2013 Rewind
A look back at the products, techniques, and innovations that defined 2013
2013’s Mission Critical Technology
CAD/CAM technology had a very good year
Dr. Koenigsberg is a partner at Gallery57 Dental in Manhattan, New York, and a co-founder of CAD/CAM Excellence.
This past year saw a continuation of the trend of technology transforming the practice of dentistry. Advances in CAD/CAM, imaging, implant planning software, and lasers are changing the procedures we do and the way we deliver these services. There have been significant improvements in the “workflow” of the individual products as well as greater integration between products. Many of these technologies are or will soon be “mission critical,” meaning that you won’t be able to practice without them.
< CAD/CAM equipment. After many years where dental CAD/CAM was a “niche” technology, 2013 witnessed an explosion of new product entries on to the market and the “mainstreaming” of intraoral scanning. Intraoral scanners are now offered by at least six major companies, with more on the way. Some of the new scanners do not require powder, which reduces the learning curve and makes full-arch impressions a reality. These digital models are ideal for the fabrication of clear orthodontic retainers and more complex cases. Most companies now offer the option of purchasing only the intraoral scanner, allowing dentists to start integrating CAD/CAM into their practice at a lower cost and with minimal disruption to their existing workflow. 2013 also saw the introduction of a “plug and play” 3D scanner that will allow an office’s own computers and monitors to be used, saving money and space, as well as allowing easy sharing of the camera between operatories. There is a trend to standardize and open up the technology so that a dentist may be able to use the camera from one manufacturer, the design software of another, and the milling unit of yet a third company. This will allow offices to decide on the solution that works for them and should lower costs.
< CAD/CAM software. With some software systems, perfect crowns can routinely be designed in minutes by anyone with knowledge of dental anatomy and function. Sirona has introduced a “virtual articulator” so that excursive function can be accounted for in the design. There have also been new applications developed to scan implants directly and design and mill implant abutments, in-office. The ability to fabricate precision surgical guides for $30 in 15 minutes has made them accessible to general practitioners on a routine basis, potentially opening up a huge area of practice growth.
< CAD/CAM materials. Nano-ceramics (eg, VITA’s Enamic®) have been introduced that are monolithic, strong, and can be milled to bevels and finished in minutes. These materials have been developed specifically for use by in-office CAD/CAM systems. Several manufacturers have added lithium ceramics to compete with the hugely successful IPS e.max® CAD (Ivoclar Vivadent) blocks, which are now available for milling bridges in the office. Zirconia has evolved so that it, too, is an option for the in-office, single-visit crown. Undoubtedly, with the growth of CAD/CAM we can expect additional materials designed specifically for this technology.
< Imaging. 2D imaging has continued to evolve, with software enhancements such as caries detection and custom settings, along with better and more durable sensors. Dexis introduced a free iPad app for enhanced patient communication. For the value shopper, low-priced sensors have been introduced that reduce an important barrier to going digital. 3D cone-beam computerized tomography (CBCT) units are now available with different fields of view, allowing dentists to select a machine that fits their needs with significant savings. New features allow for resolution and volume adjustment, which can reduce radiation exposure. Sirona has introduced an integrated facial scanner, allowing the patients’ soft tissue to overlay the bone scan.
Integration between CAD/CAM intraoral scans and CBCT scans is now a reality, allowing doctors to “virtually” place the final restoration as the first step in implant planning. It is no longer necessary to send model to a lab and have teeth built up in a radio-opaque material. The implant can be virtually placed in the best possible position relative to the bone and restoration and a precision guide can be milled in minutes. This results in a more predictable and less traumatic procedure for the patient and a faster, less stressful visit for the dentist.
< Lasers. Manufacturers have added features on their hard/soft tissue lasers to speed up workflow and ease the learning curve. Soft tissue protocols have been introduced. Convergent Dental has introduced a new CO2 laser called Solea™, which is claimed to cut enamel and dentin quickly and smoothly. There is a variable speed, computer-controlled foot pedal, which mimics the feel of traditional drill rheostats.
