Custom Abutments Alone Will Not Eliminate the Clinical Effects of Poor Cementation Techniques Around Dental Implants
Abstract:
With proper planning, placement, prosthetic treatment, and maintenance, dental implants have been shown to be a predictable and reliable treatment option with a high success rate. Clinicians who place cement-retained implant restorations, however, should be aware of the potential and sometimes irreversible biological complications associated with residual excess cement and should be prepared to consider using different practices that may reduce the problem. The present case reports describe the use of custom abutments to restore deeply placed implants with the intent of minimizing residual excess cement.
Dental implants are considered a predictable and reliable treatment option for completely and partially edentulous situations. With proper planning, placement, prosthetic treatment, and maintenance, dental implants can attain reported success rates of 97% to 99%.1,2 Dental implant crown cementation is common for a variety of reasons, including: improved esthetics; implant angulation correction; control of occlusion; less demanding implant placement; cost (components and laboratory); improved passive fit for multiple connected units; and similarity to conventional tooth-supported fixed prosthodontics.3
Cement-retained implant restorations, nevertheless, do have the potential for complications that could negatively affect their outcome. Peri-implant health is a major contributor to the success criteria of dental implants. A multicenter study reported greater peri-implant health surrounding screw-retained restorations when compared to cement-retained restorations after 5 years.4 Numerous case reports have associated residual excess cement (REC) with peri-implant disease.5-7 Wilson8 associated REC with 81% of cases exhibiting signs and symptoms of peri-implant disease. Once the cement was detected with the aid of a dental endoscope, its removal resulted in an improvement in the signs and symptoms of 76% of the cases. While the average time until the biologic complication of peri-implant disease was seen was at 3 years, failure rates in the literature greatly diminish after the first year.8
Deep subgingival cement margins have been associated with residual cement and peri-implant inflammation.9,10 To avoid these complications in deep gingival sulcus or irregular tissue contours around an implant, the use of custom abutments or screw retention has been recommended.11 Using a custom abutment could theoretically decrease the prevalence of REC complications by controlling the depth of the restorative margins. While this is the goal of treatment using custom abutments, improper design or execution still may lead to peri-implant complications. The case reports presented here demonstrate problems that may occur despite the use of custom abutments and subsequent complications associated with REC.
Case 1
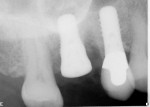
A healthy 70-year-old woman with increasingly deep pockets and furcation involvement of her upper right first molar was referred to a periodontist by her general dentist. Following evaluation and consultation, it was determined that the tooth was non-salvageable12 and required extraction and replacement with an implant-supported crown (Figure 1).
After obtaining informed consent, the patient returned for surgical treatment. She was premedicated with 2 grams of amoxicillin. In a single visit, the tooth was extracted and an osteotome sinus augmentation and implant placement were performed, as was socket grafting, using a combination of autogenous bone and freeze-dried bone allograft (FDBA).13 A Straumann® SLActive Wide Neck (WN) 4.8-mm x 10-mm Tapered Effect (TE) implant (Straumann, www.straumann.us) was placed with a 3-mm transmucosal healing abutment (Straumann). After approximately 4 months of uneventful healing, the implant was restored by the patient’s prosthodontist using a stock Straumann 5.5-mm WN solid abutment and a polycarboxylate-cement–retained ceramo-metal crown (Figure 2).
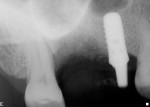
Approximately 1 year after implant placement, the patient returned to the periodontist for evaluation of 10-mm to 12-mm pockets around the mesial and palatal surfaces of the implant (Figure 3), an indication of the presence of an advanced peri-implantitis lesion.14 During surgical debridement of the area, large amounts of subgingival cement were found on the palatal surface of the implant, which was associated with 6 mm to 8 mm of bone loss extending from the mesio-palatal to the disto-palatal line angles. There was little involvement of the proximal or buccal surfaces. The area was debrided and the implant was treated with saturated citric acid for 1 minute, followed by grafting with FDBA and Emdogain™ (Straumann). Healing appeared to proceed uneventfully; however, due to the patient’s traveling schedule, only one follow-up with the periodontist was possible.
