Applications of Etch-and-Rinse Adhesive Bonding for Esthetic Restorative Dentistry
Howard E. Strassler, DMD; Luis Guilherme Sensi, DDS, MS, PhD
Abstract
This article examines the long-term clinical trials with posterior composite resin restorations, porcelain veneers, crowns, and resin and ceramic inlays and onlays that provide strong evidence of clinical success and durability when an etch-and-rinse adhesive technique is used. Based upon the current evidence available, self-etching systems have applications for direct placement composite resins, and etch-and-rinse adhesives remain the standard for adhesive restorative dentistry.
G.V. Black described the retention of restorations based upon cavity design and undercut dentin.1 Even with the caries removed, the limitations of the restorative materials available at the time (ie, gold foil and dental silver amalgam) necessitated removal of additional tooth structure in order to fulfill the requirements of retaining the restorative material. The goal of conserving tooth structure before restoration led to an evolution of adhesive bonding systems.
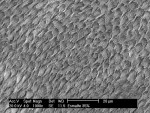
In 1955, Buonocore described a clinical technique that utilized a diluted phosphoric acid to etch the enamel surface and provide retention of unfilled, self-cured acrylic resins.2 The resin would mechanically lock to the microscopically roughened enamel surface, forming small "tags" as it flowed into the 10 to 40 micrometer deep enamel microporosities and then polymerized (Figure 1). The placement of sealants was the first clinical use of this technique.3 The combination of acid-etched enamel and adhesive composite resin restorations afforded the benefits of reducing or eliminating microleakage at the enamel margins with a decrease in sensitivity, less discoloration at the margins, lower rates of recurrent caries, and improved retention of the restorations.4,5
The effectiveness and success of etched enamel/resin bonds have been demonstrated in many reported clinical trials.6 Unlike enamel bonding, dentin bonding has seen an evolution in its viability. Effective dentin bonding materials should fulfill the following goals.
- The material should be retentive to dentin at a clinically acceptable level and able to withstand intraoral forces of occlusion and mastication.
- The bond should be instantaneous once the material has set.
- The material and technique must be biocompatible.
- The material should resist forces of polymerization shrinkage of the composite resins and the coefficient of thermal expansion and contraction to eliminate microleakage.
- The material should create a long-lasting bond to dentin.
- Postoperative sensitivity must be minimized or eliminated.
The earliest research in 1956 with dentin bonding focused on chemical adhesion of resins to the inorganic components of dentin. Buonocore and coworkers developed a methacrylate-based dentin adhesive that contained phosphate groups to attach to the calcium ions on the dentin surface.7 The basis of the bond was the presence of the dentin smear layer.8 While a weak bond was created, it was a clinically unacceptable bond to dentin. This basis of a phosphate-calcium bond was later introduced and described as the third generation phosphate ester bonding systems. These bonding systemsa,b bonded to the calcium rich dentin smear layer and etched enamel. Their bond strengths to dentin were limited by the adhesion of the smear layer to the dentin. Unfortunately, the bond's durability was impacted by hydrolysis, which occurred over time to the phosphate/calcium bond.9,10 These products had limited success, and the search continued for a better adhesive to dentin.
Concurrently, another research path for dentin bonding investigated the use of an etch-and-rinse total-etch approach, etching the enamel and dentin simultaneously with phosphoric acid.11,12 At the time, there was concern that phosphoric acid placed on dentin would cause pulpal inflammation and necrosis.13 Jennings and Ranly demonstrated that the pulpal effect of phosphoric acid on dentin for one minute was minimal.14 Early results reported with dentin etching were disappointing because the adhesive resin utilized was the same unfilled hydrophobic bonding resin (ie, Bis-GMA) used for etched enamel.12 The hydrophobic resin would not wet the moist, vital dentin, and predictable adhesion could not be produced.
