BioHorizons Laser-Lok® Microchannels
Scientific research to clinical reality for crestal bone and soft tissue stability.
By Cary A. Shapoff, DDS
Dental implant placement and restoration have become commonplace to treat compromised teeth and edentulous sites in the partially edentulous patient. The goals of dental implant procedures have evolved from replacement of missing or damaged teeth to esthetic replicas of natural teeth with long-term stability. Stability of the dental implant restoration is defined by long-term retention of the implant fixture in the alveolar bone as well as stability of the crestal bone supporting the marginal gingiva and interproximal papillae. Previous articles have reported on the average tissue heights and soft tissue dimensions associated with teeth, dental implants, and pontic sites adjacent to teeth or implants.1,2 The significance of these dimensions requires long-term stability of the bone-soft tissue complex to maintain esthetic results.
Implant companies have modified dental implant surfaces from smooth metal to roughened surfaces to achieve a higher percentage of bone-to-implant contact and maintain crestal bone.3 Dimensional crestal bone loss changes regarded as “normal” after 1 year of restoration have been reported to be 1.5 mm to 2 mm with less than 0.1 mm of additional loss each subsequent year.4-6 Roughened textures on dental implants are random surfaces that increase surface area for bone attachment but have little to no influence on soft tissue. Previously published articles have described the soft tissue “attachment” (connection) to dental implant surfaces as epithelial hemidesmosomal or light attachment with parallel and circular arrangements of connective tissue fibers.7
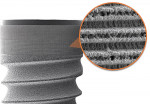
Organized roughened surfaces of specific dimensions have been developed to selectively influence fibroblast and osteoblast activity and growth patterns through contact guidance.8 These 8-µm to 12-µm grooves (Laser-Lok® microchannels, BioHorizons, www.biohorizons.com) are designed to provide a functional attachment surface for both bone and connective tissue (Figure 1 and Figure 2). This nano feature topography also directly affects the rate and amount of osteogenesis.9,10 The goal of this microengineered design is to provide long-term crestal bone and soft tissue stability. Figure 3 demonstrates the 11-year follow-up radiographic appearance of the first Laser-Lok implant.
Crestal bone loss, especially in the esthetically demanding anterior region, can result in loss of interdental bone, loss of papilla height, and open interproximal embrasures. Loss of marginal bone on facial surfaces can lead to gingival recession and possible exposure of crown margins. A variety of theories of crestal bone remodeling have been discussed in the literature. The formation of a natural biologic width, the microgap concept at the abutment–implant interface and excessive stress, and strain at the alveolar crest have been reported to explain the crestal bone loss (“bone die-back”) commonly seen with dental implants after restorative loading.11
Recommendations for placement of two or more adjacent dental implants in the anterior region have also been described.12 A previous study13 noted a vertical bone loss extending 1.4 mm laterally on adjacent implants, resulting in the loss of interproximal bone height if implants were positioned closer than 3 mm apart. Others have recommended implant placement distances relative to natural teeth,14 as the dental implant could adversely influence bone on the adjacent natural tooth. The crestal bone height on the natural tooth has a direct effect on the height of the interproximal papilla, which has significant implications in the “esthetic zone.”
The ability of Laser-Lok microchannels to limit crestal bone loss has been reported in numerous clinical studies and case reports.15-17 Nevins et al18 has shown perpendicular fibroblast attachment and impeded epithelial downgrowth on the implant collar in histological specimens of a series of patients treated with Laser-Lok implants. In a recent animal study using Laser-Lok microchannels placed on a restorative abutment, Nevins19 reported similar histological results with perpendicular fibroblast attachment and blocked epithelial downgrowth on the abutment surface above the implant–abutment interface.
Unlike other implant systems, this functional soft tissue attachment to the implant collar allows for a variety of platform placement positions at the time of surgery. Often the alveolar ridge height is different on mesial-to-distal surfaces and facial-to-palatal surfaces. All BioHorizons dental implants with the Laser-Lok collar design allow for a transitional placement of slightly supracrestal to crestal positioning. Supracrestal placement of a portion of the collar allows for soft tissue functional attachment to the microchannels, thereby protecting the crestal bone in a similar concept to the connective tissue attachment of a natural tooth.
