3-D Interdisciplinary Communication: Intermediate Restorative Measures to Enhance Esthetic Outcomes
Brad Jones, DDS; Richard D. Roblee, DDS
Abstract: Dental esthetics serves as the starting point of current diagnosis and treatment planning philosophy. In complex interdisciplinary cases in which anterior tooth structure is compromised and requires restoration, the team must have a precise means of communicating the eventual shape and dimensions of the anterior teeth before final orthodontic positioning and bracket removal and certainly prior to final restorations. Relying on the treating orthodontist’s “educated guess” for the correct spatial relationships of the anterior teeth unfairly burdens him or her and ultimately risks the esthetics and longevity of the restorations. An effective means of communication between the restorative dentist and orthodontist is available 3-dimensionally through the use of intermediate restorative procedures while the patient is in orthodontic appliances and before final tooth movements. Several cases illustrate techniques used to accomplish this with great efficiency, providing the patient a relatively low-cost treatment that enhances esthetics both during treatment and in the final outcome.
Numerous, complex problems influence anterior dental esthetics. The most common include tooth-size discrepancies caused by various factors, such as small lateral incisors, excessive incisal wear of anterior teeth with accompanying dentoalveolar extrusion, chemical erosion of enamel (eg, bulimia), congenitally missing teeth (eg, oligodontia), damaged or missing teeth because of trauma or disease, or tooth-mass-to-arch length irregularities. The restorative dentist often has the tools necessary to resolve these issues, provided the teeth occupy the proper position in the arch relative to each other and within the framework of the smile. When the teeth need repositioning and there is inadequate room to restore prior to orthodontics,1 the orthodontist proves invaluable in the interdisciplinary process.2,3 At the diagnostic and treatment planning stages, the team determines the restorative plan for each tooth prior to initiation of orthodontics.2,3 The next necessary step involves the precise communication between team members as to positioning of the teeth. In complex cases, this discussion may occur best as an intermediate restorative measure during orthodontic treatment, thereby providing a “3-dimensional” spatial guide to the orthodontist before finishing the set-up. Using such a method introduces a degree of predictability that is otherwise unachievable. This article explores several techniques that facilitate this process in complex cases.
Incisal Wear and Dentoalveolar Extrusion
Perhaps one of the most common yet complex cases involves severe wear of the incisal edges of anterior teeth. When a parafunctional habit exists,4 incisal wear develops to varying degrees depending on the malocclusion (Figure 1A) and the patient’s age. Accompanying the wear is the often underappreciated dentoalveolar extrusion of the teeth,5 resulting in short and unesthetic anterior teeth with irregular gingival margins (Figure 1B). Often, these cases are treated by crown lengthening and restoration only, which is a compromised treatment plan. It requires unnecessary removal of vital soft and hard tissue and creates greater risks of damage to the pulpal tissues during final preparations.6 However, treating the fundamental problems requires the orthodontic intrusion5 of the anterior dentogingival complex (Figure 1C) and subsequent restoration of the lost tooth structure5 (Figure 1D). Leveling the gingiva can serve as an initial guide7 for the orthodontist. However, until the correct incisal edges are in place, he or she cannot accurately predict how the teeth relate to the lips when smiling, nor how the tooth form relates to the envelope of function4 as orthodontics is finalized (Figure 1E). In addition, the patient may not appreciate the unsightly “disappearance” of the remaining tooth structure, if teeth are intruded significantly during the orthodontic process (Figure 1C). Options for addressing these problems include preparation of the teeth and placement of provisional crowns (represents aggressive therapy and is prone to maintenance problems); composite-resin bonding (a very conservative treatment);8 or no restorative treatment at this stage. Because bonded-porcelain restorations preserve more tooth structure as compared with conventional metal-ceramic crowns, they are preferred as final restorations in most cases; therefore, conservation of tooth structure at this stage is most desirable.6
Intermediate Restoration of Incisal Edges
Adding the incisal edges in composite resin during orthodontic treatment seems an obvious and proven solution. This form of “trial therapy”4 is traditionally performed with the brackets in place and the wire removed by the “free-hand” placement of composite resin. Likely reasons that this is not more common may be ascribed to the level of difficulty involved and the amount of time required in placing direct composites in the esthetic zone. Also, the dentist may hesitate to increase costs to the patient who is already anticipating a substantial investment in final restoration. A simpler and less time-consuming method can be employed in which a wax-up is performed on a diagnostic model1 and a clear vinyl polysiloxane (VPS) matrix is used to direct warmed composite resin onto the teeth.9 The latter method serves well by reducing chair-time for the dentist and lowering cost to the patient; and the immediate improvement in the smile can be dramatic. In the authors’ experience, patient responses have been overwhelmingly positive. The orthodontist or restorative dentist can make modifications as needed to satisfy the esthetic or functional requirements of the case with the patient’s approval as final orthodontic movements are performed (Figure 1E).