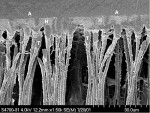
The breakthrough in the etch-and-rinse total-etch approach was first described in the late 1970s by Fusayama and coworkers,15 Bertolotti,16 and Kanca.17 They demonstrated the success of the etch-and-rinse total-etch adhesive bond based upon the addition of a hydrophilic monomer [eg, hydroxyethyl methylmethacrylate (HEMA)] to the primer and adhesive (Figure 2). This hydrophilic monomer allows the adhesive resin to penetrate the peritubular dentin and dentinal tubules.18 At the same time, Bowen was investigating the use of a dentin primer that actually was a self-cure adhesive that was painted on the enamel and dentin; it produced clinically acceptable bonds.19 This primer was commercialized to become two of the earliest etch-and-rinse total-bond adhesives introducedc,d and that are still being used successfully. In recent years, self-etch adhesives for bonding to enamel and dentin have been introduced.20
Today, adhesive bonding can be divided into two major categories: etch-and-rinse adhesive bonding and self-etch adhesive bonding. Although many have referred to etch-and-rinse systems as total-etch adhesion because a separate phosphoric acid etchant is rinsed from the surface, whereas self-etch adhesives employ an acidic monomer contained in a separate primer or within a single liquid component, both types of systems are total-etch.21 For the purpose of this article, the differentiation of the two systems will be etch-and-rinse when a separate acid application with rinsing is part of the clinical procedure and self-etch when there is no need for rinsing. Within these two categories, there are different adhesive agents with a wide variety of chemistries.
Although new concepts are typically interpreted as being superior in restorative dentistry, prior to changing materials and techniques, clinicians should have sufficient evidence to support their change.22 Unfortunately, one drawback to long-term testing of dental materials and dentin-enamel adhesives is the rapid turnover and new product introduction that has characterized the dental marketplace.23 Perdigão made note that numerous simplified adhesives have been introduced to the dental market within the last few years, sometimes without comprehensive testing to validate the performance claimed by the manufacturers.24 Fortunately, one category of adhesive bonding using an etch-and-rinse has been well researched.25-35 Long-term studies with self-etch adhesive systems are just becoming available.36-38 Of note, enamel margin degradation was more readily apparent in these studies when compared to etch-and-rinse adhesives.
Clinical success with etch-and-rinse adhesives is dependent on the proper execution of the basic clinical technique that follows.
- Prepare the tooth.
- Etch with a phosphoric acid (range of concentration 10% to 37%) for 15 to 30 seconds; 15 seconds for dentin only.
- Rinse with an air-water spray for 10 seconds.
- Dry the tooth, leaving the enamel frosty and the dentin glossy and moist.39,40
- Apply the adhesive system of choice with polymerization.
- Apply the restorative material with polymerization.
Applications for using an etch-and-rinse adhesive bonding technique in esthetic restorative dentistry include sealants, anterior composite resins, posterior composite resins, resin cementation with fiber posts, porcelain-metal, indirect composite resin, all-ceramic restorations, and conservative treatment of the worn dentition.
Etch-and-rinse bonding systems have been referred to as both fourth and fifth generation bonding agents (Table 1). Typically, fourth generation bonding agents consist of three steps and have multiple bottles with a separate dentin primer and a separate resin adhesive (ie, etch-primer-adhesive). Fifth generation bonding agents combine the dentin primer and adhesive in a single bottle and require two steps (ie, etch-prime/adhesive).20
Clinical Applications
A. Preventive Restorations: Sealants and Preventive Resin Restorations (PRR)
The sealing of caries susceptible pits and fissures using an etch-and-rinse technique is well accepted.41 Also, with an etch-and-rinse total seal adhesive technique, the use of minimally invasive preparations and restorations with a combined sealant-composite resin or the use of a flowable composite resin (ie, PRR), accomplished with either a small diameter bur or an air abrasion technique, has become a routine procedure in restorative practices.42,43 Typically, pit and fissure sealants are treatments employed for children or adolescent patients when either there is a diagnosis of active fissure caries or when a risk for caries has been recognized due to the invaginated open morphology of the occlusal pits and fissures of the posterior teeth. Sealants should be placed shortly after tooth eruption. In some cases of high-risk adult patients, sealants can be placed as well.44 There has been no concern about sealing in active dentinal caries beneath a sealant. Evidence demonstrates that, once sealed and kept sealed, dentinal caries do not progress.45
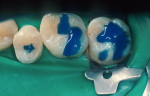
When minimal caries are diagnosed in pits and fissures on occlusal surfaces, a minimally invasive preparation can be accomplished with either air abrasion or small burs (Figure 3A; Figure 3B; Figure 3C). Once prepared, the tooth is etched (Figure 4), an adhesive is placed and light cured, and a flow-able composite resin is placed for the minimally invasive preparation as a PRR; the more extensive preparations are restored with a packable composite resin (Figure 5).
