Surgical Endodontics
A conservative alternative for endodontic treatment.
This title may seem to somewhat of a misnomer at first glance. Can apical surgery really be a conservative means of treatment?1 Should it be performed only after initial root canal therapy has failed or only after re-treatment has failed to produce a desirable result? To better answer this, we need to explore the literature, and view solutions to problems from other perspectives.
The literature suggests that a patient experiences "little pain and moderate swelling after apical surgery." 2 Nevertheless, apical surgery often has negative connotations associated with it. This is partially related to early studies that often questioned the long-term success rate of apical surgery.3 In the past, failure was largely due to one of three reasons: poor vision, prior to the microscope being introduced; larger preparations with round burs, prior to ultrasonics being introduced; and amalgam being utilized as the retroseal material of choice, before ProRoot MTA® (DENTSPLY Tulsa, https://www.tulsadental.com) was introduced. Endodontists who perform surgery with a microscope and ultrasonic retro-preparations produce outcomes that achieve results equal to non-surgical root canal therapy or re-treatment.4 Tsesis et al demonstrated a surgical success rate of 91.6%, an uncertain healing rate of 3.7%, and a failure rate of only 4.7%.5 Kim et al further corroborated these findings when they revealed that the successful outcome for isolated endodontic lesions was 95.2% after apical surgery.6
It has been established that apical surgery can be highly successful, so when should it be recommended as a treatment of choice? For patients with iatrogenic problems (ie, separated instruments, ledges, post perforations, transported canals, etc), surgery is often the treatment of choice. This logic, however, implies that a tooth's restorative condition is really what is at the heart of the matter. To further illustrate this point, cases are presented where surgery was recommended both prior to and after non-surgical root canal treatment.
Case 1
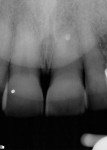
A 60-year-old patient presented with a low-grade ache on tooth No. 9. The medical history was positive for type II diabetes, which was controlled with glucophage. The chief complaint was that he felt "discomfort" whenever he bit down on his front teeth, tooth No. 9 in particular. His occlusion was excellent, and he reported having no dental treatment in the last several years aside from routine scaling and root planing. There was evidence of some tiny irritation, redness, and minute swelling at the facial-gingival margin of tooth No. 9 (Figure 1).
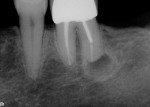
Teeth Nos. 7, 8, and 10 responded normally to cold while tooth No. 9 did not respond. All teeth tested negative with the bite stick, percussion, and palpation. There was no mobility and no significant periodontal probing depths. The patient reported no history of trauma, yet radiographic evaluation revealed no visible canal in tooth No. 9 (Figure 2). There was a periapical radiolucency, and it was noted that tooth No. 9 was shorter than tooth No. 8. Diagnosis was determined to be a necrotic pulp in tooth No. 9 with chronic peri-radicular periodontitis.
Conventional wisdom says a necrotic, intact tooth with little mobility or probing depth should have non-surgical endodontic treatment to remove the source of infection. But in this case, the author determined that greater damage could result because of the likelihood that the canal was calcified. As a result, a surgical approach was recommended and agreed upon by the patient.
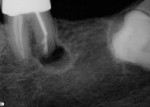
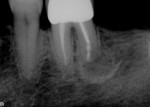
A sulcular full-thickness flap was used to visualize any coronal defects (ie, dehiscence, cracks) that may have existed and contributed to the patient's redness and tiny swelling at the gingival margin. At the apex, a microscopic canal was visualized. However, it was so small that even the microscopic endodontic explorer could not penetrate the canal. A 3-mm ultrasonic retro-preparation was achieved, using a diamond-coated tip, and the tooth was retrosealed with gray ProRoot MTA (Figure 3). The sutures were removed 1 week later. A 2.5-year check-up revealed evidence of bone regeneration (Figure 4).
Case 2
What began as a routine case slowly became more complex. A 72-year-old woman with no remarkable medical history presented with pain and a slight facial swelling adjacent to tooth No. 6. Radiographic analysis demonstrated a well-circumscribed radiolucency at the apex of tooth No. 6 (Figure 5). The patient had a 10-year-old six-unit bridge spanning teeth Nos. 2 through 7. Teeth Nos. 3 through 5 were pontics.
Cold testing with Hygenic® Endo- Ice® (Coltene-Whaledent, https://www.coltene.com) revealed no response to teeth Nos. 6, 7, or 8. Tooth No. 8 responded positively to vitality testing with a Vitality Scanner 2006 (Sybron Endo, https://www.sybronendo.com). Only tooth No. 6 was positive to percussion. Both teeth Nos. 6 and 7 were palpation positive, but tooth No. 6 was more painful. A 5-mm probing on the mesiofacial surface of tooth No. 7 was noted. It is important to point out that every tooth in need of a root canal, surgical or non-surgical, should be probed circumferentially and the findings recorded. Large probings can often be indicative of a fracture or periodontal disease. Periodontal defects may determine the design of the flap being considered for surgery.
