Infiltration of Fluid Resins Without Cutting Into Primary And Permanent Teeth in Children
By Joel H. Berg, DDS, MS; James Dunn, DDS
Caries is defined as biofilm-initiated and saliva-mediated acid demineralization of enamel and dentin.1 Caries is a process, yet many often fail to remember that it is a process that occurs over time. This process starts at the surface of the lesion (or slightly subsurface in some instances) progresses toward cavitation, and then causes possible further destruction of the tooth.
Indeed, many think of caries in terms of the results of the process—a cavity formed in the tooth—rather than in terms of the process itself. Yet, much occurs many months before a cavity (if not years, in some instances) that could lead to the progression of a caries lesion. Caries lesions often progress faster in children because of the lower mineral content in primary teeth and also because of children’s diet. The risk factors and circumstances leading to the progression of caries lesions in children is often more complex and more intense than it is in permanent teeth and in adults; therefore, progression can be rapid.
Regardless of whether the teeth are primary or permanent or the patient is a child or an adult, one can describe the caries process as a sort of continuum; on one end there is early surface demineralization and on the other there is complete cavitation with significant loss of tooth structure. Between these two extremes is subsurface demineralization that is not detectable by many of the clinical detection methods currently available. There has been rapid development of “early caries detection” devices, and soon there will be even better ways of detecting the caries lesions that are the most treatable at the earliest stages—those which now are only visible microscopically in extracted teeth. The next stage of caries progression involves demineralization of the tooth, which can be visualized clinically or radiographically, yet is not complete enough to the extent that most clinicians would place a restoration to correct the defect.
There is a circumstance along the caries process continuum in which very early lesions are often treated with remineralization techniques. Many clinicians will apply various forms of fluoride to interproximal areas where a caries lesion is present but detectable only approximately halfway through the enamel on a radiograph. These lesions are often noted in the chart as “watch” lesions; that is, the clinician waits to see if they progress on subsequent radiographs. Although this technique of watching may seem crude because the radiograph is a very insensitive device for the detection of caries lesions, it is still preferred over cutting into the tooth and subjecting the patient to a lifetime of restorative procedures. Whenever possible, it is always better to preserve tooth structure than to cut it. That is the objective of the remineralization technique.
However, by the time a bitewing radiograph shows that a caries lesion has progressed halfway through the enamel, the lesion might already have extended well into the dentin and perhaps even started to progress occlusally, incisally, and gingivally, even though this progression is not radiographically detectable. Therefore, the idea of remineralizing such lesions may not be clinically feasible. Yet, there is no consistent process or procedure that allows a large enough “middle zone” on the treatment continuum for the lesions that are watched (or perhaps even cut unnecessarily) in advance of needing a restoration. Very likely, most practitioners have a large group of patients in their practices with one or more lesions that they are “watching” to see if—and, in many cases, when—they will progress. The ability to preserve lesions in a state where they will not progress would certainly be preferable, although they may still be detectable radiographically, and only when they become too large or too advanced to be treated with remineralization techniques using fluoride or other remineralizing agents would they have to be invasively restored.
A technique using a surface erosion technique combined with resin infiltration has recently been developed. This technique allows the infusion of a combination of low-viscosity, unfilled resins that can penetrate the enamel surface of the tooth all the way to the dentinoenamel junction and slightly beyond, in some instances.