Approximately 9 months following the repair procedure, the patient was again referred back for evaluation of bleeding and suppurating pockets of 9 mm to 10 mm on the mesial and palatal of implant No. 3. In consultation with the patient and a new restorative dentist, it was determined that the repair procedure had failed and removal of the implant was necessary. Implant removal was performed after undermining the integrated implant surfaces with a high-speed bur and copious irrigation in conjunction with counter-rotation with extraction forceps. Grafting of the defect was accomplished using an allograft putty (Regenaform®, Exactech Inc., www.exac.com) reconstituted with venous blood beneath a collagen barrier (Bio-Gide®, Geistlich Pharma North America, Inc., www.geistlich-na.com). The buccal flap was advanced to obtain primary closure (Figure 4). Since the patient did not want to be “toothless,” the ceramo-metal crown on No. 4 was removed, and a cantilever provisional on Nos. 3 and 4 was cemented.
Four months later, a new Straumann SLActive surface WN10 Standard Plus (SP) implant was placed into the grafted site. The flaps were apically positioned to compensate for the previous coronal positioning, and an autogenous palatal connective tissue graft was placed to augment deficient buccal contours (Figure 5).
After an uneventful healing period, the patient returned to her new restorative dentist for fabrication of her new crown on No. 3 and replacement of the original crown on No. 4. This time, the new crown on No. 3 was fabricated using a screw-retained custom cast abutment underneath a cemented ceramo-metal crown.
Upon the patient returning to the periodontist for routine supportive care 6 months after cementation of the new crown, pockets of 5 mm to 6 mm were noted circumferentially around the implant, with significant bleeding on probing and a buccal fistula (Figure 6). A periapical radiograph revealed a large subgingival cement deposit on the mesial (Figure 7). A treatment recommendation was made to remove the crown and abutment for thorough cleaning and to ensure there was no remaining residual cement.
The patient returned and was anesthetized with local anesthetic. The crown was removed using pliers (GC Pliers, GC America Inc., www.gcamerica.com) and abrasive powder to improve the grip on the ceramic, and the abutment was then unscrewed, revealing a large amount of adherent material—presumably cement—circumferentially around the abutment (Figure 8 and Figure 9). Additionally, cement particles were removed from the transmucosal collar of the implant and the surrounding sulcular area. The abutment was cleaned mechanically and ultrasonically with cement remover and repolished, then re-placed in the implant with a seating torque of 35 Ncm. The crown was carefully recemented with polycarboxylate cement (Durelon™, 3M ESPE, www.3MESPE.com) to verify complete cement removal.
One year later, the patient was seen for routine periodontal supportive treatment, and a new periapical radiograph was taken (Figure 10). At this visit, there were no clinical signs of inflammation around the implant and no radiographic evidence of bone loss or excess cement.
Case 2
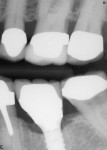
A healthy 63-year-old woman who smoked a half pack of cigarettes per day was referred for extraction and replacement of a fractured tooth No. 19. Surgery performed included extraction, placement of a Straumann SP SLActive WN implant, and grafting of the mesial socket with autogenous bone chips and anorganic bovine bone (BioOss®, Geistlich) without loading (Figure 11). Healing proceeded uneventfully, and the implant was restored 4 months later by the patient’s restorative dentist with a custom cast abutment under a ceramo-metal crown. The patient returned to the periodontist for annual follow-up, at which time it was noted that she had erythematous and edematous gingiva surrounding the implant, with suppuration and pockets measuring 8 mm on the direct facial (Figure 12). Radiographs taken to evaluate the condition showed relatively normal bone levels on the implant with nothing unusual about the restoration (Figure 13).
The crown was removed with a crown remover (GC Pliers) and the abutment was unscrewed from the implant (Figure 14). The abutment had a thick coating of material, presumably cement, extending into the surrounding gingival sulcus (Figure 15 and Figure 16). After mechanically removing the material from the abutment and then cleaning it ultrasonically, the abutment was re-placed in the implant and retorqued to 35 Ncm. The ceramo-metal crown was then carefully recemented (Durelon). Follow-up examination showed spontaneous resolution of inflammation and restoration of sulcus depth of 3 mm to 4 mm circumferentially.
