Restoring Endodontically Treated Teeth
Clinicians have a host of factors to weigh when determining the best method for restoring an endodontically treated tooth.
By Christine M. Yonker, DDS; Sergio Rubinstein, DDS; Alan J. Nidetz, DDS
Consider the following scenario: A patient sits in the treatment room, ready to have a filling replaced due to marginal breakdown and secondary decay. The practitioner clearly warns the patient that trauma to the tooth can cause the nerve to become irritated and symptomatic, which results in the need for endodontic therapy.
Furthermore, determining the extent of the decay is difficult until caries excavation begins. Therefore, it is too soon to predict whether endodontic therapy will be necessary. What the doctor has failed to mention is that the cost and time investment of the final restorative procedure will drastically differ from a filling replacement if a root canal is indeed indicated. The patient requests that the dentist stop drilling before the nerve is approached, so as to avoid a root canal. The patient is assured that the dentist will go slowly, in order to prevent performing a root canal if possible. Predicting the extent of the decay, however, is impossible without further caries removal.
Sure enough, the decay is extensive, and a pulpal exposure occurs during caries removal. The patient is notified that the nerve has been exposed, and root canal therapy is ultimately indicated. At this point, the patient is made aware that a post, core, and crown will be required after the root canal. The patient asks why several procedures are now needed when a filling was sufficient before, and wonders if a filling could just be placed after the root canal is completed.
It may be a common misconception in dentistry that a root canal goes hand-in-hand with a post and crown, but the questions concerning whether these additional procedures are really necessary are valid ones. It may be possible to restore the tooth with a direct restorative procedure, but will this elicit the best long-term outcome? How much tooth structure will remain once caries removal is completed? Can the endodontic access be closed with a direct composite? Is there enough tooth structure remaining to establish ferrule? When and why is a post-and-core build-up required?
As historically described in the literature, full-coverage crowns should only be used when there is insufficient coronal tooth structure for a more conservative restoration, or if functional or parafunctional stresses require the splinting effect of full coronal coverage.1 This may indicate that full coverage should possibly be avoided unless the above criteria are present.
Still, more questions remain: Does a more “conservative restoration” have the best long-term predictability? Is it still considered a conservative procedure if failure of the endodontically treated tooth is the ultimate outcome? One study explored whether coronal coverage impacted the survival rate of endodontically treated teeth. Tooth loss was six times higher in endodontically treated teeth without coronal coverage.2 Another clinical trial demonstrated an average time of 87 months before extracting an endodontically treated tooth, compared to 50 months without full coverage.3 In light of this information, the clinician must again consider which procedure is more conservative.
Before determining the least aggressive, most predictable restoration, it is important to first understand how the tooth structurally changes upon completion of endodontic therapy. Over time, views on changes in mechanical properties of endodontically treated teeth have varied. In 1983, Carter noted that endodontically treated teeth exhibit a fragility that vital teeth do not. He made reference to the low-moisture content of root canal teeth, and demonstrated that vital teeth had higher punch shear strength and toughness values.4 This idea was countered nearly a decade later, through a study that tested biomechanical properties such as punch shear strength, toughness, load to fracture, and microhardness of dentin in endodontically treated teeth as compared to vital teeth. The study concluded that teeth do not become more brittle after endodontic treatment.5 More importantly, the study determined that it is not the change in biomechanical properties of dentin in endodontically treated teeth that contribute to challenges in restorability of the tooth. Rather, the amount of remaining tooth structure, specifically dentin, illustrates a direct relationship with resistance to occlusal forces.6
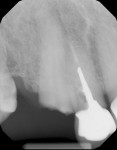
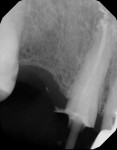
Given this knowledge, the clear goal in restoring an endodontically treated tooth is to preserve as much dentin as possible. If the restorative dentist is not completing the endodontic therapy, then communication between the restorative dentist and endodontist is vital to ensure the maximum amount of dentin remains (Figure 1 and Figure 2). In order to evaluate restorability of the tooth, the restorative dentist must be sure to remove all decay before recommending endodontic therapy. The endodontist can better evaluate the predictability of the endodontic therapy if the restorative plan can be communicated before beginning root canal therapy. The endodontist can also modify treatment, if necessary, to leave a post space that removes the least amount of dentin and best follows the anatomy of the canal, with which they are already familiar.7 Achieving endodontic success requires properly cleaning and sealing the canal as well as setting the proper restorative path for the tooth, taking into consideration the rest of the dentition in the patient’s mouth in order to obtain the best long-term outcome. Occlusion, position in the arch, and periodontal health must also be considered.8 When discussing the long-term success of an endodontically treated tooth, it might seem logical to think that the majority of root canals that fail are due to endodontic origin. However, one clinical study that classified failures of endodontically treated teeth found restorative origin to be the primary reason for failure. Conversely, the least amount of failures resulted from endodontic causes.3
This surprising finding reveals the important role the restorative dentist plays in the long-term success of root canal therapy. The restorative dentist must consider whether the treated tooth is only one in a mostly stable and healthy dentition with all remaining teeth providing proper masticatory function, or if several teeth are missing. There are other variables to account for as well, including periodontal disease, malpositioning of the tooth, mobility, malocclusion, and parafunctional habits. If the tooth is subjected to carry supplemental occlusal forces, it may be at greater risk for failure of the restoration as well as possible vertical root fracture in an otherwise properly endodontically treated tooth (Figure 3).
