The Next Evolution in CBCT: Combining Digital Technologies
A precise approach to planning dental implant reconstruction enhances accuracy.
Dental implants have provided clinicians with an increasing variety of solutions for patients who have lost or will lose their teeth, improving both function and esthetics while significantly impacting their quality of life. Treatment plans originally derived from two-dimensional (2-D) periapical or panoramic radiographs offered a limited appreciation of the bone and adjacent vital structures. The use of three-dimensional (3-D) imaging technologies has greatly enhanced the diagnostic modalities available for clinicians to treatment plan dental implants and associated grafting procedures. The recent move from medical computed tomography (CT) to cone beam computed tomography (CBCT) has provided lower radiation alternatives and removed many other barriers related to the use of the imaging modality, including immediate access through small-footprint, in-office machines.1
Managing the workflow has become an important part of the process, as many of the CBCT scanning machines have different protocols for diagnostics and the ultimate production of surgical templates. The native digital imaging and communication in medicine (DICOM) data needs to be converted for visualization and manipulation on a computer monitor. The ideal scenario would allow clinicians to accurately assess patient anatomy through the use of CBCT imaging while having an understanding of the desired final restorative result. This is best accomplished through the use of interactive treatment-planning software that helps to re-process the DICOM digital data for clinical interpretation and manipulation.2
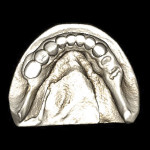
While CBCT provides insight into the 3-D assessment of the mandible or maxilla for implant placement, it does not do the best job of replicating the surface detail of teeth or surrounding anatomical structures. Surface data acquisition can be accomplished by using one of three methods: (1.) placing a stone cast into an optical scanner to capture the surface detail and occlusal morphology; (2.) placing a stone cast into the same CBCT scan machine with the same settings as the patient’s scan; or (3.) using intraoral scanners to take a virtual impression of the patient’s dentition. The majority of clinical applications use a stone cast fabricated from an intraoral impression with standard trays and impression materials (Figure 1). The diagnostic process has been further enhanced by the development of software applications that allow data from different sources to be combined. Merging the digital information from either method (optical or DICOM) with the original CBCT data greatly enhances the diagnostic phase and improves restoratively driven treatment planning (Figure 2).
Figure 3 illustrates a CBCT-derived volumetric rendering of a mandibular arch with missing teeth in the right posterior quadrant (Imaging Sciences, Inc., www.imagingscience.com). The stone cast data, as seen in Figure 1 and Figure 2, were merged with the DICOM data within the interactive treatment planning software (Invivo5 Anatomage, Anatomage, www.anatomage.com) to aid in the planning of the mandibular distal extension case. The “virtual teeth” were digitally fabricated to help plan three implants supporting three proposed crowns in the desired occlusal relationship, while avoiding the inferior alveolar nerve. The red “projections” seen in Figure 3 help provide the clinician with the trajectory of the implant and how the abutment would connect to the intended position of the desired restorations or within the envelope of the tooth. This type of planning aids clinicians in determining the prosthetic requirements prior to the surgical intervention. Armed with an individualized 3-D assessment of patient anatomy, educated decisions can be made with regard to crown-to-implant ratio, implant diameter and length, and the design of the restoration in terms of screw or cement retention.3 The clear, illustrative images are excellent for communicating with all members of the implant team, greatly improving the communication process for patient education and thus resulting in increased case acceptance.4
The third method for intraoral data acquisition is gaining popularity as the use of intraoral scanners precludes the need for conventional impression materials, while allowing for accurate surface reproduction using novel optical scanners chairside.5 Intraoral scanners streamline the digital workflow—just as digital cameras obviated the need for film—and the images go directly to the computer for interpretation. Intraoral scanners can be used in a variety of methods to enhance planning for dental implant placement and restoration. Intraoral scanners include but are not limited to: iTero™ (Align Technology, www.aligntech.com); E4D Dentist (D4D Technologies, www.e4d.com); TRIOS® (3Shape, www.3Shape.com); Lava™ C.O.S. (3M ESPE, www.3mespe.com); and CEREC® (Sirona Dental Systems, www.sirona.com).
It is now possible to merge the new digital data set from an intraoral scanner to the original CBCT scan data within the software used. The two separate files must go through a registration process to confirm accuracy. Once combined, the surface detail of the surrounding tooth anatomy is then incorporated into the interactive treatment planning software, and assessment of potential implant receptor sites can be evaluated with increased accuracy. Manipulating the software allows for a variety of different views to help aid in the planning process. For example, “removing” the bone and stone cast from view reveals the underlying precision placement of the simulated implants, abutments, and translucent virtual teeth in proximity to the natural tooth roots (Figure 4) (SimPlant®, Materialise Dental, Inc., www.materialisedental.com). Note that each implant and abutment realistically represents the actual manufacturer’s design, as chosen from the software library of components (ANKYLOS®, DENTSPLY Friadent, www.dentsply-friadent.com).
The patient’s original clinical presentation can be used for planning, or if desired, a diagnostic wax-up of the desired final restoration. Surgical templates can then be accurately fabricated from the 3-D virtual simulation to provide the link from the simulated plan to the surgical intervention. Templates derived from the CBCT scan data and interactive treatment planning software serve to increase surgical accuracy, diminish chairtime, decrease patient morbidity, allow for minimally invasive surgery in selected cases, and increase clinician confidence due to the improved understanding of the patient anatomy, while removing the guesswork from the process. However, it must be emphasized that the template will be only as good as the plan; therefore, the diagnosis and treatment-planning phase is critical to success.
The ability to plan dental implant reconstruction with greater precision is possible today due to the complete assessment of each potential implant receptor site, the length and width of each implant, the type of abutment to be used, and the components required to complete the case from surgical intervention through prosthetic rehabilitation. Having this knowledge before the scalpel ever touches the patient prepares all members of the dental implant team for successful outcomes without surprises. The ability to combine different technologies—including CBCT, optical scanning, interactive treatment planning software, and intraoral impressioning—enhances the process of providing accurate solutions for patient care, further defining the expanding arena known today as “digital dentistry.”6
References
1. Benavides E, Rios HF, Ganz SD, et al. Use of cone beam computed tomography in implant dentistry: the International Congress of Oral Implantologists consensus report. Implant Dent. 2012;21(2):78-86.
2. Ganz SD. Advanced Case Planning with SimPlant. In: The Art of Computer-Guided Implantology. Tardieu P, Rosenfeld Al, eds. Hanover Park: IL: Quintessence Publishing Co, Inc.; 2009.
3. Ganz SD. Defining new paradigms for assessment of implant receptor sites. The use of CT/CBCT and interactive virtual treatment planning for congenitally missing lateral incisors. Compend Contin Educ Dent. 2008;29(5):256-267.
4. Tischler M, Ganz SD. The CT/CBCT-based team approach to care. Part I: Identifying the implant patient and prosthetic options. Dent Today. 2012;31(8):
74-79.
5. Lee CY, Ganz SD, Wong N, Suzuki JB. Use of cone beam computed tomography and a laser intraoral scanner in virtual dental implant surgery: part 1. Implant Dent. 2012;21(4):265-271.
6. Ganz SD. Establishing New Prosthodontic Fundamentals for Implant Reconstruction through Technological Advances: Myths vs Realities. Presented at the ICOI Winter Symposium. Bellagio Hotel, Las Vegas, NV February 10, 2011.
About the Author
Scott D. Ganz, DMD
Private Practice in Prosthodontics
Maxillofacial Prosthetics and Implant Dentistry
Fort Lee, New Jersey