CAD/CAM Solutions for Minimally Invasive All-Ceramic Rehabilitation of Extended Erosive Lesions
Petra C. Guess Gierthmuehlen, DDS; and Enrico Steger, MDT
Abstract: Dental erosion is a global oral health problem that can lead to significant functional and esthetic impairments of the affected patients. Treatment of severe cases with augmented loss of the vertical dimension of occlusion (VDO) represents a challenge for both the dental team and the patient. CAD/CAM technology was used in the presented case to analyze the interocclusal space. Based on a virtual wax-up of the final restorations, CAD/CAM-fabricated preparation splints served as a guide and ensured a most minimally invasive preparation design. Milled polymer provisionals enabled the patient to visualize the final treatment outcome and served as a fracture-resistant temporary restoration to test the increased VDO. Monolithic lithium-disilicate ceramic, defect-oriented restorations with reduced ceramic thickness enabled a functional and reliable reconstruction of the severely compromised dentition. This case report documents a practical, digital approach and discusses the advantages related to treatment time, ease of treatment, and predictability.
Along with dental caries and periodontal disease, dental erosion is recognized as a global public oral health problem. Several factors related to extrinsic erosions, such as the consumption of acidic foods and beverages, medicines, and lifestyle changes, are reported in the literature.1 Moreover, gastroesophageal reflux disease (GERD) and eating disorders are common intrinsic causes of erosion. Occurrence of dental erosion as well as the degree of its severity have increased significantly during the past several years. Various epidemiologic studies have shown a wide-ranging prevalence between 4% to 82% in adults aged 18 to 88 years2 and 17.7% to 54.4% in young adults (aged 18 to 35 years), with a large difference between the investigated European countries.3 The prevalence of dental erosion is considerably higher in studies investigating younger individuals compared with those in older age groups.
Dental erosion represents a serious problem for the patient, especially if the disease is diagnosed at an advanced stage. Hypersensitivity, pain, pulpal inflammation, necrosis, and periapical pathology are possible complications. The prevalence of severe dentin hypersensitivity in young adults is high (28.4%), and a strong, progressive relationship between dentin hypersensitivity and erosive tooth wear has been reported.4 In addition, extended erosion leads to esthetic impairment, because it is correlated with significant shortening of the maxillary incisors. The patient’s physiognomy is often changed when advanced lesions cause a significant loss of vertical dimension of occlusion (VDO) in the lower face. Furthermore, the mechanical properties of the hard tissues of the affected teeth are weakened by the acid demineralization. The microhardness of enamel and dentin is significantly decreased, rendering the dental hard tissue susceptible to physical wear.5
Until recently, severe erosive tooth wear could be addressed only with extensive crown-and-bridge reconstructions or, in advanced stages, with removable dentures. These conventional procedures—including full-coverage crowns—frequently involved elective endodontic therapy, crown-lengthening procedures, and major additional loss of tooth structure.6,7 Novel treatment approaches for extended erosive lesions aim to be as minimally invasive as possible in an effort to preserve the maximum amount of remaining tooth structure. Advancements in all-ceramic and adhesive technologies enabled the development of innovative defect-oriented treatment concepts for restoring compromised dentition. Modified onlay and full-veneer preparation geometries have evolved to form a reliable alternative to conventional full-coverage crowns.8 Nonretentive preparation designs in combination with reduced restoration thicknesses allow for a minimally invasive treatment approach. Moreover, CAD/CAM technologies for the fabrication of metal-free, tooth-colored restorations are increasingly used in prosthetic dentistry.
In cases of severe erosive decay, the VDO needs to increase. In the past decade, this was accomplished with a conventionally manufactured wax-up that the dental technician would fabricate. The transfer of this desired diagnostic tooth arrangement to the mock-up, provisionals, and permanent restorations is a time-consuming and costly effort, and may be inaccurate. Innovative manufacturing technologies and new materials, such as millable polymer and wax blocks for CAD/CAM, offer novel treatment options. Limited information is available regarding these treatment concepts for patients with severe erosive tooth wear.
Case Report
The treatment sequence of the aforementioned minimally invasive approach using CAD/CAM technology and monolithic all-ceramic restorations is demonstrated in the following presented case. Discussion is based on clinically relevant scientific data.