Final porcelain restorations are placed only after adequate time has elapsed to allow settling of the teeth following bracket removal and healing of the gingival tissues. Intrusion cases may require up to 6 months of retention to achieve stable positions,7 and soft-tissue maturation may require an even greater length of time. The intermediate composite-resin restorations serve as the template for the final porcelain restorations, establishing proper incisal-edge position, emergence form, and functional occlusion,4 while maintaining optimal gingival health and esthetics. Ideal preparations can now be made with maximal conservation of tooth structure in mind to help ensure the longevity of the final restorations.6
Severe Dental Erosion
The 36-year-old female in Figure 2A wanted a “prettier smile.” Figure 2C and Figure 2D show a combination of the problems of tooth destruction from incisal wear and lingual erosion from bulimia.10 Severe erosion cases present a unique problem for the orthodontist. Not only must he or she establish the correct mesio-distal tooth positions within the arch, but the orthodontist must also develop the correct interarch relationships and maintain them with much of the lingual and incisal tooth structure of the upper incisors missing (Figure 1C). Establishing spaces in orthodontics to compensate for malformed or worn teeth is sometimes relatively easy; maintenance is extremely difficult.1 Elastics would move the anteriors together easily (as would natural eruptive forces if left unchecked); therefore, these normally positive forces become negative for the orthodontist until the tooth structure is replaced. Thus, the intermediate restoration of the upper anterior teeth after initial orthodontic spacing removes the orthodontist’s guesswork that would otherwise be involved in determining the ideal positions of the teeth 3-dimensionally. The orthodontist in this case exaggerated the spacing of the teeth to give the restorative dentist better access to create ideal tooth morphology and to make placement and finishing of the composite-resin build-ups easier (Figure 1C, Figure 2F, and Figure 2G) At this point, the restorative goal was not to develop ideal occlusal or proximal relationships yet.
As in the previous case, warmed composite resin was bonded directly onto the incisal and lingual surfaces of teeth Nos. 6 to 11. The use of a wax-up and clear VPS matrix provided greater control and facilitated the chairside procedure (Figure 2E through Figure 2G ). With this technique, chair-time and costs were reduced and the VPS matrix eliminated the traditional step of model duplication of the wax-up and plastic matrix formation, saving laboratory time as well. This approach also preserves vital tooth structure at the final restorative phase by protecting against overreduction of the tooth for porcelain placement where tooth structure was already missing. Orthodontic treatment was continued, removing the arch wire only temporarily for composite-resin placement. The orthodontist or restorative dentist has the opportunity to reshape the composite-resin buildups as needed to create ideal form as the proximal contacts develop and the interincisal relationship finalizes. Occlusal and frontal views of the composite-resin build-ups are shown in Figure 2F through Figure 2G. The orthodontist can more predictably create an ideal relationship of the anterior teeth and the patient appreciates the cosmetic improvement in the newly developed smile (Figure 2H through Figure 2I).
Denture Tooth Veneers
The 10-year-old patient shown in Figure 3A initiated orthodontic treatment at a young age when multiple permanent teeth were found to be congenitally missing, a condition termed oligodontia (severe partial anodontia). Oligodontia is characterized by the congenital absence of more than six permanent teeth, excluding third molars.11 Patients with the condition may have severe psychological problems12 related to an unesthetic smile, which is from missing and small teeth and resulting diastemas in the dentition.13 Functionally, a posterior cross-bite had developed in this patient, probably resulting from alveolar bone underdevelopment in the absence of the eruption process of the missing permanent teeth roots14 (Figure 3A and Figure 3B). In such cases, early intervention and space management with dentofacial orthopedics by the orthodontist is appropriate.2
The orthodontist carefully managed this case for several years. Rapid palatal expansion therapy, reverse-pull headgear treatment, and space maintenance were employed to influence growth and development until implant therapy and restorative treatment could begin, minimizing the potential negative consequences of no treatment (Figure 3C). The remaining permanent incisors were smaller than normal,13 and the upper primary lateral incisors were scheduled for extraction. After positioning the upper central incisors as close to ideal as possible, the orthodontist requested intermediate restoration of the upper anterior teeth. The permanent first premolars were positioned in the cuspid locations for conversion to cuspids, thereby preventing problems associated with adjacent implants in the esthetic zone. Given the major tooth-size and space discrepancies in this case, more traditional composite-resin buildup procedures were impractical for intermediate restorations.
