Using the STA Single Tooth Anesthesia System™ Unit
John L. Santopolo, DDS, MScD
An intraligamentary injection technique for definitive diagnosis in an endodontic case.
Computer-controlled local anesthetic delivery systems were introduced to the dental profession in 1997.1,2 This new technology allowed fluid pressure and the solution flow rate at the needle tip to be controlled and monitored during the injection procedure.3 Dynamic pressure-sensing technology works to decrease the pressure needed to introduce the anesthetic into the tissues and the flow rate control allows more anesthetic to be introduced into the tissues. This new technology enables the dentist to give an easier, less painful dental injection.
The classic periodontal ligament (PDL) injection technology was described by Fischer.4 It might be better understood as an intraosseous injection using the PDL as a conduit to the bone. The technique involves the placement of a 30-gauge dental needle into the gingival sulcus followed by advancing the needle into the PDL between the root surface and the tooth socket.5,6 This technique is usually held in reserve by most dental practitioners to be used when their standard anesthetic techniques do not yield deep enough anesthesia to make the procedure comfortable. The reasons that many clinicians are reticent to use a PDL injection are twofold. The first is the pain associated with the injection procedure itself. The second is the damage from trauma to the bone caused by the high pressure needed to give this injection.7,8
Benefits
The term “PDL injection” has negative connotations for most dental practitioners. As stated above, it is normally held in reserve as an injection that has to be used because the previous injections have not produced the desired anesthetic effect. Although the traditional PDL injection takes seconds to give and the small amount of anesthesia given under high pressure is effective immediately, the postoperative discomfort and the pain of the injection make the dental practitioner leery of its use. In this author’s opinion, the STA System Intraligamentary Injection Technique (Milestone Scientific, www.milestonescientific.com) has accentuated all of the positives of the old PDL technique while removing the negatives. The STA System delivers more anesthetic under less pressure, ergo a longer duration of anesthesia is achieved with no tissue damage or bone resorption. The fact that there is less trauma to the PDL results in very comfortable injections with less post-injection discomfort. Because the STA System Intraligamentary Injection does not cause any pain or discomfort, the patient is less anxious. Because the patient’s anxiety level does not increase during the STA System injection, the administration of the injection is much less stressful for the dentist.
Technique
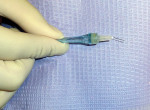
The author suggests that the clinician snap the handpiece off to make it shorter. This allows easier access to the injection site on the maxillary, but it allows easier access especially on the mandibular teeth (Figure 1). While keeping the STA System machine in the STA mode, locate the injection sites. The disto–buccal line angle and then the mesial–buccal line angle are the injection sites on the maxillary teeth. The injection sites for the mandibular teeth are the distal–lingual line angle and then the mesial–lingual line angle, finishing with the buccal furcation on the molars. The clinician should always start with the distal site on all teeth. Bend the needle approximately 10º to 15º toward the bevel and insert the needle into the PDL with the bevel of the needle placed toward the tooth. Keep this position during the entire injection. Set the machine on cruise control and administer the anesthetic at the control flow rate. Move the needle deeper into the sulcus until resistance is met. Hold the STA System handpiece in place for 15 seconds while listening for the audible tones and light signals that indicate the needle is in the PDL space. When the correct injection site has been reached, administer one quarter of a carpule of 4% articaine (1:200,000). After the correct amount of anesthesia has been injected, wait 6 seconds and slowly back out the needle. Complete the injection sequence. Once the sequence is completed, the tooth should be anesthetized pulpally and on the buccal and lingual.
Important Considerations
This technique can be used as a substitute for infiltration of a mandibular block injection technique. It will take more time to give the STA System PDL injection, but the onset of anesthesia is fast, and may potentially save some chairtime. During the injection, do not rotate the needle. Keep the bevel facing the tooth and maintain a steady needle position. Never force the needle into the PDL. A gradual injection into the sulcus that results in a slow pressure increase is optimal. The dynamic pressure sensing system will identify the correct needle position and alert the user with both an audible tone and a yellow/green LED display.