Case 3
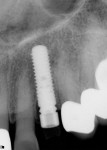
A healthy 76-year-old woman with a history of penicillin allergy was referred to a periodontist for replacement of her upper left canine, which had fractured at the alveolar crest and was deemed nonrestorable. In a single appointment, the tooth was extracted and a Straumann SLActive Bone Level (BL) implant was placed with
> 50 Ncm insertion torque stability towards the palatal of the socket.
A temporary abutment was contoured to resemble a tooth preparation, and an acrylic provisional restoration was cemented as an immediate replacement for the extracted tooth. The buccal gap was grafted with a slurry of autogenous bone chips and anorganic bovine bone (Bio-Oss) (Figure 17). After 3 months of uneventful healing (Figure 18), the patient was referred back to her restorative dentist for final restoration.
Thirteen months following implant placement and 9 months after final restoration with a milled zirconia abutment and cemented ceramic crown, the patient returned to the periodontist complaining of vague discomfort and occasional bleeding from the tissue around the implant. Pocket depths of 5 mm to 6 mm with bleeding on probing were noticed, as was evidenced by 2 mm of radiographic crestal bone loss (Figure 19 and Figure 20). Although the radiograph did not suggest the presence of cement, it was believed that some residual luting material was clinically detectable in the pockets surrounding the crown. (Note: Although no radiograph was taken at the time of implant placement, the 2 mm of bone loss refers to a comparison to the time of final healing when the patient was released back to the restorative dentist for final restoration. While the authors acknowledge that this is not absolute proof that the bone loss occurred following final restoration, they believe it is strong circumferential evidence.)
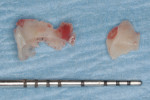
After administration of local anesthetic, a full-thickness flap was raised to gain access to the implant at the abutment/restorative interface (Figure 21), which revealed a significant amount of hard, easily dislodged material consistent with excess resin cement (Figure 22). This material even had the impression of the exterior bevel of the implant as well as the abutment on its inner surface. After carefully removing the cement and associated granulation tissue, a 3-mm to 4-mm circumferential bony defect was observed (Figure 23). The implant was cleaned with saturated citric acid and the flaps replaced. After healing, 1 mm to 2 mm of recession was noted, but the inflammation resolved.
Discussion
The use of custom abutments has been proposed to help eliminate the negative effects of REC by raising the restorative margin in the sulcus, thus facilitating cement clean-up. These case reports describe the use of custom abutments that follow the contours of the gingival margins to create more ideal restorations. Even though the intentions in abutment design and restoration fabrication were good, the cementation techniques were flawed. Other factors may influence the successful prevention of cement extrusion past the abutment margins, as well as the ease of detection and clean-up. These include: type of cement, cementation techniques, abutment design, and depth of abutment margins.
Type of Cement
A survey conducted of US dental schools by Tarica described many different types of cements used for cement-retained implant restorations.15 These included zinc oxide eugenol, resin-modified glass ionomer, zinc phosphate, conventional glass ionomer, polycarboxylate, acrylic urethane, and resin-based cements. All of these cements have different characteristics, features, and components such as flow properties, viscosities, and dimensional stability. Flow properties and film thicknesses differ depending on several variables, including dispensing and mixing techniques. There are also differences in the radiographic characteristics of these cements.
The detection of REC may be facilitated if it can be identified radiographically. There are no radiopacity standards that exist for restorative luting agents. This is different from other materials. For example, endodontic sealers have an ISO standard stating that any sealer used for endodontic purposes must be equivalent or greater to the radiopacity of 3 mm of aluminum.16 Two studies have described the large differences in the radiopacity of commonly used cements in implant dentistry.17,18 In both studies, the most radiopaque cements contained zinc, which is found in zinc phosphate, zinc oxide eugenol, and polycarboxylate cements. However, some polycarboxylate cements may be contraindicated with titanium abutments due to the potential for removal of the oxide layer of titanium and subsequent susceptibility to corrosion.19 No information exists as to whether this phenomenon is relevant to non-titanium abutments, as is seen in Case 1 above where a gold alloy was used for the abutment material. It is also unknown if corrosion of a supragingival abutment has any effect on osseointegration.