If the goal of the endodontist is to sterilize and seal the canal, then the restorative dentist’s goal is to maintain that coronal seal with a stable restoration. Several factors must be weighed when choosing a composite restoration as the material of choice in restoring an endodontically treated tooth. As previously noted, preservation of dentin is very important in the restoration of an endodontically treated tooth. So, the preservation of tooth structure is an obvious benefit of restoring with a direct restoration.
Adhesive dentistry was initially discussed by Buonocore in 1955, when he found that acid-treating enamel increased adhesion of acrylic-based filling materials.9 Acid-etching causes microporosities in enamel, in which resin can flow to achieve micromechanical retention. When restoring an endodontically treated tooth with significant removal of tooth structure, enamel may not be readily available to achieve a predictable bond, which is why dentinal bonding becomes increasingly important. Bonding to dentin can be more challenging, due to the natural moisture content of dentin and the hydrophobic qualities that most dentin-bonding agents possess. Nakabayashi et al first described the infiltration of monomers having both hydrophobic and hydrophilic groups as a successful adhesive technique.10
Although new methods of dentinal bonding are continually being researched, there are still limitations to the technique. These limitations include polymerization shrinkage that can lead to fractures in the tooth or result in gap formations at the weakest points of the dentin bond, and loss of bond strength that leads to eventual leakage.11 Additional drawbacks to bonding in a root canal system, such as C-factor and irrigants used during the endodontic procedure, should be considered. C-factor is defined as the ratio of bonded surfaces in a cavity to unbounded surfaces. As the number of bonded surfaces increase, so does the risk of debonding from the dentin as a result of the stresses from polymerization shrinkage. Essentially, every dentinal wall in a root canal system has an opposing wall, which results in an extremely unfavorable C-factor.12
The irrigant used during the root canal treatment can also have potential negative effects on the bond. Sodium hypochlorite, a common irrigant, is also an oxidizing agent, and thus can leave behind an oxygen-rich layer that can inhibit polymerization of resins. This leads to decreased bond strength and an increased risk of microleakage. It has been shown that application of materials such as Accel (Sun Medical Co, www.sunmedical.co.jp) and rosmarinic acid could neutralize the oxidizing effect, therefore increasing the bond strengths to dentin treated with sodium hypochlorite.13 Perhaps most importantly, increased cuspal deflection in molars has been shown to occur as a result of increased removal of tooth structure, particularly after endodontic access. This reinforces the importance of full cuspal coverage in an endodontically treated tooth.14
While full cuspal coverage has been shown to significantly increase the success rate of a posterior endodontically treated tooth, there is no considerable improvement in the success of an anterior endodontically treated tooth. Furthermore, intracoronal reinforcement does not necessarily provide an increased resistance to fracture or dislodgement.15 Forberger and Gohring demonstrated the opposite, by evaluating marginal continuity and fracture resistance of all-ceramic crowns with differing substructures.16 It was shown that endodontically treated premolars restored with post-and-core foundations had significantly greater resistance to stress and loading forces, as compared to crowns without the placement of access cavity restorations. Additionally, teeth restored with a rigid post-and-core substructure demonstrated less marginal leakage than teeth with a non-rigid post and core.16 The benefits of full cuspal coverage in an endodontically treated tooth have become more apparent. The argument for a post and core, however, becomes much more involved due to the conflicting data on their risks and benefits, especially with the wide variety of features different post systems offer.
