Material and Clinical Considerations for Full-coverage All-ceramic Restorations
Robert C. Margeas, DDS
Abstract
This article will examine and review the current all-ceramic alternatives available for restorative dentistry. Clinical factors that require consideration will also be examined, since these factors significantly affect clinicians’ decision-making processes when choosing the best materials for individual treatment plans. The ability to conventionally cement all-ceramic restorations has made placement procedures faster, as well as more efficient and esthetic. Yet, compromises often must be made when clinicians and patients are faced with choosing between the ultimate esthetics and function. Five cases are presented to illustrate possible clinical situations and the recommended options that are available to patients today.
Clinicians are faced daily with restorative situations requiring them to make decisions about the proper selection of materials for enhanced function and esthetics. Through traditional media sources and the Internet, today’s patients are increasingly being made aware of the availability of esthetic dentistry, and they will no longer be satisfied with treatment plans that provide ideal function without also offering an esthetic restoration. Yet, given the wealth of often confusing information and the fact that manufacturers now are producing a greater and better selection of alternatives that are both functionally and esthetically acceptable, choosing the right material in today’s dental marketplace can be challenging. To help make the selection process simpler, clinicians and their patients should be knowledgeable and well-informed about all-ceramic alternatives.
Historical Perspective
In 1885, Logan introduced the Richmond crown in which porcelain was fused to a platinum post. A year later, Land fabricated the first fused porcelain inlay and crown backed by platinum foil.1 No further advances using porcelain as a restorative material were made until the late 1950s.
The oldest all-ceramic material used in dentistry has been traditional feldspathic porcelain, which is developed from a powder and liquid. The material, which gained popularity in the early 1960s, was cemented using traditional zinc phosphate cement. Although highly esthetic, its inability to bond to enamel and dentin resulted in numerous failures. McLean introduced aluminous porcelain with an inclusion of dispersed alumina particles to resist crack formation a few years later.2
Product Developments
The next two decades produced little additional developments. However, the period from the 1980s until today ushered in a number of new products that are currently still available. These include:
A. Glass-infiltrated Alumina
Glass-infiltrated alumina (eg, In-Ceram Alumina®a) is a material with a sintered alumina glass-infiltrated infrastructure for anterior and posterior crowns, as well as anterior fixed bridges.3 This material demonstrates a flexural strength of 446 MPa.4 The opacious core limits its use as a highly esthetic material. A slip-casting technique or computer-aided design/computer-aided manufacturing (CAD/CAM) technology can be used to fabricate copings or frameworks from this material.
B. Glass-infiltrated Magnesium Alumina
Glass-infiltrated magnesium alumina (eg, In-Ceram Spinellb) was developed to produce a coping with greater translucency. However, the strength of the core material must be sacrificed in order to provide the greater translucency. This material’s flexural strength is approximately 343 MPa,4 and it is recommended for use only as anterior crowns. In this capacity, the material has demonstrated excellent results over a long period of time.5
C. Glass-infiltrated Alumina with Partially Stabilized Zirconia
Glass-infiltrated alumina with partially stabilized zirconia (eg, In-Ceram Zirconia®c) combines 35% partially stabilized zirconia with glass-infiltrated alumina to produce a material with greater strength. The flexural strength of this material is 604 MPa.4 Due to its high opacity,6 there is no significant advantage to using this material in highly esthetic areas. Slip-casting or CAD/CAM technology is used for fabricating infrastructures from this material.
D. Densely Sintered High-purity Aluminum Oxide
Densely sintered high-purity aluminum oxide (eg, Procera®d) is a polycrystalline ceramic. The ceramic core is glass free, which contributes to its high flexural strength of 650 MPa.4 The material can be used for anterior and posterior crowns, and CAD/CAM technology is employed for fabricating ceramic infrastructures.
