Image-Guided Implant Surgery in Today’s Clinical Practice
Careful treatment planning and guide stability are essential to success
Implant dentistry is entering its second half-century having gained a strong foothold as a predictable means of tooth replacement. Today, the focus on osseointegration is diminishing and the emphasis on nature-like tooth replacement, minimally invasive surgical and restorative techniques, and efficiencies of time and cost is increasing. To accomplish these goals, implant position can no longer be based solely upon bone availability, but rather should be guided by the desired prosthetic outcome—what has been termed “crown-down” approach to treatment planning and implant positioning. With the end result in mind, the surgeon is expected to place the implant in the appropriate position, at a reasonable and safe depth, and with proper angulation to facilitate efficient, lifelike tooth replacement.
Risks associated with malpositioned implants include functional and esthetic problems. Buser and colleagues point out that a successful esthetic outcome can only be achieved with “an ideal implant position in all 3 dimensions.”1 They describe proper implant position as a zone within the buccolingual, mesiodistal, and apicocoronal dimensions, rather than as a specific point. By positioning the implant within these “comfort zones,” it is predictable to achieve a functional and esthetic outcome. A violation of the comfort zones may result in complications such as peri-implant bone resorption followed by soft tissue recession and esthetic failure. Presurgical, crown-down digital planning in conjunction with guided implant surgery is an ideal means to accurately and precisely position an implant within the comfort zone and avoid potential complications.
Collaborative Care
Image-guided surgery is a technique in which preoperative diagnostic imaging, typically a cone-beam computed tomograph (CBCT), is merged with computer-based planning tools to facilitate surgical and restorative plans and procedures.2 In practical terms, patients typically have a CBCT preoperatively with or without a radiographic template in place. The radiographic template outlines the proposed ideal prosthetic outcome relative to anatomic structures and topography. This is particularly useful in patients with a deranged or partially or completely missing dentition.
The images are then imported from the CBCT files into one of many commercially available implant planning software programs. The surgeon and restorative dentist can then collaborate in choosing the precise position, angulation, and depth of implant placement, as well as the implant type, based upon a desired prosthetic outcome. Rosenfeld and colleagues3 coined the term “collaborative accountability” to describe the pretreatment analysis and subsequent negotiated compromises between surgical and restorative colleagues on implant positioning and restorative design based upon anatomic limitations and the team’s willingness and ability to overcome them. Additionally, this pretreatment evaluation is invaluable in creating realistic patient expectations.
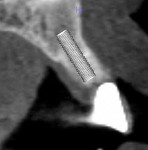
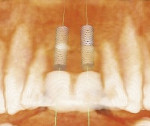
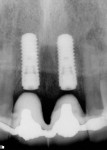
Figure 1 through Figure 7 illustrate a case from three-dimensional (3D) presurgical planning through radiographic evidence of the plan’s execution and 2-year follow up. As a result of 3D planning and subsequent guided implant surgery, the patient has a pleasing, natural looking esthetic outcome.
Higginbottom and Wilson4 described an elegant technique to fabricate a 3D acrylic surgical guide based upon a tooth set-up and ensuing radiographic stent. They used a diagnostic template to provide “a projection of the final restoration” incorporating “radiographic markers for exposing radiographs when the template is placed in the mouth.” Then they used a surveyor table and drill press to create holes in their templates, mimicking the proposed implant position confirmed by the radiographic stent.
Computer-Assisted Implant Surgery
CAD/CAM—a computer-aided technology used to design and manufacture various components2—is ideally suited to produce anatomically accurate models and design and fabricate implant surgical guides.5 Unlike their analog predecessors, CAD/CAM surgical guides precisely and seamlessly transfer the digital plan to clinical application and placement. Ozan and colleagues point out that the introduction of CAD/CAM surgical guides “has accurately allowed the transfer of planning information to implant placement.”6
With that in mind, guided implant surgery offers a number of supposed advantages to achieve these goals, including reduction of grafting requirements by optimizing available bone volume; the option of flapless surgery; reduced morbidity; avoidance of anatomic complications; the possibility of providing implant therapy where complex anatomy previously precluded treatment; improved accuracy of implant placement to improve prosthetic outcome and facilitate prefabrication of the prostheses; increased surgical precision, thereby improving implant survival rates; and use as an additional teaching tool.7
Guided implant surgery seems to have many clinical advantages. What are the shortfalls of guided implant surgery in clinical practice? Do CAD/CAM surgical guides provide an accurate means to reproduce the presurgical digital plan in the mouth?