The type of cement will also influence the removal of the REC. Agar reported that the removal of zinc phosphate from titanium surfaces was more predictable when compared to glass ionomer and resin cements.20 The resin cement was the most difficult to remove. The difficulty associated with removing these materials may be associated with the high retentive forces associated with resin cements.21
Cementation Technique
No universal protocol is used for cementation techniques of tooth-supported restorations. This may be due to the rare complication of REC surrounding the natural dentition. The increase in reports of complications regarding implants emphasizes the need for a better understanding of these procedures. While there are no clear guidelines for dealing with cementation of implant-retained restorations, there is also little information on cement loading and the amount of cement required for ideal cementation. Most manufacturers’ instructions give subjective descriptions—for example: “Use a thin layer of cement”—which are subject to interpretation by the user.
A recent publication described different cement-loading techniques used by clinicians for implant-retained crowns.22 Participants in the qualitative and quantitative survey were provided with crown forms and instructed through an audiovisual presentation to proportion, mix, and load the cement into the intaglio of the crown form. The cement lute space is the area provided for cement within the interface of the crown and the abutment. This space is typically created in the dental laboratory with the use of a die spacer during the crown fabrication process. Therefore, any quantity of cement placed within the crown that exceeds the cement lute space must be extruded out of the crown and abutment for complete seating. The quantity of cement required to be ideal would equal the thickness of the die spacer. The weight of cement necessary for ideal cementation was calculated for this survey; it averaged 13.6 mg cement weight. The cement weight of test samples varied from 3.2 mg to 506.4 mg. The authors described a large variability in the cement quantities used, which indicates a lack of uniformity and precision in cement application techniques. There is no consensus in the dental community as to the appropriate quantity of cement and placement method for an implant crown form.
Multiple techniques to help reduce the amount of cement extrusion at the time of the cementation procedure have been published.23,24 These publications describe techniques that use copy abutments to extrude cement extraorally. It is not common practice with traditional tooth-form dentistry to use a copy abutment to control cement volumes used prior to seating, and to date, no surveys have been found to corroborate the use of such devices in clinical implant practice.
Other publications have described the advantages of making modifications to the abutment or to the crown that will decrease the amount of REC at the time of the cementation procedure.25,26 These modifications include venting the crown and allowing cement excess to flow through the vent instead of the abutment margin. The abutment may also be vented, allowing excess cement to flow within the hollow screw-access chamber. These modifications have limitations and could be contraindicated if ceramic abutments or crowns are used.
Abutment Design
One of the advantages of using a custom abutment is the ability to customize the contour and shape in the subgingival area. This allows the restoration to have an emergence that more closely resembles a natural tooth. Most stock abutments cannot achieve this subgingival form, and an unnatural contour or shape will be produced at the junction of the abutment and the restoration. This will oftentimes form a ledge, undercut, concavity, or convexity that will limit the access available for debridement and instrumentation, forming a cement trap. A custom abutment should mimic the form of the natural tooth that it is replacing. The crown restoration should have the same dimensions as the abutment in order to prevent an unnatural junction.
If the implant is not placed in an ideal position bucco-lingually, mesio-distally, or apico-coronally, the resulting restoration will nearly always have an unnatural contour. A more lingual placement may create an over-contoured buccal dimension, forming a trap for cement. This is also influenced by the diameter of the implant. When a smaller-diameter implant is used to replace a large tooth like a molar, the formation of unnatural contours and a subsequent cement trap can be expected. Screw-retained restorations, by definition, cannot lead to these cement traps and should be considered in these situations.