E. Leucite-reinforced Glass Ceramics
Leucite-reinforced glass ceramics (eg, IPS Empress®e) rely on a leucite crystalline filler to reinforce its glass ceramic structures. This material has been chosen for highly esthetic restorations. However, due to the high translucency of the material,6 clinicians must be careful when attempting to cover dark, discolored tooth structure, metal posts, or implant abutments. Full-coverage crowns fabricated from this material have demonstrated excellent success rates in the anterior region.7 The flexural strength of this core material has been measured at 112 MPa.4 The copings are fabricated either with a lost wax technique or CAD/CAM technology. The inherent strength of these restorations depends upon adhesion to tooth structure. The internal surfaces must be treated with hydrofluoric acid and silanated.
F. Lithium Dislicate Glass Ceramics
Lithium dislicate glass ceramics (eg, IPS Empress® IIf; IPS Eris®g) were developed mainly for three-unit fixed partial dentures; they may also be used to create anterior/posterior crowns. The lost wax technique is used and the core is pressed. The material’s flexural strength is approximately three to four times stronger than that of leucite-reinforced glass ceramics.4 Restorations fabricated from this material also must be bonded to achieve their optimum strength.
G. Yttrium Tetragonal Zirconia Polycrystals
Yttrium tetragonal zirconia polycrystals (Y-TZP) (eg, Lava™h) are the basis for a high-strength, glass-free polycrystalline ceramic material used for the fabrication of anterior and posterior crown copings and fixed partial denture frameworks.8 The strength of the material is attributed to a process known as transformation toughening.9 If a crack begins to propagate through the ceramic, a high-energy stress state that causes the zirconia to transform from a tetragonal crystal configuration to a monoclinical configuration develops.9 In vitro studies of Y-TZP indicate flexural strengths of 900 MPa to 1200 MPa.10 Some Y-TZP restorative systems produce the substructure using CAD/CAM technology or by employing wax-up and milling processes. The size of the partially sintered, milled infrastructures is increased to compensate for shrinkage of 20% to 25% that occurs during final sintering. Esthetic layering porcelains may be used over the copings, or pressed ceramics can be employed.
Factors Contributing to Restorative Success
Regardless of the type of all-ceramic material used, the success of these metal-free restorations depends on several factors. The preparation should have rounded line angles, with the finish line being a deep chamfer or a 90° rounded shoulder. If the restoration will be bonded, the finish line should be supragingival or able to be isolated. With subgingival restorations, this may be impossible to achieve. If it is not possible to adequately isolate the preparation due to subgingival margins, it is best to use conventional cementation techniques.
Sufficient occlusal reduction is necessary to ensure adequate space for the frameworks. When there is restricted interocclusal distance, the material of choice may be metal-ceramics with metal linguals or occlusals. In addition to ensuring sufficient room for the foundation, it is also necessary to provide adequate resistance and retention form.
A much better esthetic outcome can be achieved in the presence of dark underlying tooth structure or metallic cores if either an alumina or zirconium material is chosen. When high translucency is needed, a feldspathic jacket, leucite-reinforced glass ceramic, or a glass-infiltrated magnesium aluminum are the restorations of choice.
Appropriate cementation protocol relates to the composition and strength of the core material. Feldspathic crowns must be etched with hydrofluoric acid and silanated prior to bonding. Adhesive cementation techniques are mandatory.11 Alumina and zirconia restorations may be cemented with conventional cements, such as resin-modified glass ionomers or self-etching, priming, and luting resins. Some concern remains regarding cementing ceramic polymers with resin-reinforced glass ionomer cements because of their slight setting expansion.12
By their nature, all-ceramic materials are somewhat brittle. Bonding with resin cement is necessary to ensure optimum strength of a feldspathic jacket or leucite-reinforced glass ceramic. Most failures of zirconia restorations occur in the layering porcelain or marginal ridge areas. Therefore, the substructures must be reinforced interproximally to prevent failures. It is rare to have a fracture of a zirconia core.
