Auto-Polymerizing Resin: an Aid to Master Model and Die Creation
How to avoid die breakage when fabricating thin, single-preparation dies.
Craig A. Pickett, RG, CDT
One frustration that technicians often face is an anterior preparation impression that is too thin and tiny to pour in die stone. On each attempt to create a die, the die breaks while removing the cast from the impression. After numerous tries, either the impression itself or the margins on the impression become worthless.
Seeking a “harder” die stone that will not break upon removal is a common mistake at this point. In their search, some technicians turn to the physical properties chart supplied by their gypsum manufacturer and look in the compressive strength column for the largest number they can find or in the ISO column for the next largest gypsum type number. Both of these bits of information are useful when applied properly, but misapplication can cause even greater problems for technicians and their clients.
Breaking it Down
The comparative difference between Type 4 and Type 5 die stone may be improved compressive strength. However, there is always increased expansion. In the ISO 6873 standard, Type 4 stones have a maximum of 0.15% expansion compared to the minimum 0.16% expansion of Type 5 stones. That difference results in fit changes in the clinical setting.
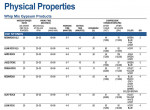
Large numbers in the compressive strength column (Figure 1) are generated when the gypsum is in the “dry” state or some time at or after 48 hours, which is the ISO standard. Some manufacturers, such as Whip Mix Corp, use a reporting time frame that is exactly 48 hours; others wait a longer time period. The longer the gypsum material continues its crystal growth, the larger the compressive numbers. However, no technician has the luxury of waiting 2 or more days for models to develop this load strength, especially when it is not the root of the problem.
The true cause is physics. The material’s ability to resist compressive forces is not used when pulled from an impression. The stone is expected to be flexible and bend without breaking, which is a test of tensile strength (Figure 2). Gypsum does not possess good tensile strength and therefore breaks when it is put under pressure to flex.
It is possible to combine different materials and get the best of both worlds. Nelson Gendusa, DDS, documented the process of producing a working pattern from DuraLay resin (Reliance Dental Mfg Co, www.reliancedental.net) using a concept created by Allen L. Weiner, DMD, PC, to create a crown under an existing removable partial denture (RPD) without patient surrender of the RPD.1 This same material and combination technique can be used to solve the gypsum breakage problem.
Several pattern resins are now available on the market, each with their own working characteristics and colors. The linear contraction properties of these materials vary. It is recommended that technicians choose a pattern resin that exhibits contraction numbers that are approximately the same as or less than the die stone used. DuraLay reports a linear contraction of 0.013% to 0.028% when mixed at a two-thirds polymer to one-third monomer ratio.2 It is best to select an auto-polymerizing resin that is comfortable to work with and incorporates a color choice that enhances marginal definition.
Step By Step
First, a single master die should be poured from the appropriate Type 4 or Type 5 die stone. These dies are generally retrievable without breakage when the technician is not working against an entire arch or quadrant. If there is an undercut in the impression that was not blocked out by the dentist prior to capture, a portion of the impression material should be removed to facilitate ease of die removal.
After die removal, the remainder of the undercut on the master die should be blocked out. The gypsum die stone should set a minimum of 30 minutes before separation from the impression.3 The reported “set time” is an initial set and not the “ready for use” time.
If there is need for die reinforcement, the DuraLay Plastic Pin can be used (Figure 3). This is a tapered and serrated pin that enhances insertion into a narrow space and aids in retention. Often a brass dowel pin or a piece of a paperclip is used for reinforcement. However, the use of either causes vibration in the die during trimming, especially when struck by a bur, and may cause pieces of the gypsum die surrounding the metal surface to flake or split.
The appropriate separator should be used sparingly to prepare the impression for the auto-polymerizing resin. Over-application of heavy petroleum jelly products should be avoided as they can reduce the clarity of the reproduced die and interfere with the crystal growth of the gypsum.
The pattern resin should be pre-mixed in a ratio of 2:1 powder to liquid or the DuraLay brush method (www.reliancedental.net/Instruction_Sheets/DuraLay) can be employed by dipping the tip of a small brush moistened with monomer into the polymer powder and retrieving a small ball of resin (Figure 4). This same method can be used for most of the resins available.
A tiny ball of wet resin should be placed in the impression of the preparation and the technician must ensure that it travels to the very tip of the preparation and traps no air bubbles. It is possible to add a small brush tip full of monomer to ensure that it moves freely or to use a dental instrument as an aid.
It should be built, drop by drop, until the preparation portion of the impression is one-third full. If reinforcement is being used, the post should be inserted at this point, and then filling should be continued until the marginal area is covered to a minimum depth of 2 mm and the post of the reinforcement is extending vertically through the center of the preparation.
Once the resin is partially cured, then a “mushroom-shaped” mass of resin can be built around the post and on top of the marginal area (Figure 5). This mass will serve as mechanical retention in the gypsum. To increase retention, undercuts can be created by carefully cutting into the resin mass with a disc or bur or by placing additional balls of resin in random areas of the buildup. The resin should not be pulled to check adaptation prior to pouring die stone as it might not return to its proper alignment.
Once the resin has completed its manufacturer-specified set time and the correct water/powder ratio is used, the die stone should be mixed and poured into the impression, fully encasing the resin mass. In this case, Resin Rock Type IV (Whip Mix Corp., www.whipmix.com) was used. Very low vibration should be used during the pour to ensure that the pattern resin is not dislodged from the impression and subsequently captured in an improper position.
After the stone has set a minimum of 30 minutes, the cast can be removed from the impression. The cast should be pinned and based for die separation or mounted to an appropriate articulator as a solid model (Figure 6). The marginal area of the resin die also should be trimmed to ensure ease of transfer between the master die and solid working cast.
It is important to be familiar with the physical properties and restrictions of the materials being used in the restorative process. Knowing the limits and finding alternative solutions helps reduce the frustration that can result from using materials in applications far beyond their physical capabilities.
References
1. Gendusa N. How to fabricate a new crown that fits an existing RPD … without forcing the patient to surrender the partial. Parkell Today: Special Report #46. https://www.parkell.com
2. Osterle M [doctoral research]. Berne, Switzerland; 1960.
3. Anusavice KJ. Phillips’ Science of Dental Materials. 11th ed. St. Louis, MO: W.B. Saunders; 2003: 263.
Disclaimer
The preceding material was provided by the manufacturer. The statements and opinions contained therein are solely those of the manufacturer and not of the editors, publisher, or the Editorial Board of Inside Dental Technology. The preceding is not a warranty, endorsement, or approval for the aforementioned products or services or their effectiveness, quality, or safety on the part of Inside Dental Technology or AEGIS Communications. The publisher disclaims responsibility for any injury to persons or property resulting from any ideas or products referred to in the preceding material.
For more information, contact:
Whip Mix Corp.
800-626-5651
www.whipmix.com
info@whipmix.com
About the Author
Craig A. Pickett, RG, CDT
Technical Support Manager
Whip Mix Corp
Louisville, Kentucky