Material Selection Guidelines for Single-Unit Implant Crowns and Abutments
How to make choosing the ideal materials a little less difficult
This article provides guidelines for the selection of crowns and abutments for single-unit implants. With recent and continued developments in crown and abutment materials, choosing the ideal material and design for a given case can be difficult.
When selecting a single-unit implant prosthesis, the dental team should address the following four primary factors:
• Functional requirements/anticipated load
• Biologic requirements
• Esthetic requirements
• Expected abutment/screw stability
Secondary factors to consider:
• Implant angulation
• Implant depth
• Clinician skill/comfort level
• Any anticipated needs for retrieval
• Interocclusal space
Abutments
Current options for definitive abutments are as follows: titanium, zirconia, titanium base with zirconia superstructure, titanium with cast gold (UCLA), e.max (Ivoclar Vivadent, www.ivoclarvivadent.us), and alumina. The use of alumina abutments seems to have fallen out of favor since the introduction of zirconia and e.max abutments. Titanium has an extensive track record of being highly biocompatible and strong; however, esthetics remains an issue. To resolve this problem, anodizing (gold or pink hue) has been tried, but this has resulted in limited success. Attempts to address the esthetic shortcomings by placing the margins of the abutment deep subgingivally (>1 mm deep) should be avoided; an increasing number of cement-induced peri-implantitis cases has been reported.1,2
Titanium abutments are available in various stock forms or fully customized (eg, NobelProcera, Nobel, www.nobelbiocare.com; Atlantis, DENTSPLY Implants, www.dentsplyimplants.com). Stock abutments rarely follow the tissue contours of any particular case, resulting in placing margins too deep at the papilla or leaving exposed titanium at the facial.3 Custom abutments allow the cement margin to closely follow the patient’s anatomy (Figure 1). The cost of custom abutments continues to decrease, and the resulting margin positions result in cementable restorations that minimize the chance of retained cement and properly support the soft tissue architecture (Figure 2).
Guidelines for Margin Positions On All Cemented Abutments
Nonesthetic areas (posterior):
• Facial = –0.5 mm
• Mesial = –0.5 mm
• Lingual/palatal = 0.0 mm
• Distal = 0.0 mm
Esthetic areas (as determined by the patient and clinician):
• Facial = –1.0 mm
• Mesial = –0.5 mm
• Lingual/palatal = 0.0 mm
• Distal = –0.5 mm
These margin positions aid the clinician in ensuring complete and thorough removal of cement, while providing a reasonable “safety zone” for esthetics at the gingival margin. Margins deeper than 1-mm subgingival significantly increase the risk for cement retention and peri-implantitis.
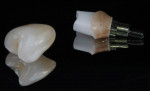
Zirconia abutments are available in two forms: solid zirconia and zirconia with a titanium insert (Figure 3) that interfaces the implant. The research to date has been inconclusive as to whether one design is less prone to breakage than the other. For peace of mind, many clinicians prefer the portion of the abutment that interfaces with the implant to have the titanium insert. However, this design is not universally available from all makers of custom abutments. Most manufacturers now offer zirconia in various shades other than the stark white. The margins for zirconia abutments should follow the above guidelines. If the proper shade of zirconia is used, margins could be placed even shallower.
e.max abutments are new to the marketplace (having just been cleared in the USA in early 2014). This product is currently available only for the Cerec systems and targeted at clinicians with in-house mills. Scant third-party research on these abutments has been conducted, and conclusions are yet to be drawn.
The use of cast UCLA abutments has proven to be successful and reliable. The three primary concerns with a cast-alloy screw-retained abutment/crown are esthetic concerns regarding the screw-access hole with angled anterior implants (Figure 4), the increasing cost of alloy, and the labor required in their fabrication. Some evidence suggests that they exhibit greater bone and gingiva loss compared with titanium.4 Screw-retained restorations (whether zirconia or cast alloy) present fairly predictable retrieval and no risk for retained cement. Under most circumstances, the retrieval of a single-unit crown is not generally needed because of more modern internal connection designs. External hex implants are significantly more prone to screw loosening,5 and as such, the clinician should expect to replace and retorque the screw during the life of the restoration.6 Cement-retained crowns can also be “marked,” indicating where the screw access would need to be drilled should the need arise.7
General Recommendations for Single-Unit Implant Abutment Selection
In most cemented cases, custom abutments should be used to ensure that margins are within 1 mm of the gingiva.
Custom titanium abutments are ideal for many single-unit posterior cases (Figure 5) (highly biocompatible and strong), or anterior cases with a low lip line and thick gingiva (Figure 6).
Shaded, custom zirconia abutments are ideal for many single-unit anterior cases (minimizes “gray” gingiva, is highly biocompatible, and addresses angled implants).