B. Anterior Restorations: Class III, IV, V, and Facial Veneers with Direct Composite Resin
When preparing Class III, IV, V, and facial veneer preparations for restorations using a total-etch adhesive technique with composite resin, the cavosurface margins of the preparation need to be prepared in order to optimize the etching process and adhesive bond. For Class III preparations, evidence demonstrates that cavosurface margins need not be beveled for a good adhesive bond.46 When shade matching is important because the margin of the preparation is in an esthetic area, an esthetic blend of composite resin from restoration to tooth is better accomplished using a cavosurface margin bevel.4 No bevel should be placed if the enamel is very thin at gingival margins or the margin is on the root surface.
While Class III preparations are employed for teeth with caries or existing defective restorations, the Class IV preparation can either be for a tooth with caries, a defective restoration, or when there has been a traumatic fracture. Typically, the Class IV restoration is placed for fractured teeth. Class IV preparations require that either a bevel of at least 1.0 mm long47 or a shoulder-chamfer margin of at least 1.0 mm to 2.0 mm long be placed with a bullet nose diamond.5 Using this preparation technique leads to durable, long-lasting restorations (Figure 6A and Figure 6B). For patients desiring a change in the appearance of teeth in the esthetic zone, a facial veneer sculpted with direct composite resin can accomplish the task (Figure 7A and Figure 7B). The desired esthetic result and treatment planned can include color changes, space closures, tooth reshaping, and tooth misalignment corrections. The preparation of these teeth depends on the desired final restorative result (eg, a facially displaced maxillary lateral incisor would need facial reduction to bring it into alignment with the adjacent anterior teeth when restored, while an undersized peg-shaped lateral incisor would only require a roughening of the surface). In most cases, the adhesive bond is to enamel, with only a 15-second etch with phosphoric acid.
A tooth fracture where the patient has the tooth fragment is a more unusual clinical situation that can be managed with an etch-and-rinse adhesive bond. There is evidence that when the patient has the tooth segment from a traumatic fracture, it can be bonded using a total-etch adhesive technique to successfully restore the tooth.48,49 Cases where the tooth fragment has been reattached have been reported to be still in place after seven years.50
Similar to the Class IV lesion, Class V lesions do not necessarily have to be carious. In many cases, the etiology of the Class V lesion is either a noncarious erosive, abrasive, or abfracted notching of the tooth at the cervical third.51,52 The outline form and depth when preparing Class V carious lesions for an etch-and-rinse adhesive restoration should be only the removal of the caries. While studies have reported good rates of retention of composite resin with only an adhesive technique,53,54 the use of mechanical undercuts will improve retention.55,56 Where adequate enamel exists, the enamel margins should be beveled to increase the bonding surface area and allow an esthetic blend of composite resin to tooth. For teeth with notch-shaped lesions, the use of an undercut created with a one-fourth round bur or a 33.5 inverted cone bur will improve retention when the preparation is more than 1.0 mm in depth. For all notch-shaped lesions, the exposed dentin to be bonded should be cleaned with a prophylaxis angle and pumice-water paste, a small round bur, or a diamond to freshen and clean the dentin. In many cases, the cervical notching of the lesion creates a beveled surface. In these cases, beveling is not necessary. All preparations ending on the root surface should not be beveled.