Case History
The patient was referred to the author’s office complaining of pain on exposure to hot and cold on the upper right side. She could not identify the offending tooth. While she was giving her written medical and dental history, the author’s receptionist noted that she was constantly sipping cold water.
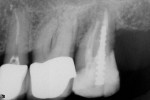
Her clinical examination showed porcelain-fused-to-metal crowns in place on teeth Nos. 3 through 5 and a core in place on tooth No. 2. Examination of the margins showed a possible opening on the mesial of tooth No. 4. A radiographic examination revealed root canal treatment had been completed on teeth Nos. 2 and 5, ruling out these teeth as a cause of pain to thermal changes. The patient’s stated specific complaint was pain on exposure to a hot cup of coffee that cold water relieved. She could not identify a specific tooth as the source of the problem.
Before the author began to use the STA System PDL injection for diagnostic purposes, he would have used a cavity test to help him determine the offending tooth, then milled through the porcelain with diamonds and a water spray and cut through the gold thimble to gain access to the natural tooth. He would have then placed a heat carrier in the opening and warmed up the tooth. If the application of heat on that tooth duplicated the patient’s complaint of pain, and if following the heat with cold controlled the pain, then a diagnosis was reached. However, if the author had chosen incorrectly and picked the tooth that was the normal of the two, he would have to access the second tooth in the same fashion and repeat the tests hoping to duplicate the patient’s complaint on the next tooth.
This method of diagnosis, although proven, has some problems inherent in its performance. First, all the milling and drilling is done without the benefit of anesthesia for obvious reasons. Naturally, patients are anxious about the use of the drill in their mouth without anesthesia. Duplicating the symptoms is uncomfortable for the patient and “playing with the pain” can produce anxiety. Drilling through a porcelain crown can produce anxiety for the dentist. Not only is the dentist concerned because he or she is making the patient anxious, but the dentist is risking a fracture of the porcelain on each crown that is test drilled.
Using this diagnosis by exclusion with the intraligamentary injection leaves a lot of anxiety behind. Once it is established that hot liquid generates the pain, the clinician can rule out a single tooth at a time. In this case, the author started with tooth No. 4. After he administered the PDL injection and waited a reasonable amount of time, he gave the patient more hot water. No pain was generated. He repeated this twice, as a way to demonstrate to the patient that the offending tooth had been “numbed” and, therefore, the generation of pain had been stopped. The diagnosis was made and the tooth was ready to be treated (Figure 2, Figure 3, Figure 4). The author believes diagnosis by anesthetic exclusion using the STA System Injection Technique will gain in popularity as practitioners become more comfortable with the STA system and techniques.
Disclosure
The author owns shares in Milestone Scientific and has been reimbursed for his lecturing expenses by the company.
References
1. Hochman M, Chiarello D, Hochman CB, et al. Computerized local anesthesia delivery vs traditional syringe technique. NY State Dent J. 1997;63:24-29.
2. Friedman MJ, Hochman MN. A 21st century computerized injection system for local pain control. Compend Contin Educ Dent. 1997;18:995-1003.
3. Hochman M, inventor. Pressure/force computer controlled drug delivery system. Assigned: Milestone Scientific, Inc. US Patent 6,200,289. March 2001.
4. Fischer G. Local Anesthesia in Dentistry. 4th ed. Philadelphia: Lea & Febiger; 1933.
5. Malamed SF. The periodontal ligament (PDL) injection: an alternative to inferior alveolar nerve block. Oral Surg Oral Med Oral Path. 1982;53:117-121.
6. Dreyer WP, van Heerden JD, de V Joubert JJ. The route of periodontal ligament injection of local anesthetic solution. J Endo. 1983; 9:471-474.
7. White JJ, Reader AL, Beck M, et al. The periodontal ligament injection: a comparison of the efficacy in human maxillary and mandibular teeth. J Endod. 1988;14:508-514.
8. Malamed SF. Handbook of Local Anesthesia. 4th ed. St Louis Mosby: 1997.
About the Author
John L. Santopolo, DDS, MScD<
Private Practice
Woodmere, New York