Denture teeth, carefully selected for size and shape, can be reshaped and hollow-ground to resemble veneers (Figure 3D). Similar methods have had good success when used to design implant provisional crowns. This procedure can be performed most efficiently on a diagnostic model in the laboratory to save valuable chair-time. The laboratory steps are tedious, requiring multiple trials and adjustments. It is important that the clinician positions the denture tooth veneers along the long axes of the teeth and resists the temptation to correct misalignments restoratively. This represents one of the more difficult aspects of intermediate restorations for the restorative dentist who, by training, normally restores teeth to the existing occlusion and adjacent tooth structures. Instead, he or she should build to ideal individual tooth anatomy and then allow the orthodontist to correct the proper occlusal and arch-form relationships.
In this case, the plan created during the model-preparatory work was to recontour the soft tissues because of slightly redundant gingival tissues and to remove the primary lateral incisors. The denture teeth were trimmed, thinned, and luted precisely onto the model with block-out compound, and then the positions were registered in a putty silicone index15,16 to facilitate transfer to the mouth (Figure 3E).17 The margins of the veneers are very thin as seen in Figure 3E. The silicone index allows the visualization of the veneer seating process, thereby ensuring proper adaptation to the teeth and easier cleanup. The teeth were prepared very slightly at the line-angles and etched for bonding in the same fashion as conventional veneers. Warmed composite resin (to increase flow)9 was loaded into the denture tooth veneers and pressed onto the teeth. Excess composite resin was removed, and then the veneers were light-cured, finished, and polished. Radiosurgery created a more desirable soft-tissue profile in relationship to bone and to maintain a healthy biologic width.18 The primary lateral incisors were extracted, and the matching denture tooth lateral incisors were sent to the orthodontist for use as pontics on the arch-wire (Figure 3G).
The denture teeth exhibit excellent shape and surface characteristics, and they are very esthetic as well as efficient for the authors’ purposes. They are relatively inexpensive and yet have enough resiliency to withstand the rigors of orthodontic forces for the extended time necessary to complete a treatment process of this nature. As the orthodontic process approaches finishing stages, they may be adjusted easily and refined similarly to the composite resin build-ups.
Long-term provisional stabilization is a significant consideration in these complex interdisciplinary cases because often the provisionals may remain for months or even years.1 Microleakage problems at the margins are common in long-term temporary crowns, whether detected or not, and temporary crown loosening frequently disrupts the orthodontic process. For these reasons, the authors prefer these rather than temporary crowns for long-term use whenever the teeth are amenable to composite bonding. The risks of sensitivity, leakage, and caries are significantly reduced.1 The orthodontist has the ability to recontour and adjust the provisional denture tooth veneers or the composite resin buildups easily as he or she closes spaces, develops proximal contacts, and creates a much more predictable treatment outcome (Figure 3H and Figure 3I). When the teeth are ready for final porcelain restorations, ideal tooth preparations can be made, conserving healthy tooth structure, and thereby helping to preserve tooth vitality and reduce postoperative sensitivity.6
Conclusion
The importance of communication between interdisciplinary team members increases with the complexity of the case. When orthodontics is indicated and severe wear or malformation of the dentition also is present, the intermediate restoration of the anterior teeth may be necessary, thereby requiring communication 3-dimensionally and precisely between the restorative dentist and orthodontist. The need to correctly identify incisal edge position in cases of severe incisal wear and subsequent dentoalveolar extrusion ideally requires the restoration of proper tooth form prior to orthodontic finishing. Composite bonding serves this purpose well; it is conservative and durable. The risks of leakage, sensitivity, and caries are reduced. Techniques are available to facilitate the bonding process and reduce chair-time and the patient’s costs.