C. Posterior Restorations: Class I and II Composite Resin
With the use of an etch-and-rinse adhesive technique with composite resin, clinical studies have demonstrated that composite resins can be considered amalgam alternatives in routine-sized preparations.29,57,58 While silver amalgam, cast gold, and porcelain-metal are still the standard for posterior tooth restorations because of their durability and wear resistance, for routine-sized preparations, composite resins can now be viewed as metal alternatives.59,60
The American Dental Association Council on Scientific Affairs stated that composite resin restorations allow for more conservative preparations, preserving tooth structure. Its guidelines further state that resin-based composites can be used for pit and fissure sealing, PRRs, initial Class I and Class II lesions using modified cavity preparation design, and moderate-sized Class I and Class II restorations. The Council's consensus was not to use composites when teeth have heavy occlusal stress, sites cannot be isolated, and patients are allergic or sensitive to resin-based composites.59 The current advantages of composite resins over silver amalgam are that they are highly esthetic, reinforce tooth structure, and conserve more tooth structure in preparation design (Figure 8A; Figure 8B; Figure 8C).61
General guidelines to improve clinical success with posterior composite resins include the following:
- Preparations in which an occlusal contact is supported by tooth structure;
- Supragingival preparation margins and the ability to place the dental dam;
- Preference of enamel margins; Note, however, that margins on the cementum of the root are acceptable if the margin is supragingival after dam placement;
- Adequate light curing in the proximal box of a Class II (ie, at least 10 seconds with a high-intensity light) to assure polymerization of the adhesive and composite resin over the distance to the end of the gingival margin.62
In recent years, the trend for posterior composite resin restorations has been to use self-etch adhesives to reduce postoperative sensitivity.20 Several different studies evaluated postoperative sensitivity using etch-and-rinse and self-etch adhesives.39,63-67 The results of these studies demonstrated no difference in postoperative sensitivity between etch-and-rinse and self-etch adhesives. In fact, the conclusion of one study stated that postoperative sensitivity may depend on the restorative technique and variability among operators, rather than on the type of enamel-dentin adhesive used.63
One area of inconsistency with etch-and-rinse bonding has been the bonding potential to desiccated dentin.40,68 The inherent nature of self-etch adhesives is no rinse, leaving the surface moist. This may contribute to minimizing postoperative sensitivity.69
D. Cementation with an Etch-and-Rinse Adhesive Technique
The etch-and-rinse adhesive technique can be used for cementation of all indirectly fabricated esthetic restorations, such as laboratory-fabricated veneers (eg, composite resin and ceramic), posterior restorations (eg, resin and ceramic inlays and onlays), crowns (eg, porcelain-metal, ceramic, composite resin), and fixed partial dentures (eg, porcelain-metal, ceramic, fiber-reinforced composite resin).
When placing laboratory-fabricated restorations using an etch-and-rinse adhesive technique, it is important to not overetch the dentin. An etching time of 10 to 15 seconds is adequate. In addition, an adhesive that is compatible with the self-cure, dual-cure, or light-cure composite resin cement being employed should be selected.
An area of recent investigation has been the compatibility of etch-and-rinse and self-etch adhesive systems with composite resin cementation. Contradictory evidence exists that some single-bottle adhesive systems do not bond well to self-cure and dual-cure composite resins due to the acidity of the single-bottle primer/adhesive. Studies demonstrating a decreased bond and other studies showing no effect have been reported.70-72 Some recent studies evaluating self-etch systems and their compatibility with dual-cure and self-cure composite resins have demonstrated some changes in chemistry resulting in composite resin-adhesive compatibility.72,73 This variability requires that the clinician review the manufacturer's recommendations for uses with self-cure and dual-cure composite resins.