Although there were no new “breakout” technologies in 2013, there were significant improvements to technologies that have been around for 10 to 25 years. These improvements involved better workflow, more integration, new features, more manufacturers and more applications, which together make these technologies increasingly important in practicing good dentistry.
Is Today the Golden Age of Implant Dentistry?
Advances in technology and design have brought unprecedented growth
Dr. Sonick is in private practice in Fairfield, Connecticut.
Is this the golden age of implant dentistry? Joel Klein, editor-in-chief of Time magazine, states that we never know when we are living in the golden age. This may be true. Today, I spend most of my clinical days performing procedures that improve the quality of patients’ lives that did not exist the day I graduated from dental school in 1979.
Soft tissue grafting for root coverage and implant augmentation, including the subepithelial connective tissue graft, which was developed by Langer and Langer, was not introduced until 1985. Today, soft tissue augmentation is performed routinely. Periodontally involved teeth, previously deemed hopeless, can now be saved and maintained, and their lost bone regenerated. Guided bone regeneration around teeth was not introduced into the literature until 1981 by Nyman, and has taken decades to perfect. Osseointegrated titanium implants were not introduced into North America until the landmark 1982 conference in Toronto. Research was begun decades earlier by P.I. Brånemark in Gothenburg, Sweden, but was not well known in North America. The research was published mostly in Swedish, when the Internet was but a thought and international cooperation was sparse. Today, dental implants are the standard of care, almost taken for granted—like the World Wide Web.
At the onset of dental implant placement, osseointegration was the goal. There was great excitement when implants merely integrated. Today implants must not only integrate but be ideally positioned in adequate bone so that optimal esthetics and function are achieved. Things have moved very fast these past 30 years, and the pace of change will only quicken as more dentists preform research, clinically document their cases, and collaborate more with each other.
Dan Sullivan, prosthodontist and past president of the Academy of Osseointegration, once commented at a national meeting that misplaced implants were often accompanied by a letter by the surgical specialist lamenting, “Sorry, but that is where the bone was.” Today this refrain is heard less often. Perhaps the greatest accomplishment since the onset of osseointegration has been the ability to regenerate bone in areas of deficiency. Two absolute requirements for the surgical placement of dental implants exist:
Implant stability at the time of placement
Ideal restorative position
Currently, bone can be predictably regenerated at the time of extraction. Most times, adequate bone for implant placement can also be regenerated post-extraction. Although limits in volume do exist, this is changing. The introduction of newer technologies in guided bone regeneration has made possible implant site development in areas previously thought hopeless. A variety of barrier membranes, growth factors (PRP, PRF, PRGF, rh-PRGF, Emdogain, rh-BMP, etc), and newer technology have revolutionized dental implant treatment. Unprecedented amounts of bone regeneration are now possible.
The use of newer technologies, including cone-beam computed tomography, has led to greater accuracy in diagnosis and treatment planning. The implant surgeon no longer must go on a surgical tour, developing the treatment plan during surgery. Patients are now able to see what is possible and what is not possible prior to surgical treatment. This allows for patient participation in treatment decisions and shared responsibility.
Lastly, differences in the design of dental implants (tapered implants, aggressive thread pitch, roughened surfaces, treated surfaces, etc) have led to a greater speed in osseointegration. Some companies tout “immediate osseointegration” with immediate loading. All cases must be evaluated individually. Patent immediate gratification is not always possible, and should be couched with what is predictable.
Time-Saving Materials
New options for streamlining restorative procedures
Dr. Helvey is an adjunct associate professor at Virginia Commonwealth University School of Dentistry in Richmond, Virginia, and a restorative dentist in private practice in Middleburg, Virginia.
This past year brought many new restorative materials and systemswith time-saving benefits for delivery of services and greater patient satisfaction and comfort. Here are six categories of products that will be of special interest for restorative dentists.