Cases that involve more extensive missing tooth structure (eg, microdontia, oligodontia) may require intermediate restoration through the modification of denture teeth to create denture tooth veneers. Together, the methods described can simplify intermediate restorations and enhance final treatment outcomes enabled by clear communication among the team regarding the tooth forms and positions ultimately desired.
References
1. Spear F. The role of temporization in interdisciplinary periodontal and orthodontic treatment. Advanced Esthetics & Interdisciplinary Dentistry. 2005;1(3):2-9.
2. Roblee RD. Interdisciplinary Dentofacial Therapy: A Comprehensive Approach to Optimal Patient Care. Hanover Park, IL: Quintessence Publishing; 1994.
3. Winter RR. Interdisciplinary treatment planning: why is this not the standard of care? J Esthet Restor Dent. 2007;19(5):284-287.
4. Vence BS. Predictable esthetics through functional design: the role of harmonious disclusion. J Esthet Restor Dent. 2007;19(4):185-191.
5. Kokich VG, Spear FM, Mathew DP. Mandibular incisor intrusion: an adjunct to restoring short, abraded anterior teeth. Advanced Esthetics & Interdisciplinary Dentistry. 2006;2(4):22-28.
6. Edelhoff D, Sorensen JA. Tooth structure removal associated with various preparation designs for anterior teeth. J Prosthet Dent. 2002;87(5): 503-509.
7. Kokich VG, Spear FM. Interdisciplinary management of anterior guidance: a case report. Advanced Esthetics & Interdisciplinary Dentistry. 2007;3(3): 17-24.
8. Soares CJ, Pizi EC, Fonseca RB, et al. Direct restoration of worn maxillary teeth with a combination of composite resin materials: a case report. J Esthet Restor Dent. 2005;17(2):85-91.
9. Daronch M, Rueggeberg FA, Moss L, et al. Clinically relevant issues related to preheating composites. J Esthet Restor Dent. 2006;18(6): 340-350.
10. Spear F. A patient with severe wear on the posterior teeth and minimal wear on the anterior teeth. J Am Dent Assoc. 2009;140(1):99-104.
11. Jorgenson RJ. Clinician’s view of hypodontia. J Am Dent Assoc. 1980;101(2):283-286.
12. Hummel P, Guddack S. Psychosocial stress and adaptive functioning in children suffering from hypohidrotic ectodermal dysplasia. Pediatr Dermatol. 1997;14(3):180-185.
13. Schalk-Van der Weide Y. Oligodontia. A Clinical, Radiographic and Genetic Evaluation [thesis]. The Netherlands: University of Utrecht; 1992.
14. Zwetchkenbaum S, Oh WS. Prosthodontic management of abnormal tooth development secondary to chemotherapy: a clinical report. J Prosthet Dent. 2007;98(6): 429-435.
15. Fridrich T, Foo H. Tooth position index for the fabrication of a mandibular implant-supported overdenture bar. J Prosthet Dent. 1998;80(1): 121-123.
16. Alvares I, Sensi LG, Aranjo EM Jr, et al. Silicone index: an alternative approach for tooth reattachment. J Esthet Restor Dent. 2007;19(5): 240-245.
17. Felippe LA, Monteiro S Jr, De Andrada C, et al. Clinical strategies for success in proximoincisal composite restorations. Part II: composite application technique. J Esthet Restor Dent. 2005;17(1): 11-20.
18. Kois JC. Altering gingival levels: the restorative connection. Part I: biologic variables. J Esthet Restor Dent. 1994;6(1):3-7.
To take the quiz and receive credit for this course, click here and you will be redirected to the Dawson Center CE Portal.
Thank you.