Patients with parafunctional habits must be evaluated carefully when deciding whether to provide them with an all-ceramic restoration. If a patient insists on a metal-free restoration, the highest strength core should be considered and occlusal guards utilized to prevent possible fractures. Wear of opposing tooth structure from an all-ceramic crown also may pose a problem. The higher leucite-containing ceramics have a tendency for high abrasion potential.13
Another important consideration is the fact that anterior and posterior restorations require different materials. For a patient with no parafunctional habits, a feldspathic jacket bonded to an anterior tooth may be the most esthetic restoration available. This may not be the best option for a posterior molar, however. Other clinical factors that require consideration are: placement of margins, health of the tissue, and whether the tooth presents with either a high translucency or a dark substructure.
The ability to cement all-ceramic restorations has made indirect metal-free procedures faster and more efficient. Often, however, compromises must be made when clinicians and patients are faced with choosing between the ultimate esthetics and function. The following case histories demonstrate some of the possible clinical situations dentists may encounter and the options that are available to patients.
Clinical Case #1
A 45-year-old patient presented with worn, sensitive teeth resulting from bulimia. She desired longer teeth. The teeth exhibited a favorable color, which made the use of a translucent material, such as feldspathic porcelain, a recommended option (Figure 1 and Figure 2). Exhibiting no posterior wear, her occlusion was ideal. The preparations were very conservative, with a minimal reduction of approximately 1.0 mm on the facial and lingual aspects. The feldspathic restorations were seated using resin cement after following a dentin bonding protocol. The final restorations achieved satisfactory function and esthetics (Figure 3 and Figure 4).
Clinical Case #2
A 50-year-old patient presented with extensive wear on all her teeth due to gastric reflux (Figure 5 and Figure 6). The treatment plan involved preparation of her teeth for full-coverage zirconium restorations. Due to the patient’s history of clenching, the zirconium restorations were considered ideal to provide the greatest strength, as well as enable the simplest way to conventionally cement the restorations. Although bonded onlays could have been used to restore some of the posterior teeth, the ease of cementation made these restorations appropriate choices. The bite was opened enough to fulfill the requirements of the restorative material and provide an esthetic result. The restorations were bonded using a self-etching, priming, and bonding resin to achieve the final result (Figure 7 and Figure 8).
Clinical Case #3
A 65-year-old patient presented with worn dentition and previously placed composite resin restorations (Figure 9 and Figure 10). The patient desired longer and brighter teeth, stated that he had fractured the bonding on several occasions, and indicated that he was ready for what he considered more definitive restorations. Alumina crowns were selected based on their masking ability, strength, and ease of cementation. The eight maxillary anterior teeth were prepared for full-coverage crowns with shoulder preparations. The restorations were seated using resin-reinforced glass ionomer cement (Figure 11 and Figure 12).
Clinical Case #4
A 40-year-old patient presented with an avulsed left central incisor that had been bonded to the adjacent teeth (Figure 13). Teeth Nos. 6 through 8, 10, and 11 all presented with previously placed porcelain veneers. The patient had lost facial bone above tooth No. 9 and did not elect to have an implant placed. Her main concern was esthetics, having seen people who had bridges placed in the past with what she described as “black gums,” so she did not want any metal-based restorations. The treatment plan developed consisted of new veneers for teeth Nos. 6, 7, and 11. A lithium disilcate glass-ceramic bridge was treatment planned for teeth Nos. 8 through 10. The teeth were prepared (Figure 14) and provisionalized. The final restorations were seated using a composite resin cement according to a dentin bonding protocol in order to achieve the final definitive results (Figure 15).
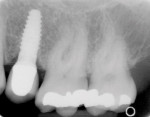
Clinical Case #5
A 38-year-old patient presented following a traumatic injury to her anterior dentition (Figure 16 and Figure 17). She severely fractured the two central incisors, with vertical fractures apparent on the lingual aspect (Figure 18). Her esthetic demands were the most important criteria. Tooth No. 10 also exhibited a Class IV fracture that she did not like. The treatment plan consisted of placing full-coverage leucite-reinforced glass ceramic restorations on the two maxillary central incisors and conservative veneers on the two lateral incisors to correct the fractures and create an ideal orthodontic result. The restorations were bonded using resin cement according to a dentin bonding protocol, producing definitive esthetic results that satisfied the patient’s expectations (Figure 19, Figure 20, Figure 21).