< Impression materials. 3M ESPE introduced Imprint™ 4 VPS Impression Material, which provides the same working time for the clinician and yet a shorter setting time for the patient. Another impression time-saver is the elimination of retraction cord placement with Aquasil Ultra Cordless Tissue Managing Impression System from DENTSPLY Caulk. According to the manufacturer, this system saves time with the elimination of placing cord or using paste, in most cases, while recording fine marginal detail.
< Digital scans. Even with new and improved traditional impression systems, the use of digital impression scanning is growing. Presently, there are five major systems available (Align Technology’s iTero, 3M ESPE’s True Definition Scanner, Sirona’s CEREC®, IOS Technologies’ IOS FastScan™ and E4D Technologies’ NEVO™) that can digitally scan preparations; CEREC and E4D still are the only systems that can fabricate restorations chairside.
< Universal adhesives. New “universal” bonding adhesives are becoming more widely used. These systems are easy to use while providing high bond strength and reduced sensitivity. The added benefit to these universal systems is that they can be used for direct and indirect restorations.
< Bulk-fill composites. There are more “bulk-fill” composite systems now available that save a considerable amount of time over the traditional incremental build-up technique. Although the incremental build-up technique has years of research to recommend its use, the bulk-fill products look promising. Further studies are needed to look at the depth of cure with fast-curing lights and creating tight interproximal contacts. Volumetric shrinkage and stress are still at the same level as conventional composites.
< Finishing and polishing. Polishing systems have been streamlined to simplify the last step of placing direct restorations. A new design in 3M ESPE’s Sof-Lex™ Spiral Finishing and Polishing Wheels allows the flexible shape to adapt to irregular concave and convex tooth surfaces. This shape replaces having to change to points, cups, wheels, and brushes, which saves time. These are single-use devices that are used without paste or water-cooling.
< Sensitivity. Kuraray has introduced a new approach to treating root sensitivity. Teethmate™ Desensitizer occludes the tubules with hydroxyapatite (HAp) by mixing tetra calcium phosphate and dicalcium phosphate with water and a catalyst. There is no film thickness and it does not interfere with subsequent resin bonding. Teethmate can be applied by the clinician or the dental hygienist without isolation. In addition, there is no irritation to the soft tissue.
State-of-the-Art Endodontics
Improvements that enhance clinical outcomes
Dr. Richard Mounce is a full-time endodontist in private practice in Rapid City, South Dakota. He owns MounceEndo, LLC, an endodontic supply company marketing Controlled Memory nickel-titanium instruments and Mani, Meta BioMed, and Aseptico Products.
In much of the world, canals prepared by stainless hand files, “cleaned” by passive irrigation, and obturated by cold lateral condensation have given way to improved evidence-based treatment methods. Ultimately, these advances are improving our patients’ quality of life through natural tooth retention and making treatment more predictable for each of us—a winning combination.
< Instrumentation. Second-generation heat-treated instruments (eg, DENTSPLY Tulsa’s M-Wire™ products, Axis/Sybron’s TF®, MounceEndo’s MounceFile Controlled Memory [CM]) whose safety, efficiency, and mechanical properties are dramatically superior to their first-generation predecessors are now available. Second-generation files have far greater cyclic fatigue resistance and improved flexibility relative to the first generation. In addition, CM instruments offer an additional advantage in that they hold their shape once curved. Clinically, this means CM files remain curved as they cut dentin rotating in canals, reducing transportation relative to standard shape memory files.
In addition, once used solely with stainless steel hand files, reciprocation of nickel-titanium files has joined rotary endodontics as a shaping option. At present, Axis/Sybron’s TF® Adaptive and DENTSPLY’s WaveOne® predominate this market. New and improved reciprocating files and motors are on the horizon. Lastly, safe and efficient gutta-percha removal in endodontic retreatment has also seen an advance with the new and unique Mani GPR instrument series.