Initial Findings
A 26-year-old male with an unremarkable medical history presented with a chief complaint of hypersensitivity, severe tooth wear, severe loss of VDO, and unesthetic maxillary anterior teeth (Figure 1 and Figure 2). He requested a full-mouth rehabilitation to address the extensive tooth structure loss and reduced VDO. The patient admitted to excessive consumption of soft drinks, and the erosive tooth wear was attributed to the high intake of acidic beverages, including energy drinks. Intrinsic causes of erosive lesions, such as eating disorders and GERD, for which the patient was evaluated, were excluded. After analysis of dietary habits, the patient completely stopped the consumption of acidic drinks.
Clinical examination findings revealed group guidance and a significant loss of VDO. Severe loss of enamel and dentin was mainly located in the palatal aspect of the anterior and posterior teeth (Figure 3 and Figure 4). The patient’s oral hygiene was good, and no signs of temporomandibular disorder or pain were evident. Diagnostics included clinical, periodontal, functional, and radiologic examinations and an esthetic analysis. The periodontal findings revealed no bleeding on probing or any clinical attachment losses.
Treatment Planning and Clinical Procedures
In addition to providing the patient with diet education and oral hygiene instruction, initial treatment consisted of removing the impacted third molars, treating the caries, and replacing the insufficient composite restorations. The anticipated alteration of VDO aimed to consider esthetic parameters and avoid acceptance problems or orthodontic intrusion. The initial esthetic analysis for the diagnostic tooth arrangement included an incisal extension of the maxillary incisors with closure of the spacing. Comprehensive photography was used to determine the occlusal/incisal planes and prosthetic space, as well as to communicate the findings to the dental technician. Maximum occlusion was registrated. Maxillary and mandibular impressions were taken with a polyether impression material (Impregum™, 3M ESPE, www.3MESPE.com) and conventional impression trays.
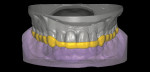
The casts were mounted on the articlulator and digitized in a laboratory scanner (S600 ARTI Zirkonzahn, www.zirkonzahn.com) (Figure 5 and Figure 6). The dental technician performed a digital tooth arrangement/virtual wax-up, rebuilding the occlusal aspects of the molar and premolar regions, as well as the incisors and canines at an increased VDO. The prospective restorations’ tooth positions, lengths, sizes, and shapes were determined. This digital setup served as a template for the entire treatment. The initial situation and prospective tooth design were digitally overlapped to analyze interocclusal spacing. Based on this analysis, a splint was designed encoding the areas where occlusal reduction was necessary (Figure 7 through Figure 9). Subsequently, the splint was milled (M5 Heavy Milling Unit, Zirkonzahn) to transfer this information to the patient’s mouth. The virtual wax-up was also used to produce CAD/CAM-fabricated eggshell temporaries (TEMP Basic, Zirkonzahn) (Figure 10). The models, splints, and temporaries were sent to the dental office and tested intraorally (Figure 11).
This full-arch mock-up arrangement was used to evaluate whether the amount of VDO correction would be acceptable for the patient and, also, whether the tooth arrangement would meet his esthetic and functional expectations. After the patient approved the mock-up, the minimally invasive preparation was performed with the CAD/CAM splints in situ (Figure 9). Sharp edges on the occlusal surfaces caused by the erosive decay were rounded. A very shallow buccal chamfer preparation (0.5 mm) was performed on the maxillary anterior and premolar teeth; no preparation was needed on the palatal aspects due to the erosive tooth structure loss (Figure 12). The mandibular anterior teeth received a veneer preparation. The abutment teeth were temporarily restored with the CAD/CAM-generated polymer-based restorations (Figure 13).
