The First Line of Defense Against Obstructive Sleep Apnea
How to read the signs
Obstructive sleep apnea (OSA), on average, affects 25% of a regular patient base with most of these cases being undiagnosed. OSA not only causes fatigue in these patients but also can be the source of dental and overall health issues.1
As a member of the team, dental assistants play a major role in fighting this disease. Noticing simple signs and symptoms can help dental assistants to give their patients not only great oral health but also better overall health.
What is OSA?
OSA affects more than 18 million people in America. Apnea literally means “without breath.” Those who have OSA experience lapses in breathing during sleep. These episodes are commonly caused by the muscles in the jaw and throat relaxing too much, allowing the soft tissues and mandible to fall back and obstruct the airway. The body is “screaming” at the brain to wake up in order to restart breathing. Most of the time, patients do not even remember waking up. These lapses in breathing during sleep are essentially suffocation.2
A patient with mild OSA would have 5 to 15 apneic episodes per hour; a patient with a moderate case would be experiencing 15 to 20 episodes per hour; and a patient with a severe case would have 30 or more episodes per hour. Some patients may experience 100 episodes per hour; some episodes may last more than a minute.2
Signs and Symptoms of OSA
The overall health signs of OSA include gasping during sleep, loud snoring, frequent urination, chronic fatigue, diabetes mellitus, cardiac disease, depression and poor concentration. Studies have shown that OSA may cause Alzheimer’s disease, dementia and memory loss as well. The dental signs are pitting from gastroesophageal reflux disease (GERD), tooth wear from bruxism, scalloped tongue, enlarged tonsils and enlarged tongue—all signs that can be easily spotted during routine appointments.
Other signs and symptoms may include3:
Diagnosis
OSA is diagnosed with an overnight sleep test, which may be the use of a polysomnography (PSG) or a home sleep testing unit.
A PSG is used to help diagnose all types of sleep disorders, including OSA. A PSG is usually conducted in a sleep laboratory at a local hospital or sleep center. In this test, a sleep technician places electrodes on the patient’s body in order to record brain waves, blood oxygen levels, heart rate, and breathing rate, as well as eye and leg movements during sleep. The sleep technician records the frequency and severity of the episodes and later, a sleep physician will read the results and make a diagnosis. In many cases, the results of a PSG are not exact due to patients’ discomfort from being connected to machines and not being in their own beds.
The other option—home sleep testing—involves use of a home sleep testing (HST) unit, which is provided by either a primary care physician or, in some states, a dentist. The HST unit is a small box that patients put on themselves which then records brain waves, oxygen levels and even heart rate. Once the patient returns the unit, the results are downloaded and sent to a sleep physician who will read them and make a diagnosis. Many healthcare professionals find this to be the preferred means of testing due to high rates of accuracy and higher chances of patient compliance.
Risk Factors
OSA can affect anyone, no matter body type or health practices. Certain factors can be indicators that a person may have OSA. These include3:
Neck size—A neck circumference more than 17 inches (43 centimeters) for men and 15 inches (38 centimeters) for women is associated with an increased risk.
Having a narrowed airway—Enlarged tonsils or adenoids and a narrow airway can be genetic.
Obesity—Fat deposits around the upper airway may cause the airway to collapse.
Having chronic nasal congestion—OSA is twice as common in those who have consistent nasal congestion at night, regardless of the cause.
Being male—In general, men are twice as likely to have OSA.
Being black, Hispanic, or Pacific Islander—Among people younger than 35 years, OSA is more common in African-Americans, Hispanics, and Pacific Islanders.
Being postmenopausal—The risk in women may increase after menopause.
Having diabetes—The condition is three times more common in people who have diabetes. Diabetes and heightened insulin levels are often symptoms of OSA.
Having high blood pressure (hypertension)—OSA is common in people with hypertension, which is often the result of undiagnosed OSA, as well.
Being older—OSA occurs two to three times more often in adults older than 65 years.
Having a family history of sleep apnea—OSA can be genetic.
Using alcohol, sedatives, or tranquilizers—These substances relax the muscles, including those in the throat.
Smoking—Nicotine can cause muscle relaxation.
Treatment
Currently, four treatments are used: weight loss, surgery, continuous positive airway pressure (CPAP) and the use of oral appliances.
Weight loss will effectively reduce the pressure on the outside of the throat, preventing collapse. However, patients with OSA may have difficulty losing weight. During an apneic episode, the body releases insulin and adrenaline, creating a “fight or flight” mode in which the body holds onto all possible resources, including fat, to survive. In patients with chronic OSA problems, weight loss can be a challenge.
The surgical options for OSA treatment are often painful and invasive and do not guarantee success. The types of surgeries include the removal of the tonsils and adenoids and correction of a deviated septum. The most common procedures are:
Uvulopalatopharyngoplasty—The removal of tissue from the rear of the mouth and top of the throat.