The diagnosis for tooth No. 6 was a necrotic pulp with chronic peri-radicular periodontitis and an acute abscess, which was an exacerbation of a chronic infection. The patient was also told that tooth No. 7 was probably necrotic and would require future treatment, but treating tooth No. 6 was most prudent because it was the source of her acute pain. With the patient's informed consent, root canal therapy was initiated on tooth No. 6. Patency was established and pus drained for almost 5 minutes from within the canal. Irrigation consisted of 30 ml 6% NaOCl throughout the procedure via EndoVac® (Discus Dental, https://www.discusdental.com) and ultrasonic activation. Studies have shown that ultrasonic activation is more effective at eliminating bacteria than passive irrigation.7 Similarly, with its negative apical pressure, EndoVac has been demonstrated to significantly improve canal debridement at 1 mm from working length when compared to passive irrigation.8 The canal was medicated with calcium hydroxide. The tooth was sealed with cotton and Cavit™ (3M ESPE, https://www.3mespe.com).
The patient returned 2 weeks later, pain free and without any noticeable swelling. Root canal therapy was completed and the tooth was sealed with gutta-percha via warm vertical condensation using a resin sealer, and the access cavity was sealed with a composite restoration (Figure 6). The patient remained symptom-free for more than 3 months. At that point, she returned with even greater pain than her initial visit. Swelling was pronounced, extending into the canine space and beginning to close her eye. Tooth No. 7 was significantly positive to percussion and palpation. Tooth No. 7 was determined to be necrotic with acute abscess.
However, herein lies the difference in the treatment approach to tooth No. 7; it demonstrated significant coronal calcification. Rather than risk making an access opening that might compromise the abutment value or perforate the tooth, it was determined that apical surgery would be a less invasive, more conservative solution. It would be less invasive because the goal was not to further weaken the two anterior abutments already anchoring a large-span bridge.
The patient gave written informed consent for apical surgery on teeth Nos. 6 and 7. A sulcular full-thickness flap was raised, demonstrating only a small amount of bone loss on the buccal surface of tooth No. 6. Upon enlarging the opening to access the lesion, it was apparent that it involved both teeth. In fact, tooth No. 7 actually had more bone destruction. This is important to mention because, radiographically, only tooth No. 6 demonstrated any visible radiolucency. This finding was in agreement with Bender and Seltzer's analysis that "early stages of bone disease cannot be detected by means of routine roentgenograms, nor can the size of a rarefied area on the roentgenogram be correlated with the amount of tissue destruction." 9
After apicoectomies were performed on both teeth, the entire lesion was curetted and submitted for biopsy. It should be noted that whenever tissue is removed from the body, it is prudent to send the sample to an oral pathologist for examination. White ProRoot MTA was placed as a retroseal in both teeth and the flap was closed with 5.0 Ethibond (Ethicon, https://www.ethicon.com) sutures. After 4 days, the sutures were removed.
In the author's opinion, MTA is a good material of choice for surgery because it has been recognized to be bioactive, hard-tissue conductive, and biocompatible, and it seals the root end.10-12 Figure 7, Figure 8, Figure 9 demonstrate the size of the area affected, along with the postoperative evidence that retro-preparations were placed in both teeth. Figure 10 illustrates bone healing at the 1.5-year mark.
Case 3
This case involved a 60-year-old woman who presented with pain on chewing in tooth No. 19. The tooth had been treated endodontically 8 years previously, and this was the first time the patient had begun to experience any significant pain. Radiographic analysis demonstrated a well-circumscribed radiolucency at the apex of the distal root of tooth No. 19 (Figure 11). Teeth Nos. 17, 18, and 21 were missing and had been replaced with a removable partial denture. Endodontic testing revealed that teeth Nos. 20 and 22 were positive, non-lingering to Endo-Ice, while tooth No. 19 did not respond. Only tooth No. 19 was positive for percussion, palpation, and bite-stick. Diagnosis was determined to be a pulpless tooth No. 19 with chronic peri-radicular periodontitis with symptoms.
Because the tooth anchored her partial denture, the patient wanted to retain it. Non-surgical re-treatment, apical surgery, extraction, and no treatment were all offered to her as treatment choices. Because the obturated distal canal was not centered, it was deduced that failure was likely due to an untreated second distal canal. Re-treatment would have likely been the best treatment alternative. Because she did not want to have her crown compromised in any way, apical surgery was determined to be the treatment of choice.