Depth of Abutment Margins
Confusion exists as to where the abutment margin should be placed in reference to the gingival margin. Raising the cement margins by using custom abutments helps reduce the tissue depth to the margin, but a 2011 study by Linkevicius et al9 found that implant crown margins placed any distance subgingivally will result in increased frequency of REC. Many custom abutments are fabricated using different CAD/CAM designs, which have a built-in default setting controlling the abutment margin depth. Most of these systems place the facial abutment margins 1 mm subgingivally. In an in-vivo study, Linkevicius et al10 (2013) described a significant increase in the amount of REC found in peri-implant tissues when comparing abutment margins that were equigingival to abutment margins that were located 1 mm subgingivally. Therefore, the default positioning of the abutment margins 1 mm subgingivally associated with CAD/CAM-fabricated custom abutments may be problematic and should be evaluated further. It may be necessary to fabricate abutment margins supragingivally to facilitate detection and clean-up and to minimize subgingival REC.27
Conclusion
The present case reports describe the use of custom abutments to restore deeply placed implants. The irreversible damage caused by the extrusion of REC past the abutment margins, lack of detection, and failure to clean is substantial and unconscionable. Excellent crestal bone stability has been confirmed for many implant systems, with and without grafting procedures28-30 when restorative procedures are appropriately completed. Clinicians should be aware of the potential and sometimes irreversible biological complications associated with REC and should be prepared to consider using different practices that may reduce the problem. The use of a custom abutment to raise restorative margins alone may not be sufficient to minimize these complications. A clear understanding of abutment design, cementation techniques, cementation quantities, cement materials, REC detection, and cement removal is recommended. These procedures are all important factors associated with successful treatment; therefore, they should not be delegated to auxiliary staff. Cementation should be given the same importance and detail as implantation in order to achieve optimal results.
ABOUT THE AUTHORS
Alfonso Piñeyro, DDS
Part-time Affiliate Instructor, Department of Restorative Dentistry, University of Washington School of Dentistry, Seattle, Washington; Private Practice, Seattle, Washington
Jeffrey Ganeles, DMD
Assistant Clinical Professor, Nova Southeastern University College of Dental Medicine, Ft. Lauderdale, Florida; Assistant Clinical Professor, Boston University Goldman School of Graduate Dentistry, Boston, Massachusetts; Private Practice with Florida Center for Periodontics & Implant Dentistry, PA, Boca Raton, Florida
REFERENCES
1. Lindquist LW, Carlsson GE, Jemt T. A prospective 15-year follow-up study of mandibular fixed prostheses supported by osseointegrated implants. Clinical results and marginal bone loss. Clin Oral Implants Res. 1996;7(4):329-336.
2. Ekelund JA, Lindquist LW, Carlsson GE, Jemt T. Implant treatment in the edentulous mandible: a prospective study on Brånemark system implants over more than 20 years. Int J Prosthodont. 2003;16(6):602-608.
3. Hebel KS, Gajjar RC. Cement-retained versus screw-retained implant restorations: achieving optimal occlusion and esthetics in implant dentistry. J Prosthet Dent. 1997;77(1):28-35.
4. Sherif S, Susarla SM, Hwang JW, et al. Clinician- and patient-reported long-term evaluation of screw- and cement-retained implant
restorations: a 5-year prospective study. Clin Oral Investig. 2011;15
(6):993-999.
5. Pauletto N, Lahiffe BJ, Walton JN. Complications associated with excess cement around crowns on osseointegrated implants: a clinical report. Int J Oral Maxillofac Implants. 1999;14(6):865-868.
6. Gapski R, Neugeboren N, Pomeranz AZ, Reissner MW. Endosseous implant failure influenced by crown cementation: a clinical case report. Int J Oral Maxillofac Implants. 2008;23(5):943-946.
7. Callan DP, Cobb CM. Excess cement and peri-implant disease. Journal of Implant and Advanced Clinical Dentistry. 2009;1(6):61-68.
8. Wilson TG Jr. The positive relationship between excess cement and peri-implant disease: a prospective clinical endoscopic study. J Periodontol. 2009;80(9):1388-1392.
9. Linkevicius T, Vindasiute E, Puisys A, et al. The influence of margin location on the amount of undetected cement excess after delivery of cement-retained implant restorations. Clin Oral Implants Res. 2011;22(12):1379-1384.
