Indirect Conversion Technique
Implant therapy that can be individualized for each patient
Robert Kreyer, CDT
William Perry, DDS
Implant prosthetics is a rapidly growing segment of modern prosthetic dentistry.
The demand for implant placement in edentulous patients is driven by their awareness of complete denture treatment options through media and Internet marketing. In the coming years, there is likely to be an evolution of prosthetic implant treatment options, so the practitioner should always consider what is best for the individual compromised edentulous patient.
This article presents an indirect conversion technique for immediate loading of a complete implant-supported provisional. This technique is not revolutionary, but it provides the clinician and technician with a flexible implant treatment option that can accommodate an individual patient’s prosthetic factors and variables.
Implant Prosthetic Case Planning
As with any implant prosthetic case, a successful outcome depends on the clinical and technical time invested in diagnostic planning from the beginning of the case. Understanding a prosthetic patient’s esthetic expectations and functional desires is a critical part of developing a case plan. Evaluating existing restorative space with mounted casts on a dental articulator is an essential part of the implant design process and case planning. Once these implant prosthetic variables are communicated, a diagnostic denture is created within established restorative space.
Diagnostic Denture
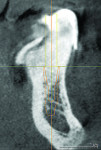
During diagnostic planning procedures, a traditional complete denture is designed and created according to the patient’s esthetic expectations and established restorative space. This diagnostic denture allows the clinician and technician to evaluate the restorative space and function of the proposed implant prosthetic treatment as a team. The diagnostic denture can also be converted to a radiographic stent for CBCT scans. Using these scans, one can plan the intraoral position of the guide pin, thus providing a reference point for vertical dimension and screw access in relation to tooth placement (Figure 1). The problem with using an existing or old denture for case planning and scanning concerns residual ridge resorption, the result of which is that denture teeth are not in their optimal position. The ideal prosthetic tooth position is in line with the vector forces of occlusion to the long axis of implant body. The best way to plan for implant placement and functional occlusion is through the use of a diagnostic denture on a semi-adjustable articulator. The waxed denture tooth arrangement is then processed, finished, and polished to include all of the hard edentulous anatomy that will provide support to the complete denture prosthesis.
Direct Implant Conversion
With the demand for implant-supported prosthetics rapidly increasing, it is necessary to examine the techniques currently being used and re-evaluate their efficiency and predictability.
The direct conversion technique for immediate loading of implants has been used widely for converting mucosal-supported dentures to implant-supported ones. The direct conversion of a complete denture provisional prosthesis can be very time consuming clinically. It is also difficult to maintain established records such as the vertical and centric plus midline esthetic relationship. The direct conversion technique is usually performed either in the operatory of the surgeon or that of a restorative dentist by a clinician and technician. Such a conversion could tie up chairtime for most of the day, costing the clinician in lost time and labor. A positive benefit of direct implant conversion for patients is that they leave after surgery with a provisional restoration.
Indirect Implant Conversion
The indirect conversion technique presented in this article offers a predictable prosthetic option that places the conversion back in the dental laboratory and provides the clinician and patient with optimal restorative implant results. The technique also maintains established occlusion of vertical dimension (OVD) and centric relation records. Since the diameter of the holes for cylinders is minimal, the strength of the provisional is not compromised.
Using the indirect conversion technique, implants are placed in a single day. The patient then goes home and comes back to the clinician’s office the next day, when the converted provisional is delivered and fitted.
After implant placement, an intraoral verification jig is made with a resin or composite bar 2 mm above the mucosal surface. For accurate transfer to the articulator, occlusal records are taken over the jig for mounting (Figure 2, Figure 3 and Figure 4). A 2 mm layer of VPS impression material is then extruded onto the intaglio surface to provide space for acrylic resin. Gypsum stone is then mixed, and a verification master cast base is created for conversion of the mandibular complete denture (Figure 5, Figure 6 and Figure 7).
The verification cast is then articulated to the mounted maxillary cast with the occlusal record (Figure 8). The verification cast intaglio surface is then analyzed as compared to the complete mandibular denture and the amount of gingival denture base that needs to be cut back is visualized (Figure 9 and Figure 10).
The vertical dimension record is then verified with the guide pin relationship (Figure 11 and Figure 12). The crest of the residual ridge is marked on the intaglio of the denture base to gauge gingival cut-back (Figure 13, Figure 14 and Figure 15). The denture is attached to the maxillary, and the intaglio is relieved according to markings on the VPS surface (Figure 16 and Figure 17). After the intaglio surface is relieved, the OVD is verified by maintaining incisal pin contact (Figure 18).
A hard VPS matrix is made for the denture by extruding heavy-body material around the labial, buccal, and lingual surfaces for relining of the intaglio surface (Figure 19, Figure 20 and Figure 21).
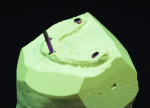
Guide pins are then screwed into implant model analogs, allowing the denture to line up to the milling machine when drilling screw access holes (Figure 22, Figure 23 and Figure 24).
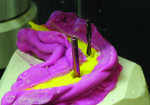
Temporary cylinders are then measured, cut, and screwed into place according to the guide pin paths and relieved denture base surface (Figure 25 and Figure 26).
The cut-back denture is then placed over the cylinders and into the matrix with guide pins screwed into place (Figure 27 and Figure 28) The denture is now relined, and the technician may attach temporary cylinders and create a convex intaglio surface (Figure 29 and Figure 31). Finally, the provisional implant-supported prosthesis is finished, polished, and delivered to the patient. (Figure 32 and Figure 33).
Summary
There are many modifications of the direct and indirect conversion techniques that include capturing implant placement with a quick impression, creating a fast master cast, and doing the conversion on a cast or in the mouth. A clinician or technician may choose a combination of both techniques, allowing most of the conversion to be done out of the intraoral environment. The trick is to select the best conversion technique based on the clinical implant restorative plan and the patient’s expectations and desires.
About the Authors
Robert Kreyer, CDT
Partner
Custom Dental Prosthetics Inc.
Los Gatos, CA
William Perry, DDS
Owner
Private Practice
Los Gatos, CA