After the patient wore the provisional for 6 weeks, conventional impressions (Identium®, Kettenbach, www.kettenbachusa.com) of the abutment teeth were acquired. A cross-mounting bite registration was performed, and the mounted models were then digitized with the laboratory scanner (Figure 14 and Figure 15). The initial lodged virtual wax-up was then used again to design the final restorations (Figure 16 through Figure 18). The restorations were subsequently milled in CAD wax in the 5-axis milling unit and, finally, pressed in a lithium-disilicate glass ceramic (IPS e.max® Press, Ivoclar Vivadent, www.ivoclarvivadent.com) (Figure 19). The monolithic all-ceramic restorations were polished and subsequently characterized with surface stains. All lithium-disilicate glass-ceramic restorations were adhesively luted under rubber dam isolation using a dual-polymerizing composite cement (Variolink® II, Ivoclar Vivadent) following the manufacturer’s protocol. A stable static occlusion and a dynamic occlusion with incisal/canine guidance were obtained (Figure 20 and Figure 21). Finally, the patient was provided with a CAD/CAM-fabricated occlusal splint (Temp Premium Flexible Transpa, Zirkonzahn) to facilitate long-term success (Figure 22 and Figure 23).
Intraoral photographs taken at a 1.5-year recall confirmed a stable occlusion, healthy periodontal status, and no marginal staining or plaque accumulation. No caries at the restoration margins or signs of fractures within the restorations were observed (Figure 24 through Figure 26).
Discussion
A key disadvantage of the traditional approach commonly used to treat patients with substantial erosive lesions is the extensive tooth preparation required for conventional crowns.6,7 In particular, the reduced crown height of eroded teeth complicates prosthodontic treatment, because it means there is less remaining tooth structure, which is needed for retention. The extensive removal of tooth structure during conventional crown therapy often results in endodontic treatment and can compromise the long-term survival of the dentition, which is especially relevant when patients are relatively young. In contrast, adhesive restorations represent a more conservative treatment approach, reducing the need for preparation. Superficial preparation of the eroded tooth structure with diamond burs is recommended to ensure adequate surface roughening to enable reliable long-term bonding.9
Data on the performance of composite restorations in patients with severe erosive tooth wear are scarce and contradictory. Recent data are available only in case reports, case series,10 and a retrospective clinical study,11 but they document favorable mid-term results (3.98-year and 5.5-year survival rates of 93.1% and 99.2%, respectively) for adhesively bonded direct composite restorations. However, these chairside treatments using direct composites are time consuming and highly dependent on the operator’s skills. Moreover, deterioration with respect to marginal quality, marginal discoloration, surface texture, and anatomic form was observed. Hence, novel CAD/CAM composite-based material systems, such as resin nanoceramic and hybrid ceramics with enhanced wear resistance and mechanical properties, were developed in an effort to improve the long-term performance of extended restorations for erosive lesions in the load-bearing area. No scientific evidence, however, is available on these materials for the restoration of erosive wear.
Another minimally invasive treatment approach uses palatal indirect composite restorations and facial feldspathic ceramic veneers to restore anterior teeth with severe erosion. While this concept showed favorable results (100% 4-year survival rates) in a prospective clinical study, to date it has been implemented in only one study center; therefore, the success of its use in general remains unclear.12
All-ceramic restorations have a long history of clinical success in minimally invasive rehabilitation of the anterior and posterior dentition. For restoration of carious lesions, promising outcomes are reported for minimally invasive crowns (99.01% 3-year survival rates)13 and posterior restorations (97% to 100% 7-year survival rates).14 To the authors’ knowledge, no prospective, randomized clinical study on erosive lesions has yet been reported in the dental literature.
In the present case, conventional impressions were made, as only limited data are available regarding the precision of full-arch scans.15 Inaccuracies, distortions, and horizontal deviations have been reported in laboratory studies, particularly in the distal portions of the data sets.16
Emerging advantages of the digital technique described in this case report include reduced treatment time and a shorter manufacturing process. The predictability of the final treatment can also be enhanced because of the easy transfer from the planning to the definitive restoration. The virtual diagnostic tooth arrangement was used to manufacture the preparation splints as well as the temporary and permanent restorations, and it needed to be made only once. Moreover, it could be replicated and easily modified. Hence, the treatment was concluded in fewer appointments. The implementation of computer technology allowed for the expectation of highly predictable, precise, reliable restorations. The application of CAD wax enabled the machinability of thin margins of the minimally invasive restorations with a CAD/CAM milling device. The digital approach ensured a cost- and time-effective workflow. Consequently, this method could make the comprehensive treatment of erosive decay accessible to a wider patient population.