In a recent systematic review, Jung and colleagues7 examined 19 studies investigating the accuracy of computer-assisted implant dentistry. In all, they examined nine computer-assisted implantation systems with more than 1,300 implant positions measured. When examining systems using computer assisted implant planning and surgery, they found an “overall mean error at the entry point of 0.74 mm…with a maximum of 4.5 mm, while the mean error at the apex was 0.85 mm with a maximum of 7.1 mm.”7 Specifically, they reported that the systems using milled surgical guides had a mean error at the entry point of 1.12 mm with a maximum of 4.5 mm. At the apex, the same guides had a mean error of 1.2 mm with a maximum of 7.1 mm. These findings run in stark contrast to expectations. Conversely, in an in vitro study of flapless implant surgery performed by clinicians of varying experience, Van de Velde and colleagues found implant placement to be inaccurate when performed freehand, without the use of a digitally generated surgical guide.8
By contrast, dynamic intraoperative navigation systems that reproduce the virtual implant position in real time and allow intraoperative changes in implant position2 had a mean error at entry point of 0.62 mm with a maximum error of 3.4 mm. The same systems demonstrated a mean error of 0.68 mm at the apex with a maximum error of 3.5 mm. Dynamic navigation systems have largely been abandoned because of the cost of implementation. Nonetheless, it is interesting that they are more accurate than CAD/CAM surgical guides. This is due to the fact that if an error is encountered during the drilling process using a dynamic guide, the clinician can recognize the issue in real time and make adjustments as needed. By contrast, when using a CAD/CAM guide, clinicians, particularly those with less experience, may not recognize an inaccuracy in osteotomy position, inclination, or depth. This is consistent with Hinckfuss and colleagues’ conclusion that "surgical guide design, surgeon’s experience, and size of edentulous site all statistically significantly affect the accuracy of implant placement.”9
Factors Impacting Accuracy
Given the difference in accuracy of the two systems, it seems likely that inaccuracies with guided implant surgery stem from either the guides themselves or execution of the presurgical plan. Mandelaris and colleagues10 describe a number of factors that may contribute to inaccuracies in guided implant surgery, including the quality of the CBCT and its subsequent reconstruction; the possibility that thin crestal bone is mistaken for other radiopaque structures such as the radiographic template, overlying pontics, or adjacent teeth; the dimensional stability of the stone casts that are later digitized to merge with the presurgical digital plan and later fabricate a guide; the fit and stability of the radiographic template (if used); the movement and fit of the guide at the time of surgery; and the clinician’s expertise in planning. Each of these is sufficient to create significant inaccuracy at the time of surgical execution of the prescribed digital plan.
Mandelaris’s group points out the importance of guide stability. This subtle point should not be overlooked. In evaluating osteotomy depth deviation associated with guided implant surgery, Cassetta and colleagues11 provide additional clarity on the situation. In evaluating 112 implants, in regard to surgical guide support, they looked at paired comparisons of mucosa-supported, tooth-supported, and bone-supported guides. They found bone-supported guides to be more accurate than mucosa-supported guides regarding apical and coronal deviations; tooth-supported guides were also more accurate than mucosa-supported guides. They did not, however, find accuracy differences between the maxilla and mandible, nor between partial and complete edentulism.
Hinckfuss and colleagues9 describe other factors contributing to inaccuracy of implant surgical execution when using a guide. They noted, “If the first implant drill was incorrectly angled or positioned, subsequent drills have a tendency to be guided in the same direction.” They went on to state that “most surgeons assumed they could rely entirely on the guide to control the drill position and angle throughout the drilling sequence, so action to correct early drilling errors did not appear to be taken as often.” Not surprisingly, they reported that implant surgeries involving multiple sites tended to have greater inaccuracies, as the surgeon typically relied upon the guide without question during the procedure. As a result, multiple site surgeries tended to have an increased amount of inaccuracy if the initial drill was off axis or malpositioned. This emphasizes the need for guide stability during surgery. It also highlights the need to visually check the osteotomy’s position during surgery to assure accurate implant placement.
A number of things can be done to improve guide stability and eliminate guide movement during guided surgery. Cassetta and colleagues recommend adequate flap elevation so as not to impinge upon the guide, to eliminate flap tension as a cause for guide instability.8 This requires sufficient and often extensive flap reflection. Additionally, they recommend guide fixation using horizontally placed bone fixation pins. The pins should be arranged at least as a tripod for maximum guide stability during surgery. In these cases, horizontal osteotomies are planned presurgically during the digital planning. At the time of surgery, horizontal osteotomies are prepared through the mucosa into the underlying alveolar bone, through which the fixation pins are placed. It is important to pay close attention in planning and later placing horizontal fixation pins to avoid vital structures such as adjacent tooth roots and neurovascular canals. In dentate and partially dentate patients, the surgeon can place a thin layer of flowable material, such as bite registration material, on the inner surface of the guide, then immediately seat the guide in proper position. Figure 7, Figure 8, and Figure 9 demonstrate this technique, securing the guide in proper position, assuring the guide’s stability, and accurately creating an osteotomy.
Flapless Implant Surgery
One of the advantages of guided implant surgery is reduced complications associated with implant placement in flapless procedures compared with non-guided procedures. Brodala’s systematic review of flapless implant surgical procedures concludes, “Flapless implant surgery appears to be a plausible treatment modality for implant placement, demonstrating both efficiency and clinical effectiveness.”12 He also points out that although the intraoperative complication rate is low, only 3.8%, complications are generally clustered around buccal and lingual alveolar bone perforations. He also points out that the presence or absence of perforations was not reported in most studies and that their impact upon other complications, such as recession and implant failure, is unclear.