When using etch-and-rinse adhesives with dual- and self-cure composite resin cements for luting crowns, inlays, and onlays, it is important when placing the adhesive for cementation procedures that it be air thinned before light curing to avoid pooling of the resin in areas that could interfere with restoration seating. Use of a self-cure or dual-cure adhesive that will polymerize in the absence of light curing eliminates this problem. Also, composite resin cements can be more viscous and thixotopic and require firm seating pressure to fully seat the restoration.74 In addition, etch-and-rinse adhesives can be used for the cementation of esthetic fiber posts,75 but the current trend for cementation of fiber posts is to use self-adhesive resin cements.76
As with facial veneering using direct composite resin, porcelain veneers are bonded to etched enamel surfaces. There are instances when there will be a limited amount of exposed dentin for bonding. When cementing porcelain or laboratory-fabricated composite resin veneers, an etch-and-rinse bonding system is advised. Most self-etching adhesives recommend the use of a phosphoric acid etchant when using the self-etch adhesive to bond a veneer. It is also recommended that a light-cure only luting composite resin be used with porcelain or composite veneers. Since veneers are typically cemented with a light-cure only luting composite resin, there is no concern about adhesive-composite resin incompatibility. The adhesive is light cured simultaneously with the resin cement after seating the veneer. The durability of porcelain veneers placed with an etch-and-rinse technique has been reported, with one study having a mean longevity of 15.2 years (Figure 9A and Figure 9B).33
E. Conservative Treatment of the Worn Dentition
As patients retain their teeth longer, changes occur to the biting surfaces of posterior teeth and incisal edges of anterior teeth due to wear. This destructive loss of tooth structure not associated with caries is caused by attrition due to normal and para function. It is frequently seen in the anterior region as the cupping of exposed dentin in the incisal edges, with enamel chipping or more substantial loss of tooth substance (Figure10 ). If an intervention is performed before anterior teeth demonstrate moderate to severe wear, the destruction can be reduced.77 In order to restore worn incisal edges, a conservative definitive preparation must be done. Using a small bur (ie, a pear-shaped burl or a small round burm), prepare into the dentin to a depth of 1.0 mm (Figure 11) to allow for adequate composite resin longevity as the restoration functions. The preparation removes only dentin, leaving a shell of enamel. Since the enamel may be quite thin in some areas, it may chip during preparation. This is not a problem because the composite resin will restore that surface. A periodontal probe should be used to verify a preparation depth of 1.0 mm of all enamel walls. The teeth can then be restored using an etch-and-rinse adhesive technique, with an etching time of no more than 15 seconds (Figure 12).
Conclusion
Although promising new techniques with self-etching adhesives have been introduced, there have been limited long-term clinical trials of few products with these bonding systems to demonstrate evidence that they will be as successful as the etch-and-rinse technique. The ability of self-etch adhesives to bond to enamel with the same durability as etch-and-rinse adhesives still must be demonstrated. Long-term clinical trials with posterior composite resin restorations, porcelain veneers, crowns, and resin and ceramic inlays and onlays provide strong evidence of clinical success and durability when using an etch-and-rinse adhesive technique.25-35, 37, 54, 55 Clearly, clinicians need to evaluate the clinical requirements of any adhesive restorative system they select for treating the natural dentition.
As evidenced by the popularity of self-etch single bottle adhesives, there has been a trend in recent years for simplification with adhesive systems. Based upon the current evidence available, self-etching systems have applications for direct placement composite resins.20,24,36-38 Given the evidence available, etch-and-rinse adhesives remain the standard for adhesive restorative dentistry.
Disclosure
Howard E. Strassler, DMD, has disclosed that he has received grant and research support from Den-Mat, Centrix, Dentsply, and Ultradent Products, Inc., as well as an honorarium from Den-Mat.
References
1. Black GV. A Work on Operative Dentistry. Chicago, IL: Medico-Dental Publishing Company; 1908.
2. Buonocore MG. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res. 1955;34: 849-853.
3. Cueto EI, Buonocore MG. Sealing of pits and fissures with an adhesive resin: its use in caries prevention. J Am Dent Assoc. 1967;75:121-128.
4. Torney DL, Denehy GE, Teixeira LC. The acid-etch class III composite resin restoration. J Prosthet Dent. 1977;38: 623-626.
5. Jordan RE, Suzuki M, Gwinnett AJ, et al. Restoration of fractured and hypoplastic incisors by the acid etch resin technique: a three-year report. J Am Dent Assoc. 1977;95: 795-803.
6. Strassler HE. Applications of total-etch adhesive bonding. Compend Contin Educ Dent. 2003;24: 427-430, 432, 434-436.
7. Brudevold F, Buonocore MG, Wileman W. A report on a resin composition capable of bonding to human dentin surfaces. 1956;35:846-851.
8. Diamond A, Carrel R. The smear layer: a review of restorative progress. J Pedod. 1984;8:219-226.
9. Retief DH, Gross JD, Bradley EL, et al. Tensile bond strengths of dentin bonding agents to dentin. Dent Mater. 1986;2: 72-77.
10. Eliades GC, Caputo AA, Vougiouklakis GJ. Composition, wetting properties and bond strength with dentin of 6 new dentin adhesives. Dent Mater. 1985;1:170-176.