In a variety of in vitro and in vivo studies, Meyer-Lueckel and others have shown that the infiltration technique works very well in both primary and permanent teeth. In one study, they demonstrated the effect of 15% hydrochloric acid vs 37% phosphoric acid in allowing the surface to be etched and eroded sufficiently to subsequently allow penetration of the resin.2 The study results showed that there was an effective reduction in the surface depth from natural enamel caries when the 15% hydrochloric acid was applied for between 90 and 120 seconds.3 Using hydrochloric acid instead of phosphoric acid has allowed for the infiltration technique to be used. The researchers went on to develop additional aspects of the technique, and subsequently showed that two applications of the resin material influenced penetration depth, completeness, as well as the surface hardness of the infiltrated restoration.3
One in vitro study4 demonstrated that by infiltrating caries lesions that were beyond the remineralization stage there was an inhibition of further demineral a likelihood that infiltrated clinical lesions would be protected, would not progress further, and would be resistant to further acid demineralization4; in fact, they might even be strengthened by virtue of such resin penetration. Further studies characterized various resins and combinations of resins as well as the timing of hydrochloric acid application, and developed the technique to the point where it is now a commercial product.5-8
This product was launched in early 2009 in Europe, and will be available in the United States and many other countries later in the year. Several studies published by Meyer-Lueckel and Paris, as well as others, have shown a halting of lesion progression, sealing of the surface, and effective stabilization of caries lesions at what was previously the “watched” stage. This gave much promise to the idea of clinical procedures being successful in the large segment of lesions along the caries continuum that progress to being cavitated as they are being “watched.”9,10
Additional work has examined the differences between primary and permanent teeth, and such work has shown that, similarly, the hydrochloric acid-etching of the surface—together with the combination of fluid resins—can penetrate enamel all the way to the dentinoenamel junction, allowing lesions that have been infiltrated with this resin to stabilize, thus avoiding progression to the cavitation stage.10-12These lesions were resistant to demineralization, as was the case when the permanent teeth were treated. There are several in vivo studies currently underway; the results will likely be published sometime this year. Early findings, disseminated through personal communication from the studies’ authors, reveal that infiltration with this combination of resins, using the technique described, have allowed an arrest of lesion progression, compared with the control group, in which lesions were not infiltrated and a significantly higher number progressed to cavitation. This appropriate comparison should encourage clinicians to be comfortable in the knowledge that caries progression would have occurred if the lesions were not infiltrated, and that indeed it was generally halted, at least initially, in cases in which infiltration was performed.
Clinical Cases
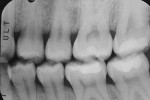
The authors report on two cases where they applied the infiltration (Icon, DMG, Hamburg, Germany) technique in interproximal situations. The first is in a premolar, with infiltration treating the distal aspect of the permanent tooth. Figure 1 shows tooth No. 13 in the arch of a 17-year-old female patient. Upon radiographic examination, the distal aspect could be visualized (Figure 2). There was a lesion which, on theradiograph, had progressed halfway through theenamel. Most clinicianswould not consider this to be a lesion capableof remineralization given the extent of the progression. Figure 3 shows the lesion/tooth isolated under the rubber dam. A good rubberdam is necessary to protect the tooth and toobtain adequate moisture control duringthe procedure. Figure 4 shows the tooth being wedged with the special wedges provided in the unit-dose kit. Figure 5 demonstrates theplacement of a specialized matrix that is included in the infiltration kit. This matrix shows the hydrochloric acid gel being exuded fromthe orifices within the matrix (allowing access to the proximal surface via wedging), placement of the acid and, later, the resin, which affects the approximal surface,allowing these agents to flow only onto the proximal surface under consideration for the procedure. This resin is placed after the area isdried using an ethanol solution. It is essential to have complete desiccation within the areato be infiltrated sothat the infiltrate can flow appropriately, through capillary action, into the surface all the way to the dentinoenamel junction. Figure 6 shows theproximal after rinsing the hydrochloric acid anddrying, with a new matrix placed, through whichthe resin material flows. The resin material isflossed to obtain a smooth surface (Figure 7). This is repeated a second time to obtain proper filling. The patient is thendischarged with a“note card” contained in the kit documenting the procedure, so that it will be known by the patient/parent or another dentist later on that the lesion was infiltrated. The material is not radiopaque; therefore, it may be not discernible on a radiograph at subsequent visits. Documentation in the chart needs to adequately record that the infiltration procedure was performed to allow further evaluation of the lesion and todetermine that the lesion has not progressed.
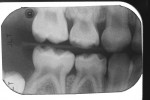
The second case involved both proximal surfaces of primary tooth T in a 5-year-old patient. This patient was cooperative but anxious, so mild sedation with nitrous oxide was employed. Infiltration was performed on both the mesial and distal proximal aspects of tooth S. The radiograph (Figure 8) shows that both the mesial and distal aspects had caries lesions that had progressed approximately halfway through the enamel. In fact, in the mesial aspect, although there was some surface cavitation, the lesion had only progressed halfway through the enamel. The distal had a more typical cone-shaped lesion that also penetrated halfway through the enamel depth. The tooth was isolated under a rubber dam (Figure 9). The tooth was then wedged on both proximal aspects (Figure 10), and matrices were placed on both the mesial and distal aspects. This could have been done simultaneously, but in this instance the authors chose to separate the procedure for photographic purposes and visualization. There was some oozing of saliva and blood, but this was limited to the distal aspect of the canine, not on the mesial aspect of the first primary molar where the infiltration and the etchant would be exuded. The infiltration material was flowed into the mesial aspect of the first primary molar (Figure 11). Floss was used to obtain a smooth surface before light-curing (Figure 12). The resin was then light-cured, and the patient went home with a satisfactory restoration that was infiltrated without cutting.