Maxillomandibular advancement—The upper and lower parts of the jaw are moved forward from the rest of the facial bones. This enlarges the space behind the tongue and soft palate, making obstruction less likely.
Pillar implants—This is a minimally invasive treatment that involves placement of three tiny polyester rods in the soft palate. These inserts stiffen and support the tissue of the soft palate and reduce upper airway collapse and snoring.
Positive airway pressure therapy is the gold standard with the most common type being CPAP. When a patient uses CPAP, or any type of positive airway pressure therapy, the air pressure being delivered to the inside of the airway keeps the upper airway passages open. This prevents obstructive apnea and snoring but prevents collapses in the throat. Although CPAP is the most commonly prescribed method of treatment for OSA, most patients cannot tolerate it due to discomfort issues associated with the mask, high levels of air pressure and restrictions on sleeping positions.
Oral appliance therapy involves the selection, fitting and use of a specially designed mouthpiece that maintains an open airway when worn during sleep. There are two kinds of oral appliances: custom and over-the-counter. Custom appliances are proven more effective and more comfortable than
over-the-counter devices, which have a higher chance of side effects, such as tooth movement or temporomandibular disorders.4
Oral appliances are made by dentists who have received special training in dental sleep medicine. These dentists are comfortable with using a wide range of oral appliances, as there are more than 140 on the market today and can help determine which is best suited for the patient’s specific needs. Some advantages of using oral appliance therapy include being4:
- Comfortable and easy to wear. Most people find that it only takes a couple weeks to become acclimated to wearing the appliance.
- Small and convenient. This makes them easy to carry when traveling.
- Reversible and noninvasive.
Oral appliances are used to help treat mild-to-severe sleep apnea cases by repositioning the lower jaw, tongue, soft palate and uvula; stabilizing the lower jaw and tongue; and increasing the muscle tone of the tongue.
Oral Signs
A dental assistant should be able to easily spot the oral signs of the condition. Heavy bruxism, GERD and higher Mallampati classification rating are some of the most obvious dental signs of OSA. If a patient is frequently cracking porcelain crowns or is using a device to prevent bruxism, there is a high chance that the patient also has OSA. During an apneic episode, the patient often clenches and grinds the teeth in order to wake up and resume breathing, possibly resulting in TMJ disorder and tooth wear. Chances are that at least 75% of the mouth guards being made for patients should be oral appliances for OSA.
GERD or acid reflux is another common symptom of OSA. When breathing becomes obstructed, the muscles in the throat and windpipe tighten. This can cause stomach acid to be pushed into the throat and mouth, potentially corroding the teeth. Patients who report chronic acid reflux despite using antacids are most likely to have undiagnosed OSA.
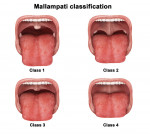
A simple physical trait indicative of OSA is the patient’s Mallampati classification (Figure 1). Patients with Class 3 or Class 4 Mallampati classification are most likely to have some degree of OSA due to the small space in the throat for the passage of air.
Regularly talking to patients about OSA during all appointments will help to raise awareness for both the patient base and the office. This simple practice could help save lives. Adding a simple screening questionnaire, such as the Epworth Sleepiness Scale (available online at https://epworthsleepinessscale.com), to regular appointments can help to identify patients who may have OSA.
Advice for Patients
If a patient is not receptive to therapy for his or her OSA, the oral healthcare professional can suggest some lifestyle changes that may help to control apneic episodes3:
- Lose weight—Weight loss can help to relieve constriction of the airway.
- Avoid use of alcohol and medications such as tranquilizers and sleeping pills—These are muscle relaxants that can interfere with breathing.
- Sleep on your side or abdomen rather than on your back—Patients who sleep supine or on the back can have blockages in the airway from the tongue and soft palate resting against the back of the throat. Positional therapy is one way to prevent sleeping on the back. Some patients sew a tennis ball onto the back of their pajamas to prevent rolling supine.
- Keep your nasal passages open at night—If the patient has chronic nasal blockage, suggest using a saline nasal spray to help keep the passages open.
1. Obstructive sleep apnea. Wikipedia Web site. https://en.wikipedia.org/wiki/Obstructive_sleep_apnea. Accessed September 8, 2011.
2. Hiestand DM, Britz P, Goldman M, Phillips B. Prevalence of symptoms and risk of sleep apnea in the US population: Results from the national sleep foundation sleep in America 2005 poll. Chest. 2006;130(3):780-786.
3. Obstructive sleep apnea. Mayo Foundation for Medical Education and Research website. https://www.mayoclinic.com/health/obstructive-sleep-apnea/DS00968. Accessed September 8, 2011.
4. Patient resources. Oral appliances. American Academy of Dental Sleep Medicine website. https://www.aadsm.org/oralappliances.aspx. Accessed September 8, 2011.
About the Author
Larry Twersky
CEO
1-800-snoring
Los Angeles, California