11. Lee HL Jr., Orlowski JA, Scheidt GC, et al. Effects of acid etchants on dentin. J Dent Res. 1973;52:1228-1233.
12. Torney DL. The retentive ability of acid-etched dentin. J Prosthet Dent. 1978;39:169-172.
13. Skinner EW, Phillips RW. The Science of Dental Materials. 5th ed. Philadelphia, PA: Saunders; 1960.
14. Jennings RE, Ranly DM. Autoradiographic studies of 32 P penetration into enamel and dentin during acid etching. ASDC J Dent Child. 1972;39:69-71.
15. Fusayama T, Nakamura M, Kurosaki N, et al. Non-pressure adhesion of a new adhesive restorative resin. J Dent Res. 1979;58: 1364-1370.
16. Bertolloti R. Total etch—the rational dentin bonding protocol. J Esthet Dent. 1991;3:1-6.
17. Kanca J 3rd. One-year evaluation of a dentin-enamel bonding system. J Esthet Dent. 1990;2:100-103.
18. Summitt JB. Fundamentals of Operative Dentistry: A Contemporary Approach. 3rd ed. Chicago, IL: Quintessence Pub. Co.; 2006.
19. Bowen RL, Cobb EN. A method for bonding to dentin and enamel. J Am Dent Assoc. 1983;107:734-736.
20. Strassler HE. Self-etching resin adhesives. Inside Dentistry. 2007;3(2):50-54.
21. Van Meerbeek B, De Munck J, Yoshida Y, et al. Buonocore memorial lecture. Adhesion to enamel and dentin: current status and future challenges. Oper Dent. 2003;28: 215-235.
22. Duke ES. Self-etching adhesives: new science or just a trend? Compend Contin Educ Dent. 2002;23:1186-1187.
23. Meiers JC, Young D. Two-year composite/dentin bond stability. Am J Dent. 2001;14:141-144.
24. Perdigão J. New developments in dental adhesion. Dent Clin North Am. 2007;51:333-357, viii.
25. Swift EJ Jr., Perdigão J, Wilder AD Jr., et al. Clinical evaluation of two one-bottle dentin adhesives at three years. J Am Dent Assoc. 2001;132:1117-1123.
26. Baratieri LN, Ritter AV. Four-year clinical evaluation of posterior resin-based composite restorations placed using the total-etch technique. J Esthet Restor Dent. 2001;13:50-57.
27. Busato AL, Loguercio AD, Reis A, et al. Clinical evaluation of posterior composite restorations: 6-year results. Am J Dent. 2001;14: 304-308.
28. Donly KJ, Jensen ME, Triolo P, et al. A clinical comparison of resin composite inlay and onlay posterior restorations and cast-gold at 7 years. Quintessence Int. 1999;30: 163-168.
29. Gaengler P, Hoyer I, Montag R. Clinical evaluation of posterior composite restorations: the 10-year report. J Adhes Dent. 2001;3:185-194.
30. Thordrup M, Isidor F, Hörsted-Bindslev P. A prospective clinical study of indirect and direct composite and ceramic inlays: ten-year results. Quintessence Int. 2006;37:139-144.
31. Frankenberger R, Petschelt A, Krämer N. Leucite-reinforced glass ceramic inlays and onlays after six years: clinical behavior. Oper Dent. 2000;25:459-465.
32. Pallesen U, Qvist V. Composite resin fillings and inlays. An 11-year evaluation. Clin Oral Investig. 2003;7:71-79.
33. Strassler HE. Long term clinical evaluation of Cerinate etched porcelain veneers. J Dent Res. 2005;84(Special Issue A): Abstract #432.
34. Peumans M, De Munck J, Fieuws S, et al. A prospective ten-year clinical trial of porcelain veneers. J Adhes Dent. 2004;6: 65-76.
35. Unlu N, Belli S. Three-year clinical evaluation of fiber-reinforced composite fixed partial dentures using prefabricated pontics. J Adhes Dent. 2006;8:183-188.
36. Peumans M, De Munck J, Van Landuyt K, et al. Five-year clinical effectiveness of a two-step self-etching adhesive. J Adhes Dent. 2007;9:7-10.