Added retention to a tooth with minimal remaining tooth structure is the primary reason for placement of a post. The benefit of added retention, however, must be weighed against the potential risks of post-space preparation. These risks include the possibility of disturbing the root canal seal, the excessive removal of dentin—thereby weakening the tooth—and risk of root perforation. Rigid post and cores such as cast gold, zirconia, or ceramic have been shown to be the least desirable post design for stress transmission.17 Rigid posts are very stiff, which gives them added strength under loads, but can also lead to increased root fracture, due to transmission of forces to less rigid dentin. Ceramic and zirconia do not possess the darkness that metal does, and may provide a more esthetic option for a rigid post. But, using a noble metal to cast a post and core means that less tooth structure needs to be removed. Compared to a stiffer material, fewer forces are ultimately transmitted to the tooth.
Obtaining a passive fit as well as venting the restoration before cementation is very important in avoiding unnecessary pressure in the root canal system. In order to obtain a path of insertion, a cast post also requires increased removal of tooth structure. More tooth structure can be preserved, however, in a pre-fabricated post. Non-rigid posts, such as pre-fabricated fiber posts, have become the treatment of choice in most circumstances when posts are indicated. Although non-rigid posts reduce the transmission of forces to the tooth—which can lead to increased marginal leakage over time—the benefits of these reduced forces outweigh the possibility of marginal leakage. The decreased load transferred to the root dentin leads to less irreparable root fractures upon failure (Figure 4).11 This is significant because marginal leakage has the potential for repair, whereas a root fracture almost always does not.
Regardless of post placement, it has been shown that the design of the ferrule is essential in improving load resistance in root-canal treated teeth, despite varying degrees of post length.18 Guidelines for a proper crown preparation include well-defined margins with appropriate axial and occlusal reduction, and proper margin selection based on the type of crown being fabricated, axial wall height of at least 3 mm, and nearly parallel opposing walls, minimally tapered (Figure 5).
If a tooth is badly broken down, these criteria become more difficult to achieve, and other criteria such as ferrule design become increasingly important. In dentistry, ferrule is defined as a metal band or ring that encircles the tooth in order to provide retention and resistance form, as well as protect the tooth from fracture. Generally, at least 2 mm of ferrule is desired, but one study showed that at least 1 mm of coronal tooth structure improved fracture resistance. Still, 2 mm is strongly recommended. The same study showed that parallel walls proved to be the most critical factor in resistance to dislodgement, more so than margin design and axial width of the tooth at the crown margin.19 If ferrule cannot be obtained, other procedures such as clinical crown lengthening, orthodontic extrusion, or possible extraction may become necessary.
What are the benefits of pursuing such treatment, given the increasing number of dental implants being placed, and such ambiguity regarding the best, most predictable method of restoring an endodontically treated tooth? Successful endodontic and restorative treatment provides patients with the opportunity to preserve their natural dentition with excellent function for several years. Furthermore, the preservation of the tooth and periodontal ligament will enable the patient to maintain proprioception, which would otherwise be lost.
There may be some controversy surrounding the best method of restoring an endodontically treated tooth. But, once it is determined that a post, core, and crown are the appropriate treatment, placing the best possible restoration gives the patient a significantly better chance of increasing the life of the endodontically treated tooth. Determining which restoration is most conservative is left up to individual practitioners, and should be determined on a case-by-case basis. What is most important is having the appropriate knowledge to be able to make that decision confidently.
Case Report 1
The patient presented with an existing occlusal amalgam on tooth No. 18. The patient reported temperature sensitivity and percussion sensitivity, and was referred to a specialist where the root canal was completed. The patient returned for final restoration at the completion of root canal therapy where a pre-fabricated post was fit and bonded in place (Figure 6). After the post, a composite build-up was used to replace the missing tooth structure that was removed during the endodontic therapy (Figure 7). The need for a full-coverage crown was discussed with the patient prior to having the root canal completed (Figure 8). Communicating with the endodontist to outline the final restorative plan for the tooth was extremely important. In this case, the endodontist was able to prepare an appropriate post space before the patient returned to the restorative dentist. This not only saved the restorative dentist time during the restorative procedure, but it also ensured that excess dentin removal did not occur (Figure 9 and Figure 10). Conversely, if the endodontist creates a post space unnecessarily, undue forces may be placed on the root.