< Anesthesia. Patient comfort is improving through innovative local anesthesia delivery. Both the STA™ device from Aseptico and the Anesto from W&H are significant improvements over the hand-held syringe.
< Looking ahead. Technology that will remove all tissue, biofilm and smear layer, and disinfect into the dentinal tubules is coming in the form of Sonendo®. According to its website, “Sonendo has developed a system that delivers broad spectrum sonic energy through a disposable dental ‘handpiece’ to the root canal system. This closed loop, fluid-based system is designed to quickly, easily and safely loosen and remove all the tissue, debris, and bacteria from the canal within minutes.” Having observed this disruptive technology first hand, a quantum leap forward for patients’ comfort, clinical efficacy, and endodontic predictability is near. Although not yet available, Sonendo is part of a very bright future for endodontics and, more importantly, our patients.
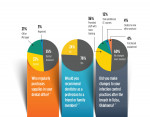
What Keeps You Up at Night?
Ray Williams
Adjunct Professor, Periodontology
UNC School of Dentistry
Chapel Hill, North Carolina
On a weekly basis, I hear the words “outreach” and “global dentistry.” I also read about outreach efforts that are bringing dental care to those in need around the globe. This is a good thing happening in our profession. Helping others who do not have access to dental care in remote places is certainly not new in dentistry, but the momentum seems to have picked up and the outreach seems more organized. I think we are clearly on our way with bringing dental care to the world, and there is no turning back.
As an administrator/teacher in a dental school, I have watched the growth of our school’s “outreach” program and have seen it become a very popular part of the 4-year pre-doctoral experience. As such, we are better able to bring much needed dental care to diverse populations nationally and internationally. I watch the dedication of our faculty and students who work tirelessly to fund our outreach missions through numerous fundraising initiatives. Having found the resources for another outreach mission, they travel far and wide to help people. And then, I watch as our teachers and students return from an outreach mission, their lives having been forever transformed by the opportunity to help those in great need. I wonder, and rightly so, how on Earth we will find the time and the resources to conduct the next outreach mission. But I know the answer and it is simple. We will.
Gerard Kugel, DMD, MS, PhD
Associate Dean for Research
Tufts University School of Dental Medicine
Private Practice
Boston, Massachusetts
What keeps me up at night would be the number of new materials and techniques that are being introduced to dentistry with little or no bench and/or clinical data. We just completed a study attempting to identify fundamental differences in publications existing between successful and unsuccessful dental materials. As expected, there was a very significant difference in the number and quality of the research between the failed and successful products.
It seem that our dental offices have become the clinical test sites for these new products. I lose sleep over this.
Amanda Seay, DDS
Private Practice
Mount Pleasant, South Carolina
The knowledge that our profession continues to evolve in ways that give us the opportunity to be better at what we do. I am excited about the growing realization that digital technology, specifically CAD/CAM dentistry, is changing the way we do dentistry in the operatory and the dental laboratory. Communication among the restorative dentist, surgeon, and laboratory technician can be done more efficiently with the software that is available today. The technicians get to add another tool to their artistic set of skills—to be able to digitally design and review their creation and have milled wax and pressed restorations from one source is incredible. This means that CAD/CAM, which has traditionally been for posterior restorations, is playing an increasingly larger role in esthetic dentistry when it comes to anterior restorations.
2013's Hottest Products
1. Endo-Express & SafeSiders (Essential Dental Systems)
2. Composi-Tight 3D XR Sectional Matrix System (Garrison Dental Solutions)
3. Blu-Mousse and Green-Mousse (Parkell, Inc.)
4. Peter Brasseler Series Diamonds (Brasseler USA)
5. Keller Bite Appliances (Keller Laboratories)
6. Schick 33 (Sirona)
7. ERA Attachments (Sterngold Dental)
8. All-Bond Universal (BISCO)
9. True Definition Scanner (3M ESPE)
10. CEREC AC with Omnicam (Sirona)
Source: InsideDentalProducts.com