37. Dijken JW, Sunnegårdh-Grönberg K, Lindberg A. Clinical long-term retention of etch-and-rinse and self-etch adhesive systems in non-carious cervical lesions A 13 years evaluation. Dent Mater. 2007;23:1101-1107.
38. Loguercio AD, Bittencourt DD, Baratieri LN, et al. A 36-month evaluation of self-etch and etch-and-rinse adhesives in noncarious cervical lesions. J Am Dent Assoc. 2007;138: 507-514.
39. Kanca J 3rd. Improving bond strength through acid etching of dentin and bonding to wet dentin surfaces. J Am Dent Assoc. 1992;123:35-43.
40. Gwinnett AJ. Moist versus dry dentin: its effect on shear bond strength. Am J Dent. 1992;5:127-129.
41. Mertz-Fairhurst EJ, Fairhurst CW, Williams JE, et al. A comparative clinical study of two pit and fissure sealants: 7-year results in Augusta, GA. J Am Dent Assoc. 1984;109:252-255.
42. Simonsen RJ. Preventive resin restorations (I). Quintessence Int Dent Dig. 1978;9:69-76.
43. Strassler HE, Goodman HS. A durable flowable composite resin for preventive resin restorations. Dent Today. 2002;21: 116-121, 178.
44. Ripa LW, Leske GS, Varma OA. Longitudinal study of the caries susceptibility of occlusal and proximal surfaces of first permanent molars. J Public Health Dent. 1988;48:8-13.
45. Handelman SL, Washburn F, Wopperer P. Two-year report of sealant effect on bacteria in dental caries. J Am Dent Assoc. 1976;93: 967-970.
46. Ireland E, Xu X, Burgess JO. Microleakage of beveled and nonbeveled Class 3 resin restorations. J Dent Res. 1998;77(Special Issue): Abstract #207.
47. Bagheri J, Denehy GE. Effect of enamel bevel and restoration lengths on Class IV acid-etch retained composite resin restoration. J Am Dent Assoc. 1983;107:951-952.
48. Simonsen RJ. Restoration of a fractured central incisor using original tooth fragment. J Am Dent Assoc. 1982;105: 646-648.
49. Strassler HE. Aesthetic management of traumatized anterior teeth. Dent Clin North Am. 1995;39:181-202.
50. Andreasen FM, Norén JG, Andreasen JO, et al. Long-term survival of fragment bonding in the treatment of fractured crowns: a multicenter clinical study. Quintessence Int. 1995;26: 669-681.
51. Grippo JO. Abfractions: a new classification of hard tissue lesions of teeth. J Esthet Dent. 1991;3:14-19.
52. Lee WC, Eakle WS. Possible role of tensile stress in the etiology of cervical erosive lesions of teeth. J Prosthet Dent. 1984;52: 374-380.
53. Van Meerbeek B, Peumans M, Gladys S, et al. Three-year clinical effectiveness of four total-etch dentinal adhesive systems in cervical lesions. Quintessence Int. 1996;27: 775-784.
54. Duke ES, Robbins JW, Snyder DS. Clinical evaluation of a dentinal adhesive system: three-year results. Quintessence Int. 1991;22:889-895.
55. Leinfelder KF. Restoration of abfracted lesions. Compendium. 1994;15:1396, 1398-1400.
56. McCoy RB, Anderson MH, Lepe X, et al. Clinical success of class V composite resin restorations without mechanical retention. J Am Dent Assoc. 1998;129: 593-599.
57. Wilder AD Jr., May KN Jr., Bayne SC, et al. Seventeen-year clinical study of ultraviolet-cured posterior composite Class I and II restorations. J Esthet Dent. 1999;11:135-142.
58. Lundin SA, Koch G. Class I and II posterior composite resin restorations after 5 and 10 years. Swed Dent J. 1999;23: 165-171.
59. Statement on posterior resin-based composites. ADA Council on Scientific Affairs; ADA Council on Dental Benefit Programs. J Am Dent Assoc. 1998;129:1627-1628.
60. Smales RJ, Webster DA, Leppard PI. Survival predictions of amalgam restorations. J Dent. 1991;19:272-277.
61. Strassler HE. Predictable and successful posterior packable Class II composite resins. Amer Dent Instit for CE. 2001;75:15-23.