After the patient gave written informed formed consent, local anesthesia was administered using one carpule of 3% mepivacaine and one carpule of 2% lidocaine with epinephrine 1:100,000 via inferior alveolar and long buccal injections. A sulcular full-thickness flap was elevated and an osteotomy was performed to expose the distal root of tooth No. 19. After tissue removal, the non-treated distal-buccal canal was clearly visible and an apical isthmus was present. Meanwhile, the excised tissue sample was submitted for biopsy. After minimal tooth resection, bevel, and ultrasonic retro-preparation (again with a diamond-coated tip), both canals and an isthmus were sealed with white ProRoot MTA. Figure 12, Figure 13, Figure 14 demonstrate the two retro-preparations along with the adjoining isthmus postoperatively. At the 6-month check-up, there was already complete radiographic bone regeneration (Figure 15).
Interestingly, all three biopsies were determined to be granulomas. This is important to note because many people erroneously believe they can make that diagnosis by looking at a radiograph. Numerous studies, however, have demonstrated that radiographs are not sufficient to determine diagnosis of peri-radicular lesions.13 More recent studies have shown that even cone-beam computed tomography is not capable of doing this.14 Also worthy to note is that some radiolucencies may be true cysts. While they can occur as frequently as 8.6% of the time, they often cannot be eliminated by non-surgical endodontic therapy, and may require surgical intervention.15
Conclusion
Although endodontists and general dentists alike are used to treating necrotic teeth by non-surgical root canal therapy, this is not always the best method of treatment. While it still is the most desirable method, these three cases demonstrate that clinicians must use their prudent judgment to determine what will benefit the patient the most in order to better preserve their teeth. These cases demonstrate that apical surgery can often be more definitive, less invasive, and more conservative than non-surgical root canal treatment or non-surgical re-treatment.
Disclosure
The author lectures for and has received honoraria from Discus Dental.
References
1. Chivian N. Surgical endodontics: a conservative approach. Journal of the New Jersey Dental Society. 1969;40(6):234-244.
2. Christiansen R, Kirkevang LL, Horsted-Bindslev P, Wenzel A. Patient discomfort following apical surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 105(2):245-250.
3. Frank A, Glick D, Patterson S, Weine F. Long-term evaluation of surgically placed amalgam fillings. J Endod. 1992;18(8):391-398.
4. Rubenstein RA, Kim S. Long-term follow-up of cases considered healed one year after apical microsurgery. J Endod. 2002;28(5):378-383.
5. Tsesis I, Faivishevsky V, Kfir A, Rosen E. Outcome of surgical endodontic treatment performed by a modern technique: A meta-analysis of literature. J Endod. 2009; 35(11):1505-1511.
6. Kim E, Song J, Jung I, et al. Prospective clinical study evaluating endodontic microsurgery outcomes for cases with lesions of endodontic origin compared with cases with lesions of combined periodontal-endodontic origin. J Endod. 2008;34(5):546-551.
7. Spoleti P, Siragusa M, Spoleti MJ. Bacteriological evaluation of passive ultrasonic activation. J Endod. 2003; 29(1):12-14.
8. Nielsen BA, Baumgartner J. Comparison of the Endo Vac system to needle irrigation of root canals. J Endod. 2007;33(5):611-615.
9. Bender IB, Seltzer S. Roentgenographic and direct observation of experimental lesions in bone: II. J Endod. 2003;29(11):707-712.
10. Enkel B, Dupas C, Armengol V, et al. Bioactive materials in endodontics. Expert Rev Med Devices. 2008;5(4):475-494.
11. Moretton TR, Brown CE Jr, Legan JJ, Kafrawy AH. Tissue reactions after subcutaneous and intraosseous implantation of mineral trioxide aggregate and ethoxybenzoic acid cement. J Biomed Material Research. 2000; 52(3):528-533.
12. Torabinejad M, Chivian N. Clinical applications of mineral trioxide aggregate. J Endod. 1999;25(3):197-205.
13. Drouin RD, Mascres C. [Granuloma or cyst? The unknown chronic periapical lesion.] J Dent Que. 1989;26:547-551.
14. Rosenberg PA, Frisbie J, Lee J, et al. Evaluation of pathologists (histopathology) and radiologists (cone beam computed tomography) differentiating radicular cysts from granulomas. J Endod. 2010;36(3):
423-428.
15. Simon J. Incidence of periapical cysts in relation to the root canal. J Endod. 1980; 6(11):845-848.
About the Author
Joseph D. Chikvashvili, DDS
Private Practice
West Orange, New Jersey
Director of Endodontics
Newark Beth Israel
Medical Center
Newark, New Jersey