An in vitro model study of flapless implant surgery performed by students, general dentists, and specialists questioned the validity of flapless implant procedures.8 In the study, Van de Veld and colleagues found that there were consistent deviations of implant position from ideal position regardless of experience. This occurred despite neighboring teeth remaining in place, seemingly acting as a guide. In fact, they found perforations of the buccal plate in over half of all flapless implant surgeries among specialists at the incisor, premolar, and molar positions.8
Both of these studies led to the conclusion that flapless implant surgical procedures are more accurate when performed with a digitally-created guide. Mandelaris and colleagues agree, reporting on several minimally invasive, flapless, digitally-guided surgeries, including both single tooth and full-arch tooth replacement with endosseous implants. They concluded, “The use of totally guided precision CT-based surgery offers the opportunity for minimally invasive implant surgery and the obvious clinical benefits of reduced pain and swelling associated with open flap techniques.”10 They go on to point out that these procedures require attention to detail in the planning and guide fabrication phases as well as during the procedure itself.
Conclusion
Guided implant surgery is an accurate means of replicating a computer-based presurgical plan. In performing guided surgery, however, the implant surgeon should be familiar with the pitfalls and demands of the technique, recognize how and where inaccuracies may arise, and be adept at overcoming potential errors. Guide stability during surgical execution appears to be the greatest contributing factor to inaccuracies. Other issues—such as dimensional stability of presurgical stone models, poor quality radiographs and reconstructions, and imperfections in milling techniques—may contribute as well. Nonetheless, when assuring guide stability, the digital presurgical plans are accurately replicated at surgery. Guided implant surgery appears to be a significant aide in minimally invasive surgical procedures.
References
1. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19(suppl):43-61.
2. Laney WR, ed in chief. Glossary of Oral and Maxillofacial Implants. Chicago, IL: Quintessence Publishing Co, Ltd; 2007.
3. Rosenfeld AL, Mandelaris GA, Tardieu PB. Prosthetically directed implant placement using computer software to ensure precise placement and predictable prosthetic outcomes. Part 1: diagnostics, imaging, and collaborative accountability. Int J Periodontics Restorative Dent. 2006;26(3):215-221.
4. Higginbottom FL, Wilson TG Jr. Three-dimensional templates for placement of root-form dental implants: a technical note. Int J Oral Maxillofac Implants. 1996;11(6):787-793.
5. Verstreken K, van Cleynenbreugel J, Marchal G, et al. Computer-assisted planning of oral implant surgery: a three-dimensional approach. Int J Oral Maxillofac Implants. 1996;11(6):806-810.
6. Ozan O, Turkyilmaz I, Ersoy AE, et al. Clinical accuracy of 3 different types of computed tomography-derived stereolithographic surgical guides in implant placement. J Oral Maxillofac Surg. 2009;67(2):394-401.
7. Jung RE, Schneider D, Ganeles J, et al. Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants. 2009;24(suppl):92-109.
8. Van de Velde T, Glor F, De Bruyn H. A model study on flapless implant placement by clinicians with a different experience level in implant surgery. Clin Oral Implants Res. 2008;19(1):66-72.
9. Hinckfuss S, Conrad HJ, Lin L, et al. Effect of surgical guide design and surgeon’s experience on the accuracy of implant placement. J Oral Implantol. 2012;38(4):311-323.
10. Mandelaris GA, Rosenfeld AL, King SD, Nevins ML. Computer-guided implant dentistry for precise implant placement: combining specialized stereolithographically generated drilling guides and surgical implant instrumentation. Int J Periodontics Restorative Dent. 2010;30(3):275-281.
11. Cassetta M, Stefanelli LV, Giansanti M, et al. Depth deviation and occurrence of early surgical complications or unexpected events using a single stereolithographic surgi-guide. Int J Oral Maxillofac Surg. 2011;40(12):1377-1387.
12. Brodala N. Flapless surgery and its effect on dental implant outcomes. Int J Oral Maxillofac Implants. 2009;24(suppl):118-125.
About the Authors
Frederic J. Norkin, DMD
Adjunct Assistant Clinical Professor Department of Periodontology
Nova Southeastern University College of Dental Medicine
Fort Lauderdale, Florida
Jeffrey Ganeles, DMD
Assistant Clinical Professor, Periodontics
Nova Southeastern University College of Dental Medicine
Fort Lauderdale, Florida
Private Practice
Boca Raton and Aventura, Florida
Samuel Zfaz, DMD
Adjunct Associate Professor
Nova Southeastern University College of Dental Medicine
Fort Lauderdale, Florida
Private Practice
Boca Raton, Florida
Alireza Modares, DDS
Private Practice
Boca Raton, Florida