-being, both from a periodontal and psychosocial perspective (Figure 12 and Figure 13).
However, it is important to remember that implants are man-made, and they are not impervious to disease. Periodontists are increasingly called upon to manage peri-implantitis and other hard and soft tissue complications. Dental implants require careful monitoring and ongoing maintenance. Not infrequently, management of these complex conditions requires close cooperation between the periodontist and the restorative dentist (Figure 14).24
Take-Home Messages
It can be said that periodontists have the most extensive literature base in dentistry on the diagnosis and management of periodontal disease and dental implants. However, they need to communicate their knowledge with the rest of the dental community. They also need to listen to those in the dental community to determine what their needs are. It is incumbent upon periodontists to lead the conversation with restorative dentists, who are the primary caregivers in this country, the ones who treat most of the periodontal disease. Periodontists should provide them with the evidence-based tools they need to better diagnose, assess, and manage patient risk.
Restorative dentists and periodontal specialists can work as partners to manage their own risk as well as that of their patients. Together, they can maximize the success of their professional lives, and provide lifelong periodontal health and well-being to patients who require their skills. As treatment teams, they are responsible for determining how and when to act, and on which patients. This is best developed with a one-on-one dialogue. Communication and commitment are the keys to success.
Dentistry plays an ever-increasing role in the lives of people. The hope is that clinicians can return to their practices with a renewed enthusiasm about their profession and an eagerness to enhance their knowledge and skills. That enthusiasm, that excitement for the future, that dedication to their patients is apparent in all they do—it energizes their staffs, and gives their patients the confidence to pursue what is possible and to be active participants in their care.
Ultimately, the team approach is about trust. There is the trust of patients that their clinician will place their benefit above his/her own, which is why dentists rank among the most trusted in health professionals. There is also the trust between periodontists and restoring colleagues who, working together, are well-positioned to help a long-living and demanding population achieve its desire for lifelong health and well-being.
Acknowledgments
The author would like to thank the restorative team members: Thomas Thompson, DDS; George Perri, DDS; Terence Kilker, DDS; Michael Crial, DMD; and Greg Kuwabara, DDS.
References
1. US Census Bureau. Population Division 2011. https:///www.census.gov. Accessed March 1, 2011.
2. Wilson AG. Epigenetic regulation of gene expression in the inflammatory response and relevance to common diseases. J Periodontol. 2008;79(8 Suppl):1514-1519.
3. Tili E, Michaillie J, Adler H, et. al. Mutator activity induced by microRNA-155 (miR-155) links inflammation and cancer. Proc Natl Acad Sci U.S.A. 2011;108(12):4908-4913.
4. Eiseman B. When blue turns gray: postwarranty performance. Am J Geriatr Psychiatry. 2006;14(1):21-26.
5. American Diabetes Association. https://www.diabetes.org. Accessed March, 2011.
6. Meisel P, Wilke P, Biffar R, Holtfreter B, Wallaschofski H, Kocher T. Total tooth loss and systemic correlations of inflammation: role of obesity [published online ahead of print July 14 2011]. Obesity. 2011.
7. Blankstein R, Budoff MJ, Shaw LJ, et al. Predictors of coronary heart disease events among asymptomatic persons with low low-density lipoprotein cholesterol. J Am Coll Cardiol. 2011;58(4):364-374.
8. Ridker PM, Koenig W, Kastelein JJ. C-reactive protein in the Heart Protection Study. Lancet. 2011;377(9781):1918.
9. Kaptoge S, Di Angelantonio G, Lowe G, et al. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet. 2010;375(9709):132-140.
10. Preshaw PM, Taylor JJ. How has research into cytokine interactions and their role in driving immune responses impacted our understanding of periodontists?J Clin Periodontol. 2011;38(Suppl 11):60-84.
11. Graves DT, Li J, Cochran DL. Inflammation and uncoupling as mechanisms of periodontal bone loss. J Dent Res. 2011;90(2):145-153.
12. Löe H, Theilade E, Jensen SB. Experimental gingivitis in man. J Periodontol. 1965;36:177-187.
13. Löe H, Anerud A, Boysen H, Morrison E. Natural history of periodontal disease in man. Rapid, moderate and no loss of attachment in Sri Lankan laborers 14 to 46 years of age.J Clin Periodontol. 1986;13(5):165-174.
14. Axelsson P. Role of genetic and hereditary factors. In: Diagnosis and Risk Prediction of Periodontal Diseases. Chicago, IL: Quintessence Publishing Co; 2002:146-163.
15. McDevitt MJ, Wang HY, Knobelman C, et al. Interleukin-1 genetic association with periodontitis in clinical practice. J Periodontol. 2000;71(2):156-163.
16. Beck J, Garcia R, Heiss G, Vokonas PS, Offenbacher S. Peridontal disease and cardiovascular disease. J Periodontol. 1996;67(10 Suppl):1123-1127.
17. Scannapieco FA, Bush RB, Paju S. Associations between periodontal disease and risk for atherosclerosis, cardio-vascular disease, and stroke. A systematic review.Ann Periodontol. 2003;8(1):38-53.
18. Nesse W, Dijkstra PU, Abbas F, et al. Increased prevalence of cardiovascular and autoimmune diseases in periodontitis patients: a cross sectional study. J Periodontol. 2010;81(11):1622-1628.
19. Smith JO, Aarvold A, Tayton ER, Dunlop DG, Oreffo RO. Skeletal tissue regeneration: Current approaches and novel reconstructive strategies for an aging population [published online ahead of print June 30 2011]. Tissue Eng Part B Rev.
20. Bowers GM, Schallhorn RG, Mellonig JT. Histologic evaluation of new attachment in human intrabony defects. J Periodontol. 1982;53(8):509-514.
21. Heijl L, Heiden G, Svärdström G, Ostgren A. Enamel matrix derivative (EMDOGAIN) in the treatment of intrabony defects.J Clin Periodontol. 1997;24(9 Pt 2):705-714.
22. Froum SJ, Weinberg M, Rosenberg E, Tarnow D. A comparative study utilizing open flap debridement with and without enamel matrix derivative in the treatment of periodontal intrabony defects. A 12-month re-entry study. J Periodontol. 2001;72(1):25-35.
23. Gurinsky BS, Mills MP, Mellonig JT. Clinical evaluation of demineralized freeze-dried bone allograft and enamel matrix derivative versus enamel matrix derivative alone in the treatment of periodontal osseous defects in humans. J Periodontol. 2004;75(10):1309-1318.
24. Bowers GM, Schallhorn RG, McClain PK, Morrison GM, Morgan R, Reynolds MA. Factors influencing the outcomes of regenerative therapy in mandibular Class II furcations. J Periodontol. 2003;74(9):1255-1268.
25. Heasman P, Esmail Z, Barclay C. Peri-implant diseases. Dent Update. 2010;37(8):511-526.
About the Author
Donald S. Clem, III, DDS
President, American Academy of Periodontology
Private Practice
Fullerton, California