Conclusion
As demonstrated in the clinical cases presented, various all-ceramic alternatives are available today for restorative dentistry. The ability to cement all-ceramic restorations has made the procedures faster, as well as more efficient and esthetic. Yet, with more options, there may also be more confusion. In order to decide upon the best material choice, clinicians and patients must carefully weigh the advantages and disadvantages of each on a case-by-case basis. Depending upon the particular patient’s needs and desires, these decisions may involve compromises or a choice between the ultimate esthetics and function. However, by working together and examining the many predictable and satisfactory products that are available today, clinicians and their patients can arrive at an informed solution to satisfy the chief needs and desires of both parties.
References
1. McLean JW, Hubbard JR, Kedge MI. The Science and Art of Dental Ceramics. Chicago, IL: Quintessence Pub. Co.;1979-1980.
2. McLean JW, Hughes TH. The reinforcement of dental porcelain with ceramic oxides. Br Dent J. 1965;119:251-267.
3. McLaren EA. All-ceramic alternatives to conventional metal-ceramic restorations. Compend Contin Educ Dent. 1998;19:307-308, 310, 312.
4. Seghi RR, Sorensen JA. Relative flexural strength of six new ceramic materials. Int J Prosthodont. 1995;8:239-246.
5. Fradeani M, Aquilano A, Corrado M. Clinical experience with In-Ceram Spinell crowns: 5-year follow-up. Int J Periodontics Restorative Dent. 2002; 22:525-533.
6. Heffernan MJ, Aquilino SA, Diaz-Arnold AM, et al. Relative translucency of six all-ceramic systems. Part I: core materials. J Prosthet Dent. 2002;88:4-9.
7. Campbell SD. A comparative strength study of metal ceramic and all-ceramic esthetic materials: modulus of rupture. J Prosthet Dent. 1989;62:476-479.
8. Luthardt RG, Holzhüter MS, Rudolph H, et al. CAD/CAM-machining effects on Y-TZP zirconia. Dent Mater. 2004;20:655-662.
9. Sorenson JA. The Lava all-ceramic system: CAD/CAM zirconium. Prosthodontics for the 21st century. Synergy in Dentistry. 2003;2(Suppl to Contemp Esthet Restor Pract):3-6.
10. Christel P, Meunier A, Heller M, et al. Mechanical properties and short-term in-vivo evaluation of yttrium-oxide-partially-stabilized zirconia. J Biomed Mater Res. 1989;23:45-61.
11. Groten M, Pröbster L. The influence of different cementation modes on the fracture resistance of feldspathic ceramic crowns. Int J Prosthodont. 1997; 10:169-177.
12. Christensen GJ. Seating nonmetal crowns or fixed partial dentures with resin cement. J Am Dent Assoc. 1998;129:239-241.
13. Schuh C, Kinast EJ, Mezzomo E, et al. Effect of glazed and polished surface finishes on the friction coefficient of two low-fusing ceramics. J Prosthet Dent. 2005;93:245-252.
a In-Ceram Alumina®, Vident, Brea, CA
b In-Ceram Spinell, Vident, Brea, CA
c In-Ceram Zirconia®, Vident, Brea, CA
d Procera®, Nobel Biocare, Yorba Linda, CA
e IPS Empress®, Ivoclar Vivadent, Amherst, NY
f IPS Empress® II, Ivoclar Vivadent, Amherst, NY
g IPS Eris®, Ivoclar Vivadent, Amherst, NY
h Lava™, 3M ESPE, St. Paul, MN
About the Author
Robert C. Margeas, DDS
Adjunct Professor, Department of Operative Dentistry
University of Iowa College of Dentistry
Iowa City, Iowa
Private Practice
Des Moines, Iowa