Conclusion and Clinical Significance
Defect-oriented adhesive monolithic restorations with reduced ceramic thicknesses represent an esthetic, functional, and minimally invasive treatment option for the rehabilitation of complex cases with erosive defects. In this case, the application of CAD/CAM technology efficiently facilitated treatment planning and restoration fabrication and provided the clinician with guidelines to successfully implement the presented minimally invasive treatment concept. The virtual wax-up, milled preparation splints, CAD/CAM provisionals, and wax patterns of the final lithium-disilicate ceramic restorations provided for a highly predictable and esthetic treatment outcome that was achieved in a timely and cost-effective manner. Long-term clinical studies on the performance of this CAD/CAM workflow are needed.
Disclosure
Enrico Steger, MDT, is founder and CEO of Zirkonzahn GmbH.
About the Authors
Petra C. Guess Gierthmuehlen, DDS
Professor and Chair
Department of Prosthodontics
School of Dentistry
Heinrich-Heine University
Düsseldorf, Germany
Enrico Steger, MDT
Dental Laboratory Steger
Bruneck, Italy
Founder and CEO
Zirkonzahn GmbH, Gais, Italy
References
1. Barbour ME, Lussi A. Erosion in relation to nutrition and the environment. Monogr Oral Sci. 2014;25:143-154.
2. Jaeggi T, Grüninger A, Lussi A. Restorative therapy of erosion. Monogr Oral Sci. 2006;20:200-214.
3. Bartlett DW, Lussi A, West NX, et al. Prevalence of tooth wear on buccal and lingual surfaces and possible risk factors in young European adults. J Dent. 2013;41(11):1007-1013.
4. West NX, Sanz M, Lussi A, et al. Prevalence of dentine hypersensitivity and study of associated factors: a European population-based cross-sectional study. J Dent. 2013;41(10):841-851.
5. Lussi A, Jäggi T, Schärer S. The influence of different factors on in vitro enamel erosion. Caries Res. 1993;27(5):387-393.
6. Edelhoff D, Sorensen JA. Tooth structure removal associated with various preparation designs for anterior teeth. J Prosthet Dent. 2002;87(5):503-509.
7. Edelhoff D, Sorensen JA. Tooth structure removal associated with various preparation designs for posterior teeth. Int J Periodontics Restorative Dent. 2002;22(3):241-249.
8. Guess PC, Schultheis S, Wolkewitz M, et al. Influence of preparation design and ceramic thicknesses on fracture resistance and failure modes of premolar partial coverage restorations. J Prosthet Dent. 2013;110(4):264-273.
9. Zimmerli B, De Munck J, Lussi A, et al. Long-term bonding to eroded dentin requires superficial bur preparation. Clin Oral Investig. 2012;16(5):1451-1461.
10. Attin T, Filli T, Imfeld C, Schmidlin PR. Composite vertical bite reconstructions in eroded dentitions after 5.5 years: a case series. J Oral Rehabil. 2012;39(1):73-79.
11. Hamburger JT, Opdam NJ, Bronkhorst EM, et al. Clinical performance of direct composite restorations for treatment of severe tooth wear. J Adhes Dent. 2011;13(6):585-593.
12. Grütter L, Vailati F. Full-mouth adhesive rehabilitation in case of severe dental erosion, a minimally invasive approach following the 3-step technique. Eur J Esthet Dent. 2013;8(3):358-375.
13. Cortellini D, Canale A. Bonding lithium disilicate ceramic to feather-edge tooth preparations: a minimally invasive treatment concept. J Adhes Dent. 2012;14(1):7-10.
14. Guess PC, Selz CF, Steinhart YN, et al. Prospective clinical split-mouth study of pressed and CAD/CAM all-ceramic partial-coverage restorations: 7-year results. Int J Prosthodont. 2013;26(1):21-25.
15. Ender A, Mehl A. In-vitro evaluation of the accuracy of conventional and digital methods of obtaining full-arch dental impressions. Quintessence Int. 2015;46(1):9-17.
16. Patzelt SB, Emmanouilidi A, Stampf S, et al. Accuracy of full-arch scans using intraoral scanners. Clin Oral Investig. 2014;18(6):1687-1694.