Implant Restorative Space
Developing the best solution through team communication
Every Chicago Midwinter meeting brings forth new products, innovations, and attendee’s pure passion for prosthetics. This year in Chicago, dental technician Renzo Chiappe presented an innovative implant prosthetic technique he developed with Dr. Noel Pilie who owns a practice in New Orleans, Louisiana. The innovative prosthetic technique showcased in this article created a tremendous buzz during the dental laboratory meetings that weekend.
The key to innovation is to understand a need and provide a solution to the market. Through communication and collaboration between the clinical and technical team of Dr. Pilie and Renzo Chiappe, they designed and created a new protocol for a predictable profile with immediate loading of an All-on-4® (Nobel Biocare, www.nobelbiocare.com) or more implant prosthesis. A brief introduction of their protocol for a predictable profile is presented in this article.
Implant Perspective
The All-on-4 (or 5 or more) procedure is a very advanced, sophisticated reconstruction of a major part of the anatomy of the stomatognathic system. It commonly involves extraction of teeth, surgical bone and gingival tissue removal, placement of multiple dental implants, and then replacement of bone, gingiva, and at least a complete arch of teeth with artificial material that must be compatible with the oral environment. Frequently both upper and lower arches are replaced simultaneously. It must look good, feel good, and not cause any adverse effects on the patients jaw joints, jaw bone, muscles, gingival, or muco-buccal tissues. The complete oral reconstruction is performed by a medical team consisting of the restorative dentist, surgeon, and dental laboratory technician.
The resulting prosthesis is different from most complete occlusal rehabilitation cases where the success or failure is primarily dependent on the knowledge and skills of the restorative dentist alone. The patient’s teeth from the gum up are rebuilt and the tooth roots and periodontium absorb the occlusal stresses caused by chewing and parafunctional activity. The laboratory technician builds the crowns according to the dentist’s prescription. The adaptability of the stomagnathic system with its unique periodontal ligament proprioception and neuromuscular protection of teeth, bone, joints, and muscles saves the restorative team and the patient, in many instances, by reducing excessive force on these structures. Problems that occur or that are incipient or those that take some time to become symptomatic, may not be diagnosed as related to failure of the prosthesis to fulfill certain guidelines.
Lacking periodontal ligaments, implants, and implant restorations do not enjoy this same auto-protection against excessive forces. Uncontrolled adverse pressure can result in damage to the prosthesis or even be fatal to one or more implants.
The All-on-4 prosthetic concept is quite different than the dentate occlusal rehabilitation and is unique in many ways. As pointed out, it is a reconstruction and replacement of the patient’s alveolar ridge, gingiva, tooth support structure, and teeth. It always involves facial and dental cosmetics, phonetics, and masticatory function. It is further made unique by the fact that a surgeon is involved performing a major portion of the services. To a great extent the success or failure of the entire prosthesis is dependent on his skills and knowledge as well as the restorative dentist’s. Then dental technicians must add the unique and new nature of the laboratory work necessary to support them by providing a prosthesis that fulfills all of the parameters prescribed. We must recognize the skill and art contributed by the laboratory technician in supplying a product that meets the patient’s needs and cosmetic wishes and can be delivered in a predictably successful and efficient manner.
Each member of the dental care team, the surgeon, the restorative dentist, and the laboratory technician, has a unique set of skills and is dependent on the other for successful case outcome. Each should have an understanding of the other’s work and the challenges they face in performing their part of the treatment. Only then can we support one another in order to bring the case to a successful and stress-free completion.
The work being performed cannot be carried out independently but must be planned and performed in concert. Each team member should do his or her part competently and completely and not depend on the other to perform a procedure that is not specifically within the skill set or training to perform.
In short, each team member is as important as the other, and, if one is lacking in skill or knowledge, it can lead to a complication in performing a procedure and even compromise the ultimate outcome. The entire case can be jeopardized and ultimately one or more components may fail and everyone suffers, especially the patient. So let us keep in mind that as healthcare professionals it is the patient’s best interest and wellbeing that should drive us in this endeavor.
The goal is for each team member to continue to strive to increase the skills and knowledge of the utilization of implants and the concept and principles of complete dentistry so as to best perform this life-changing treatment for our patients in a seamless and predictably successful manner.
Implant Space
As in all prosthodontic procedures the case begins with the patient, and understanding their esthetic needs and expectations through visual observation and digital photography. After the master casts have been created and mounted according to clinical relationship records the restorative space needed is evaluated.
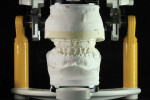
Measurements and calculations are made to determine proper bone reduction after extraction of remaining dentition. The space calculation is determined from the 10-mm tooth, the 4-mm bar, and 4-mm wrap around acrylic. It is determined that 15 mm on the anterior and 13 mm on the posterior sector are needed or the final restoration (Figure 2 through Figure 5). This bone reduction measurement will guide the clinical and technical restorative team in the design and fabrication for this immediate-loaded implant prosthesis. A silicone putty occlusal registration should always be created before master cast surgery to remove teeth, tissue, and bone (Figure 6). This will provide a reference point in case one needs to verify the starting point at anytime. The master cast is then sectioned and removed (Figure 7 and Figure 8).
Implant Esthetics
A baseplate is then fabricated and denture teeth arranged in wax according to the patient’s esthetic needs (Figure 9 through Figure 12). The wax is built up on the lingual with posterior stops for occlusal vertical dimension (OVD) and a bite jig, representing a record of tooth positions, is made (Figure 13 through Figure 15). Posterior teeth are removed from the wax baseplate in areas where implants will be placed by the surgeon (Figure 16). This will provide access to implants. The teeth will then be cold-cured in place using a bite jig for tooth placement.
Figure 17 and Figure 18 show a processed maxillary and mandibular with labial and buccal inspection windows to verify the properly calculated level of bone reduction. Note on the maxillary that the labial and buccal inferior portion of inspection window is at the bone level of the silicone putty master cast that was created in intaglio after processing and finishing the implant prosthesis. Figure 19 and Figure 20 show a labial and occlusal view of the surgical guide this surgeon used, allowing adequate space for implant placement.
Implant Expectations
In the end the patient’s prosthetic needs and desires are exceeded with this immediate-loaded, temporary implant restoration (Figure 21). A final or definitive implant supported All-on-4 restoration is then made at the second stage of the rehabilitation with proper gingival base contours representing accepted pontic design and protocol (Figure 22).
Implant Collaboration
Implant prosthetic treatment requires a multidisciplinary approach for design and case planning if dental technicians are to exceed esthetic and functional expectations with these complex restorative cases. Develop a restorative team to observe and communicate implant prosthetic variables that will provide optimal implant treatment for a compromised patient.
Acknowledgment
The authors would like to thank Steve M. Cambre, DDS for providing the case and photography. For more information on the technique presented, contact Renzo Chiappe at rechiappe@hotmail.com.
About the authors
Robert Kreyer, CDT
Partner
Custom Dental Prosthetics Inc.
Los Gatos, California
Renzo Chiappe
Owner
Chiappe Dental Lab
Covington, Louisiana