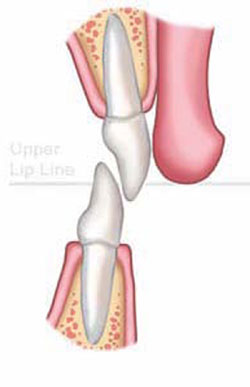 Figure 1A Unwom initial malocclusion | 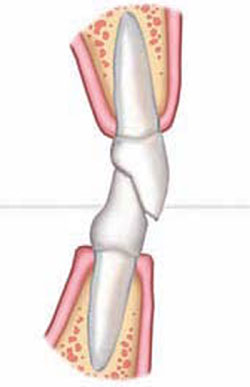 Figure 1B Dental wear with secondary dentoalveolar extrusion | ||||||
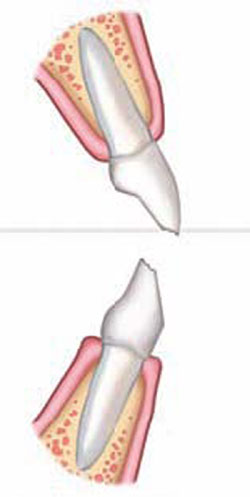 Figure 1C Orthodontic overcorrection | 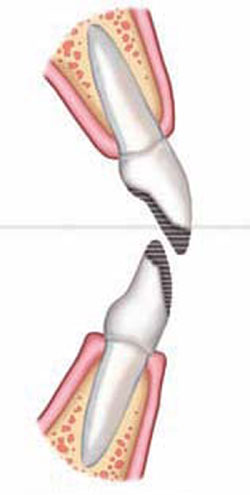 Figure 1D Intermediate restoration to ideal anatomy (not function) | ||||||
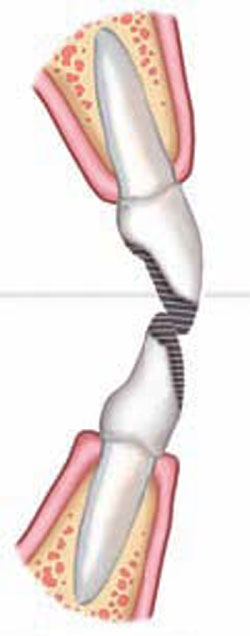 Figure 1E Orthodontic finalization of esthetics and function | |||||||
| FIGURE 1A THROUGH FIGURE 1E Incisal wear with dentoalveolar extrusion. Note the relationship of the maxillary incisal edge to lip line. | |||||||
| | |||||||
 Figure 2A Smile view showing incisal wear and open buccal corridors. |  Figure 2B Retracted view of worn incisal edges with uneven gingival margins. Patient exhibits classic signs of bulimia: lingual erosion of upper incisors and premolars. | ||||||
 Figure 2C Initial orthodontics to create space for intermediate restorations.Note the exaggerated spacing of the anterior upper teeth.Alignment of the gingiva and initial leveling. |  Figure 2D Occlusal view depicts severe destruction of lingual tooth structure. The orthodontist has provided access to perform restorative procedures more easily. | ||||||
 Figure 2E Clear VPS matrix from waxup formed on model.Matrix loaded with warm composite resin and pressed into place. Light curing of composite resin directly through matrix. |  Figure 2F Completed lingual view of ideal anatomic form of teeth Nos. 6 to 11. | ||||||
 Figure 2G Frontal smile showing incisal edges immediately after placement. |  Figure 2H Smile view 3 months after bracket repositioning shows improved esthetics and even gingival architecture.Note the filling out of the buccal corridors. | ||||||
 Figure 2I Retracted view after orthodontic refinement. | |||||||
| | |||||||
 Figure 3A A 10-year-old patient with oligodontia, missing multiple permanent teeth. Retracted view shows posterior cross-bite, resulting from underdeveloped alveolus. |  Figure 3B Panoramic radiograph shows retained primary teeth, eight missing permanent teeth, and delayed eruption pattern. | ||||||
 Figure 3C Orthodontics and dentofacial orthopedics were performed to develop arches for optimal future restorative.Mini-implants were used for orthodontic anchorage. |  Figure 3D Denture teeth hollow-ground and luted to model along the long axes of the teeth. Lateral incisors will be extracted. | ||||||
 Figure 3E Putty silicone index formed to aid transfer to mouth and denture tooth veneers placed into index. Note the very thin material remaining, similar to porcelain veneers. |  Figure 3F Denture tooth veneers bonded in place in similar fashion to porcelain veneers.Wetting surface with methyl methacrylate monomer and treating with unfilled resin improves bond. | ||||||
 Figure 3G Smile view with matching lateral incisor pontics in place on the orthodontic wire. First premolars were converted to cuspids to prevent the need for adjacent anterior implants. |  Figure 3H Occlusal view after 1 year. Veneers are easy to reshape as interproximal and occlusal contacts are developed. | ||||||
 Figure 3I Progress at 1 year. | |||||||
| |||||||