10. Linkevicius T, Vindasiute E, Puisys A, et al. The influence of the cementation margin position on the amount of undetected cement. A prospective clinical study. Clin Oral Implants Res. 2013;24(1):71-76.
11. Morton D, Martin WC, Ruskin JD. Single-stage Straumann dental implants in the aesthetic zone: considerations and treatment procedures. J Oral Maxillofac Surg. 2004;62(9 suppl 2):57-66.
12. Samet N, Jotkowitz A. Classification and prognosis evaluation of individual teeth-a comprehensive approach. Quintessence Int. 2009;40(5):377-387.
13. Fugazzotto PA, DePaoli S. Sinus floor augmentation at the time of maxillary molar extraction: success and failure rates of 137 implants in function for up to 3 years. J Periodontol. 2002;73(1):39-44.
14. Froum SJ, Rosen PS. A proposed classification for peri-implantitis. Int J Periodontics Restorative Dent. 2012;32(5):533-540.
15. Tarica DY, Alvarado VM, Truong ST. Survey of United States dental schools on cementation protocols for implant crown restorations. J Prosthet Dent. 2010;103(2):68-79.
16. ISO 6876:2001. Dental root sealing materials. Geneva, Switzerland: International Organization for Standardization.
17. Wadhwani C, Hess T, Faber T, et al. A descriptive study of the radiographic density of implant restorative cements. J Prosthet Dent. 2010;103(5):295-302.
18. Pette GA, Ganeles J, Norkin FJ. Radiographic appearance of commonly used cements in implant dentistry. Int J Periodontics Restorative Dent. 2013;33(1):61-68.
19. Wadwani CP, Piñeyro AF. Implant cementation: clinical problems and solutions. Dent Today. 2012;31(1):56-62.
20. Agar JR, Cameron SM, Hughbanks JC, Parker MH. Cement removal from restorations luted to titanium abutments with simulated subgingival margins. J Prosthet Dent. 1997;78(1):43-47.
21. Mansour A, Ercoli C, Graser G, et al. Comparative evaluation of casting retention using the ITI solid abutment with six cements. Clin Oral Implants Res. 2002;13(4):343-348.
22. Wadhwani C, Hess T, Piñeyro A, et al. Cement application techniques in luting implant-supported crowns: a quantitative and qualitative survey. Int J Oral Maxillofac Implants. 2012;27(4):859-864.
23. Wadhwani C, Piñeyro A. Technique for controlling the cement for an implant crown. J Prosthet Dent. 2009;102(1):57-58.
24. Dumbrigue HB, Abanomi AA, Cheng LL. Techniques to minimize excess luting agent in cement-retained implant restorations. J Prosthet Dent. 2002;87(1):112-114.
25. Wadhwani C, Piñeyro A, Hess T, et al. Effect of implant abutment modification on the extrusion of excess cement at the crown-abutment margin for cement-retained implant restorations. Int J Oral Maxillofac Implants. 2011;26(6):1241-1246.
26. Patel D, Invest JC, Tredwin CJ, et al. An analysis of the effect of a vent hole on excess cement expressed at the crown-abutment margin for cement-retained implant crowns. J Prosthodont. 2009;18(1):54-59.
27. Wadhwani CP, Piñeyro A, Akimoto K. An introduction to the implant crown with an esthetic adhesive margin (ICEAM). J Esthet Restor Dent. 2012;24(4):246-254.
28. Cordaro L, Torsello F, Chen S, et al. Implant supported single tooth restoration in the aesthetic zone: transmucosal and submerged healing provide similar outcome when simultaneous bone augmentation is needed. Clin Oral Implants Res. 2013;24(10):1130-1136.
29. Sanz M, Ivanoff CJ, Weingart D, et al. Clinical and radiological outcomes after submerged and transmucosal implant placement with two-piece implants in the anterior maxilla and mandible: 3-year results of a randomized controlled clinical trial. Clin Implant Dent Relat Res. 2013;doi:10.1111/cid.12107. [Epub ahead of print]
30. Albrektsson T, Buser D, Sennerby L. Crestal bone loss and oral implants. Clin Implant Dent Relat Res. 2012;14(6):783-791