Cemented crowns should have the screw-access hole marked to aid in retrieval (Figure 7 and Figure 8).
Screw-retained restorations are ideal for single units if retrieval is planned, cement management too difficult, or interocclusal space is limited.
Single-Unit Crowns
Current options for single-unit implant crowns include porcelain fused to metal (PFM), e.max, layered zirconia, full-contour zirconia, porcelain-filled composites, and full gold. The most popular options are as follows:
PFM crowns are reliable choices for implant crowns. Their strength does not rely heavily on the choice of cement, and thus even “temporary” cements can be used with great success. PFMs can be designed with metal stops in MIP if high loads are anticipated (such as on a second molar or when opposing another implant). PFMs can be challenging esthetically, particularly along the gingival margin.
The use of e.max crowns (lithium disilicate) has proven to be highly successful on implant crowns in most cases. Some research has shown e.max crowns to be exceptionally strong on implants, in some cases rivaling the strength of layered zirconia crowns.8 They are less likely to break if a resin cement is utilized. However, extreme care must be taken to ensure that no cement is left subgingivally. This can be particularly difficult with resin cements as they tend to have low viscosity, translucency, good bonding to titanium, and nonresorption. Thus, the use of resin cements is only advisable for e.max crowns when the extra strength is needed and the margins closely follow the gingival margins. Resin cements should not be used if the margin is more than 1 mm subgingival.
Early on, layered zirconia crowns had some significant problems with porcelain delaminating. Much of this concern has been resolved with properly designed frameworks and slower cooling times.9 Layered zirconia crowns will require more occlusal clearance than a full-contour zirconia crown. Both can be cemented to the abutment, using nearly any cement on the market. Wear of the opposing teeth and restorations by full-contour zirconia crowns is still unclear. Like many types of restorations, the esthetic result of zirconia-based restoration is based on the technician’s skill set (Figure 9 and Figure 10).
General Recommendations for Single-Unit Implant Crown Selection
PFM has a strong track record and is generally a good functional choice, but is not the most esthetic.
In the past, layered zirconia has had problems with chipping, but this seems to be resolved.
e.max implant crowns are working well clinically and has recently been the subject of considerable research.
Full-contour zirconia crowns are new to the profession, but appear to be working well. It is not yet clearly known how they wear enamel. They will inevitably prove difficult to removed.
No “one” right answer can determine which abutment/crown material is right for all cases. The guidelines above are based on the authors’ clinical experience with patients, with students’ patients, and the relevant scientific literature. They should serve well in most cases, although there is significant room for personal preferences. Many cases can be treated successfully with various materials and methods.
References
1. Linkevicius T, Puisys A, Vindasiute E, et al. Does residual cement around implant-supported restorations cause peri-implant disease? A retrospective case analysis. Clin Oral Implants Res. 2012;[Epub ahead of print].
2. Wilson T. The positive relationship between excess cement and peri-implant disease: a prospective clinical endoscopic study. J Periodontal. 2009;80(9):1388-1392.
3. Chee W, Jivraj S. Designing abutments for cement retained implant supported restorations. Brit Dent J. 2006;201(9):559-563.
4. Abrahamsson I, Berglundh T, Glantz PO, Lindhe J. The mucosal attachment at different abutments. J Clin Perio. 1998;25(9):721-727.
5. Kitagawa T, Tanimoto Y, Odaki M, et al. Influence of implant/abutment joint designs on abutment screw loosening in a dental implant system. J Biomed Mater Res B Appl Biomater. 2005;75(2):457-463.
6. Pjetursson BE, Brägger U, Lang NP, Zwahlen M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin Oral Implants Res. 2007;18(Suppl 3):97-113.
7. Schoenbaum TR, Chang YY, Klokkevold PR. Screw-access marking: a technique to simplify retrieval of cement-retained implant prostheses. Compend Contin Educ Dent. 2013;34(3):230-236.
8. Martínez-Rus F, Ferreiroa A, Özcan M, et al. Fracture resistance of crowns cemented on titanium and zirconia implant abutments: a comparison of monolithic versus manually veneered all-ceramic systems. Int J Oral Maxillofac Implants. 2012;27(6):1448-1455.
9. Tan JP, Sederstrom D, Polansky JR, et al. The use of slow heating and slow cooling regimens to strengthen porcelain fused to zirconia. J Prosthet Dent. 2012;107(3):163-169.
About the authors
Todd R. Schoenbaum, DDS, FACD
Assistant Clinical Professor, Division of Restorative Dentistry, Director of Continuing Education,UCLA School of Dentistry
Los Angeles, CA
Yi-Yuan Chang, BS, MDC
Staff Research Associate, Division of Restorative Dentistry, UCLA School of Dentistry
Los Angeles, CA