Discussion
The infiltration technique is indeed a revolution in restorativedentistry for children and adults. In the case of children, parents wouldprefer that the tooth not be cut unnecessarily, establishing a cycle of continuous replacement of restorations, because of the natural limited lifespanof a restoration. If one can place arestoration that will halt progression of thelesion without cutting the tooth, it iscertainly preferable to cutting the tooth in any way. The infiltration technique, supported by currently undergoing clinical studies, is auseful tool in the armamentarium of therestorative dentist for children. Although further studies will confirm the long-term benefits, initial workpublished over the last several years, as well as results of ongoing clinical studies, indicate thatthis technique is a viable option on the restorative dentistry “continuum” for children. With the rapid progress of caries lesions in children, the clinician can now choose to “infiltrate” interproximal caries lesions rather than cut the teeth or simply “watch” the lesion progress to thepoint of cavitation.
Disclosure
Dr. Berg is a current consultant for DMG America.
References
1. American Academy of Pediatric Dentistry.Definition of Early Childhood Caries. Available at: www.aapd.org. 2007.
2. Meyer-Lueckel H, Paris S, Kielbassa AM. Surface layer erosion of natural caries lesions with phosphoric and hydrochloric acid gels in preparation for resin infiltration. Caries Res.2007;41(3): 223-230.
3. Paris S, Meyer-Lueckel H. Influence of application frequency of an infiltrant on enamel lesions. J Dent Res. 2008;87(Spec Iss B):1585.
4. Mueller J, Meyer-Lueckel H, Paris S, et al. Inhibition of lesion progression by the penetration of resins in vitro: influence of the application procedure. Oper Dent. 2006; 31(3):338-345.
5. Paris S, Meyer-Lueckel H, Kielbassa AM. Resin infiltration of natural caries lesions. J Dent Res.2007;86(7): 662-666.
6. Paris S, Meyer-Lueckel H, Mueller J, et al. Progression of sealed initial bovine enamel lesions under demineralizing conditions in vitro. Caries Res. 2006;40(2):124-129.
7. Meyer-Lueckel H, Paris S, Kielbassa AM. Einfluss verschiedener Ätzgele auf den Mineralgehalt initialer Schmelzläsionen von Michzähnen. Dtsch Zahnärztl Z. 2007; 62(11 Supplement):D16.
8. Paris S, Meyer-Lueckel H, Stiebritz M, Kielbassa AM. Surface layer erosion of enamel caries lesions in primary teeth in preparation for resin infiltration. Caries Res.2007;41(2):268-334.
9. Ekstrand KE, Bakhandeh A. Versiegelung approximaler Kariesläsionen an Milchzähnen bei Kindern. Data on file. DMG Hamburg, Germany.
10. Paris S, Meyer-Lueckel H. Radiographic comparison of lesion progression after infiltration and standard therapy—in vivo—18 months follow-up. Data on file. DMG Hamburg, Germany. Scientific documentation p 27.
11. Martignon S, Meyer-Lueckel H, Tellez M, Paris S. Radiographic comparison of lesion progression after infiltration, sealing and floss instructions in a high caries risk population—12 months follow up. Data on file. DMG Hamburg, Germany. Scientific documentation p 28.
12. Ekstrand KR, Bakshandeh A. Radiographic comparison of lesion progression after infiltration, sealing and floss instructions in a high caries risk population—6 and 12 months clinical follow up. Data on file. DMG Hamburg, Germany. Scientific documentation p 30.
About the Authors
Lloyd and Kay Chapman
Chair for Oral Health
Department of Pediatric Dentistry
The University of Washington School of Dentistry
Seattle, Washington
James Dunn, DDS
Private Practice
Auburn, California