Case Report 2
This patient presented with a fractured tooth No. 9. Endodontic therapy was completed and the tooth was prepared for a full-porcelain crown (Figure 11 and Figure 12). For several reasons, the decision to fabricate a casting was made. While there are different ways of fabricating a cast post and core, inlay resin was used for this patient (Figure 13). The casting was fabricated using high noble alloy (Figure 14). One of the reasons that the decision to use a casting was made was due to the size of the build-up in relation to the size of the post. If a prefabricated post and core was used, the retention of the build-up would rely solely on the bonding because of the ratio of the build-up to the post. This concept is similar to looking at the crown-to-root ratio when considering different restorative plans. Furthermore, attention also had to be paid to the deep bite that this patient possessed (Figure 15). If excessive loads were placed on this anterior tooth, these loads would be transferred to the underlying post and core. In this case, because of the size of the tooth, location of the tooth and forces placed on this tooth, it made more sense to fabricate a cast post and core.
References
1. Walton RE, Torabinejad M. Principles and Practice of Endodontics. 3rd ed. 2002;269-281.
2. Aquilino SA, Caplan DJ. Relationship between crown placement and the survival of endodontically treated teeth. J Prosthet Dent. 2002;87(3):256-263.
3. Vire DE. Failure of endodontically treated teeth: Classification and evaluation. J Endod. 1991;17(7):338-342.
4. Carter JM, Sorenson SE, Johnson RR, et al. Punch shear testing of extracted vital and endodontically treated teeth. J Biomech. 1983;16:841–848.
5. Sedgley CM, Messer HH. Are endodontically treated teeth more brittle? J Endod. 1992; 18(7):332-335.
6. Assif D, Gorfil C. Biomechanical considerations in restoring endodontically treated teeth. J Prosthet Dent. 1994;71(6):565-567.
7. Lorton L, Vire DE. Special restorative considerations for endodontically treated teeth. J Endod. 1981;7(3):133-136.
8. Kogan E, Rubinstein S, Zyman G, Nidetz AJ. Evolution and integration of current restorative concepts. Alpha Omegan. 2007;100(3):120-126.
9. Buonocore MG. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res. 1955;34(6):849-853.
10. Nakabayashi N, Kojima K, Masuhara E. The promotion of adhesion by the infiltration of monomers into tooth substrates. J Biomed Mater Res. 1982;16(3):265-273.
11. Ree M, Schwartz RS. The endo-restorative interface: current concepts. Dent Clin N Am. 2010;54:345-374.
12. Tay FR, Loushine RJ, Lambrechts P, et al. Geometric factors affecting dentin bonding in root canals: a theoretical modeling approach. J Endod. 2005; 31(8):584-589.
13. Prasansuttiporn T, Nakajima M, Kunawarote S, et al. Effect of reducing agents on bond strength to NaOCl-treated dentin. Dent Mater. 2010;Nov 10.
14. Panitvisai P, Messer HH. Cuspal deflection in molars in relation to endodontic and restorative procedures. J Endod. 1995;21(2):57-61.
15. Sorensen JA, Martinoff JT. Intracoronal reinforcement and coronal coverage: A study of endodontically treated teeth. J Prosthet Dent. 1984;51(6):780-784.
16. Forberger N, Gohring TN. Influence of the type of post and core on in vitro marginal continuity, fracture resistance, and fracture mode of lithia disilicate-based all-ceramic crowns. J Prosthet Dent. 2008;100(4):264-273.
17. Baraban DJ. The restoration of endodontically treated teeth: An update. J Prosthet Dent. 1988;59(5):553-558.
18. Buttel L, Krastl G, Lorch H, et al. Influence of post fit and post length on fracture resistance. Int Endodon J. 2009; 42:47-53.
19. Sorensen JA, Engelman MJ. Ferrule design and fracture resistance of endodontically treated teeth. J Prosthet Dent. 1990;63(5):529-536.
About the Authors
Christine M. Yonker, DDS
Oral Rehabilitation
Center, P.C.
Skokie, Illinois
Sergio Rubinstein, DDS
Oral Rehabilitation
Center, P.C.
Skokie, Illinois
Alan J. Nidetz, DDS
Oral Rehabilitation
Center, P.C.
Skokie, Illinois




 www.sybronendo.com
www.sybronendo.com

 www.bisco.com
www.bisco.com




 www.pearsondental.com
www.pearsondental.com