The following case examples demonstrate the ability of BioHorizons’ Laser-Lok technology to provide long-term bone and soft tissue stability in regions of narrow bone, adjacent dental implants in the esthetically demanding anterior regions, and reconstructed severely damaged extraction sockets and periodontally compromised sites.
Case 1
In this case, shown in Figure 4, Figure 5, Figure 6, a 17-year old girl presented for consideration of dental implants to replace congenitally missing lateral incisors. Her medical history revealed no contraindications to dental implant surgery. Prior orthodontic care had created adequate mesial-to-distal coronal space and adequate root parallelism of adjacent teeth. She initially presented with a thin biotype and excessive gingival display (altered passive eruption). A preliminary esthetic crown-lengthening procedure involving flap reflection and crestal osseous surgery was performed in the maxillary arch to position the gingival at the proper anatomical position. The existing alveolar ridge appeared clinically narrow, not uncommon with congenitally missing teeth, from incomplete ridge expansion associated with permanent tooth eruption. Three-dimensional radiographic imaging was performed to determine the exact buccolingual ridge dimension and flare necessary for presurgical treatment planning and proper implant tri-dimensional positioning. A BioHorizons Laser-Lok Tapered Internal (3.5-mm platform) was placed after obtaining proper depth with the surgical drills and ridge expansion procedures to the predetermined position using a restoratively designed surgical guide.
Case 2
Figure 7, Figure 8, Figure 9 shows a 44-year-old woman who was referred for dental implant consideration on tooth No. 26 after diagnosis of external root resorption and periapical abscess. All other adjacent teeth were in good periodontal health. A preliminary phase of extraction and socket grafting using MinerOss® allograft (cortical and cancellous bone allograft, BioHorizons) was allowed to heal for 4 months prior to dental implant surgery. A BioHorizons Laser-Lok 3-mm dental implant was placed and allowed to heal for 3 months before second-stage surgery and provisionalization. The permanent crown was completed after 8 weeks of soft tissue maturation with the provisional restoration.
Case 3
A 69-year old man presented for dental implant consultation after the extraction of teeth Nos. 9 through 10 without ridge preservation procedures 4 months earlier (Figure 10). Significant horizontal alveolar resorption and loss of the bony facial plate was clinically evident. A simultaneous implant surgical procedure with bone augmentation was performed as both implants could be positioned 3 mm to 4 mm behind the facial contour of the existing alveolar housing.
Case 4
In the last case, shown in Figure 11, Figure 12, Figure 13, Figure 14, Figure 15, a 47-year-old man was referred for dental implant consideration after the horizontal fracture of teeth Nos. 9 and 10. These teeth had undergone prior endodontic therapy and post placement. Periapical radiolucencies were noted on both teeth and a hopeless prognosis was assigned to each tooth. A delayed implant placement approach was planned with extraction of both teeth and socket grafting with MinerOss® allograft. Four months after grafting, dental implants were placed through a flapless approach using a soft tissue punch of matching implant diameter. Implant positioning and platform positioning was determined by use of a restoratively designed surgical guide with anticipated proper crown height. The platform was positioned 3 mm apical to the ideal gingival margin of the intended crown restorations.
Conclusion
The author’s long-term clinical experience with dental implants designed with Laser-Lok microchannels has demonstrated exceptional bone stability. The restorative colleagues who provided the prosthetic support have remarked about the excellent tissue health around the implants. The author’s periodic re-evaluation of clinical cases has demonstrated shallow sulcular depth and excellent soft-tissue health. The stability of crestal bone has been noted in immediate extraction cases, grafted sites, and single-tooth restorations, as well as multiple adjacent implants. It is the author’s opinion that the reality of bone and soft-tissue stability has been achieved in a private practice setting with a wide variety of clinical situations.