62. Felix CA, Price RB. Effect of distance on power density from curing lights. J Dent Res. 2006;85(Special Issue B): Abstract #2468.
63. Perdigão J, Geraldeli S, Hodges JS. Total-etch versus self-etch adhesive: effect on postoperative sensitivity. J Am Dent Assoc. 2003;134:1621-1629.
64. Akpata ES, Behbehani J. Effect of bonding systems on post-operative sensitivity from posterior composites. Am J Dent. 2006;19: 151-154.
65. Perdigão J, Anauate-Netto C, Carmo AR, et al. The effect of adhesive and flowable composite on postoperative sensitivity: 2-week results. Quintessence Int. 2004;35:777-784.
66. Unemori M, Matsuya Y, Akashi A, et al. Self-etching adhesives and postoperative sensitivity. Am J Dent. 2004;17: 191-195.
67. Browning WD, Myers M, Downey M, et al. Reduction in post-operative sensitivity: a community based study. J Dent Res. 2006;85(Special Issue B): Abstract #1151.
68. Lee R, Blank JT. Simplify bonding with a single step: one component, no mixing. Contemp Esthet Rest Practice. 2003;7:45-46.
69. Hillam R, Pasciuta M, Cobb D. Shear bond strength of primer/adhesives with proprietary dual cure resin cement. J Dent Res. 2002;81(Special Issue A): Abstract #369, A-72.
70. Pasciuta M, Cobb D, Denehy G. Shear bond strength of dual cure primer/adhesives with dual cure resin cements. J Dent Res. 2002;81(Special Issue A): Abstract #405, A-76.
71. Christensen G. Self-etch primer (SEP) adhesives update. CRA Newsletter. 2003;27:1-5.
72. Cheong C, King NM, Pashley DH, et al. Incompatibility of self-etch adhesives with chemical/dual-cured composites: two-step vs one-step systems. Oper Dent. 2003;28: 747-755.
73. Tay FR, Pashley DH, Yiu CK, et al. Factors contributing to the incompatibility between simplified-step adhesives and chemically-cured or dual-cured composites. Part I. Single-step self-etching adhesive. J Adhes Dent. 2003;5:27-40.
74. White SN, Yu Z, Kipnis V. Effect of seating force on film thickness of new adhesive luting agents. J Prosthet Dent. 1992;68: 476-481.
75. Strassler HE, Cloutier PC. A new fiber post for esthetic dentistry. Compend Contin Educ Dent. 2003;24:742-744, 746,748.
76. Strassler HE. Fiber posts: an update. Inside Dentistry. 2007;3(3):70-75.
77. Strassler HE, Kihn PW, Yoon R. Conservative treatment of the worn dentition with adhesive composite resin. Contemp Esthet Rest Pract. 1999;3:42-52.
a Adper™ Scotchbond™, 3M, St. Paul, MN
b BondLite, Kerr Corporation, Orange, CA
c Tenure® Multi-Purpose, Den-Mat, Santa Maria, CA
d All-Bond 2®, Bisco, Inc., Schaumburg, IL
e Fissurotomy bur, SS White Burs, Inc., Lakewood, NJ
f Flowline®, Heraeus Kulzer, Armonk, NY
g Solitaire 2, Heraeus Kulzer, Armonk, NY
h 4 Seasons, Ivoclar Vivadent Inc., Amherst, NY
i 4 Seasons, Ivoclar Vivadent Inc., Amherst, NY
j Artiste® Nano Composite, Pentron Clinical Technologies, LLC, Wallingford, CT
k LUMINEERS®, Den-Mat®, Santa Maria, CA
l #329 or #330, SS White Burs, Lakewood, NJ
m #1/2 or #1, SS White Burs, Lakewood, NJ
n Virtuoso Universal, Den-Mat®, Santa Maria, CA
About the Authors
Howard E. Strassler, DMD
Director, Operative Dentistry – Endodontics, Prosthodontics, and Operative Dentistry
University of Maryland Dental School
Baltimore, Maryland
Luis Guilherme Sensi, DDS, MS, PhD
Assistant Professor – Endodontics, Prosthodontics, and Operative Dentistry
University of Maryland Dental School
Baltimore, Maryland