No-Preparation Veneers to Enhance the Natural Tooth
Why this is a viable and esthetic option for today’s patient.
As we all know, preparation design can make or break a case. With proper planning and preparation design, we can create stunning esthetics with depth and vitality. Without it, the best we can do is usually an over-contoured, manufactured-looking restoration. The same can be said about no-preparation dentistry—even though we are looking to nature to provide our preparation design instead of the dentist.
Nature produces a variety of tooth shapes and arrangements within the display of the lips and the face of the patient. In many cases, a patient’s smile requires a greater tooth presence due to small teeth, large lips, or tooth position. The author believes that it is the responsibility of dental professionals to recognize and diagnose these patients searching for cosmetic enhancement in the most non-invasive way. Case selection is critical and can determine success or failure. However, case selection is most critical when presented with no-preparation cases. The author feels there should be no compromise of esthetics in treating patients without any tooth preparation as long as both the dentist and ceramist work together as a team. In this article, we will look at how the author fabricates no-preparation veneers for the most esthetic outcome, the thought process behind selecting porcelains, and what to look for in diagnosing a no-preparation case.
Case Presentation 1
The patient was a 15-year-old girl with a promising career in the entertainment industry. She was moving to Hollywood and felt that her smile could use some improvement. She wanted the spaces between her teeth closed and a brighter, fuller smile (Figure 1 and Figure 2). The patient already had a good amount of tooth display in repose so we did not want to lengthen her teeth (Figure 3). Because of her age, the dentist did not want to prepare her teeth and, therefore, requested that we proceed with no-preparation veneers.
Creating Prototypes
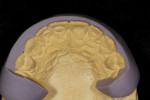
The first step in any smile design case is to create prototypes. Prototypes serve several purposes. First, they allow the patient and the dentist to preview the new smile both esthetically and functionally. Second, they show if and where any enamel reduction is needed. Third, they are used for shade communication between the patient, the dentist, and the ceramist. Prototypes can be created with bisacryl temporary material by using a diagnostic wax-up and a silicone matrix, as was done in this case (Figure 4 through Figure 7), or by hand sculpting directly in the patient’s mouth with composite. Each of these techniques has benefits and drawbacks. When the dentist fabricates the prototypes directly in the patient’s mouth they are able to get direct feedback from the patient as they are working. The laboratory technician does not have the benefit of communication with the patient or the added value of the face and lips as a guide. In cases that are extremely thin, the author has found that a bisacryl transfer will not last very long in the patients mouth due to lack of retention. Once the patient and the dentist have approved the design, an impression is taken and sent to the laboratory along with a photographic series for communication. Models are created, and platinum foil is adapted to the dies by means of tweezers, an orange wood stick, and a swager (Figure 8 through Figure 10). The laboratory technologist then fabricates a silicone matrix from the model of the prototypes to show the amount of space needed for the ceramic (Figure 11 through Figure 14). Using these tools, the ceramist is able to see how much room he has from the tooth to the final desired contour. This information is critical in determining which porcelains to use and how much opacity or translucency is needed on each individual tooth.
Porcelain Layering
First, a wash bake is applied to the foil, and the foil is readapted to the die to ensure a good fit. Translucent porcelains are used in the gingival, incisal, and interproximal zones in order to blend into the natural tooth (Figure 15). Subsequent porcelain is applied and fired to achieve the desired effects and contour (Figure 16). Colored pencils and metallic paste are used to verify and establish line angles and surface anatomy (Figure 17 and Figure 18). Surface texture and final contours are reached using various rotary diamond instruments. Once the desired contour and surface morphology are achieved, the veneers are brought to a natural glaze and manually polished using a series of rubber wheels and diamond polishing paste. Finally, the foil is removed from the veneers with sharp-pointed tweezers. Because the veneers are very thin, 0.02 mm, the ceramist must be extremely careful while removing the foil (Figure 19). After the foil is removed, marginal adjustments are made with a rubber wheel. Here you can see the amount of translucency and subtle opacity built into the veneers (Figure 20). Once the veneers are placed back on the model, we can see how much they will be influenced by the underlying tooth color (Figure 21 through Figure 25). Using translucent cement, the veneers are placed immediately after bonding (Figure 26 through Figure 28).
Porcelain selection is critical for no-preparation cases. If the proper porcelains are not chosen, the veneers can be very opaque and flat looking or too low in value. The technician should note the effect of too much translucency and too much opacity. In this case, the one where we made more than 50 veneers to evaluate the effects of shade and value on a natural tooth, more than 50 veneers were made on tooth No. 9 to evaluate the effects of value and shade on a natural tooth. We learned that if too much opacity is added, the margins will be visible and there is little light transmission from the tooth. On the other hand, if there is too much translucency, the entire tooth becomes visible and the value is lowered. Therefore, semi-colored translucent porcelain must be added in marginal and interproximal areas and more opaque porcelain should be blended to mask out undesirable colors and brighten the tooth. If any length is added it must be blended so as not to have an immediate shift in color or value from the tooth to the unsupported porcelain in the veneer. We also learned that the original color of the tooth can be drastically changed and brightened and that dark-colored teeth can be blocked out if the patient desires (Figure 29 through Figure 31). Many times when a patient presents with severely discolored teeth, the ceramist can fabricate a prepless veneer on a single anterior tooth so the dentist and the patient can verify that the final shade can be achieved without any significant cost. This creates a very comfortable situation from which to proceed (Figure 32 and Figure 33).
Case Presentation 2
The patient was a teenaged girl who was unhappy with her smile and felt her teeth were too small. She wanted a more grown-up smile. In our evaluation, both the technician and the dentist felt that her centrals were an appropriate size for her smile but that her laterals and cuspids were lacking. A diagnostic wax-up was fabricated to confirm our suspicions, and the patient approved it. The technician fabricated no-preparation veneers on teeth Nos. 6, 7, 10, and 11. Special consideration was given to the contours and characterization of the veneers in order to blend with her natural teeth and create harmony in the smile (Figure 34 through Figure 39).
Case Presentation 3
This patient wanted a brighter smile but also one that was more full and closed up some of the spaces (Figure 40). The dentist began this process with an intraoral mockup. By hand-sculpting the prototypes, the dentist was able to get real-time feedback from the patient about the overall architecture and color. This information was critical, as it would become the most important tool of communication between the dentist and the ceramist (Figure 41).
After the prototypes were approved, the dentist took an impression and sent it to the ceramist. The ceramist created two silicone matrices (Figure 42 and Figure 43), which served as a guide for how much room there was for porcelain application (Figure 44 and Figure 45). Without this information it would be very difficult for the ceramist to plan which porcelains he would need to create the final restoration with proper translucency and color. The ceramist then fabricated the veneers with internal characterization to enhance the natural tooth (Figure 46 through Figure 49). Finally, the veneers were placed and the patient was extremely happy (Figure 50 and Figure 51).
Conclusion
There is a lot of misleading information in the dental profession about what can or cannot be accomplished with no-preparation veneers. After fabricating more than 10,000 no-preparation veneers, the author feels they are important tools to incorporate into your business. When diagnosed correctly and fabricated properly, no-preparation veneers can be the most esthetic, cosmetic enhancement option for patients today.
Acknowledgment
The author would like to thank Dr. Dennis Wells and Dr. Gordon West for their contributions to this article and for their commitment to esthetic dentistry.
About the Author
Mark Willes
Owner
Experience Dental Studio
Lindon, Utah
This case was also the Kois Center “Case of the Month” featured in the June 2011 issue of Compendium. Find it online at dentalaegis.com/go/idt37