Acknowledgment
The author would like to thank Mr. Boyd Peters, BioHorizons' vice president of marketing, dental implants, for editorial support and the use of corporate product images. Additionally, the author is grateful to the following clinicians for their contributions:
Figure 3. Restoration by Dr. Jeffrey Babushkin, Trumbull, CT
Figures 4-6. Restoration by Dr. Perry Kest, Southbury, CT
Figures 8-15. Restorations by Dr. David Wohl, Fairfield, CT
Disclosure
Dr. Cary A. Shapoff provides clinical consulting services to BioHorizons and has been paid an honorarium for corporate-sponsored lectures that he presents. He has also received material support for writing this article.
References
1. Salama H, Salama MA, Garber D, Adar P. The interproximal height of bone: A guidepost to predictable aesthetic strategies and soft tissue contours in anterior tooth replacement. Practical Periodontics Aesthet Dent. 1998;10:1131-1141.
2. Tarnow D, Elian N, Fletcher P, et al. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol. 2003;74:1785-1788.
3. Cochran DL. A comparison of endosseous dental implant surfaces. J Periodontol. 1999;70:1523-1539.
4. Smith DC, Zarb GA. Criteria for success of osseointegrated endosseous implants. J Prosthet Dent. 1989;62:567-572.
5. Albrektsson T, Zarb GA, Worthington P, et al. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:1-25.
6. Roos J, Sennerby L, Lekholm U, et al. A qualitative and quantitative method for evaluating implant success: a 5-year retrospective analysis of the Brånemark implant. Int J Oral Maxillofac Implants. 1997;504-514.
7. Berglundh T, Lindhe J, Ericsson I, et al. the soft tissue barrier at implants and teeth. Clin Oral Implants Res. 1991;2:81-90.
8. Ricci JL, Grew JC, Alexander H. Connective-tissue responses to defined biomaterial surfaces. I. Growth of rat fibroblast and bone marrow cell colonies on microgrooved substrates. J Biomed Mater Res A. 2008;85A:313-325.
9. Valencia S, Gretzer C, Cooper LF. Surface nanofeature effects on titanium-adherent human mesenchymal stem cells. Int J Oral Maxillofac Implants. 2009;24:38-46.
10. Zinger O, Zhao G, Schwartz Z, et al. Differential regulation of osteoblasts by substrate microstructural features. Biomaterials. 2005;26:1837-1847.
11. Oh T-J, Yoon J, Misch CE, et al. The causes of early implant bone loss: myth or science. J Periodontol. 2002;73:322-333.
12. Tarnow DP, Elian N. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol. 2003;74:1785-1788.
13. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71:546-549.
14. Choquet V, Hermans M, Andriaenssens P, et al. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001;72:1364-1371.
15. Pecora GE, Ceccarelli R, Bonelli M, et al. Clinical evaluation of laser microtexturing for soft tissue and bone attachment to dental implants. Implant Dent. 2009;18:57-66.
16. Weiner S, Simon J, Ehrenberg DS, et al. The effects of laser microtextured collars upon crestal bone levels of dental implants. Implant Dent. 2008;17:217-228.
17. Shapoff CA, Lahey B, Wasserlauf PA, Kim D. Radiographic analysis of crestal bone levels around Laser-Lok® collar dental implants. Int J Periodontics Restorative Dent. 2010;30:129-137.
18. Nevins M, Nevins ML, Camelo M, et al. Human histologic evidence of a connective tissue attachment to a dental implant. Int J Periodontics Restorative Dent. 2008;28:111-121.
19. Nevins M, Kim DM, Jun SH, et al. Histologic evidence of a connective tissue attachment to laser microgrooved abutments: A canine study. Int J Periodontics Restorative Dent. 2010;30:245-255.
About the Author
Cary A. Shapoff, DDS
Private Practice Limited to Periodontics—Dental Implant Surgery
Fairfield, Connecticut